What Imaging Studies Should Be Ordered To Help Establish The Diagnosis How Should The Results Be Interpreted
Doppler echocardiography transthoracic echocardiography is the main imaging modality used in HFPEF to establish the diagnosis by criteria exclude valvular, right-sided or pericardial disease and assess for other potential differential diagnoses. The following describes echocardiographic criteria recommended by the European Society of Cardiology for the diagnosis of HFPEF:
An LV ejection fraction of > /= 50% and LV end-diastolic volume index < 97 mL/m2 are used as cut-off values for normal or mildly abnormal LV systolic function. LV diastolic dysfunction can be demonstrated using Doppler echocardiography.
Raised LV filling pressure is indicated by a ratio of mitral early diastolic inflow velocity to mitral early annular lengthening velocity > 15. Additional echocardiographic parameters are useful as surrogate markers of LV diastolic dysfunction, if they exceeded specific cut-off values.
These parameters are useful when the E/e ratio is intermediate . They include left atrial volume , pulmonary venous flow velocity , mitral inflow Doppler and LV mass index .
Cardiac Catheterization
Invasive assessment of hemodynamic parameters by cardiac catheterization remains the gold standard for the diagnosis of HFPEF. Criteria for raised LV filling pressure include LV end-diastolic pressure > 16 mmHg or a mean pulmonary capillary wedge pressure > 12 mmHg.
Other
What Are The Stages Of Heart Failure
Heart failure is a chronic long-term condition that gets worse with time. There are four stages of heart failure . The stages range from “high risk of developing heart failure” to “advanced heart failure,” and provide treatment plans. Ask your healthcare provider what stage of heart failure you are in. These stages are different from the New York Heart Association clinical classifications of heart failure that reflect the severity of symptoms or functional limits due to heart failure.
As the condition gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. You cannot go backwards through the stages. For example, if you are in Stage B, you cannot be in Stage A again. The goal of treatment is to keep you from progressing through the stages or to slow down the progression.
Treatment at each stage of heart failure may involve changes to medications, lifestyle behaviors and cardiac devices. You can compare your treatment plan with those listed for each stage of heart failure. The treatments listed are based on current treatment guidelines. The table outlines a basic plan of care that may apply to you. If you have any questions about any part of your treatment plan, ask a member of your healthcare team.
Treatment And Prognosis Of Hfpef
Clinical trials in HFpEF have produced neutral results to date and treatment is largely directed toward associated conditions and symptoms . This approach is consistent with recommendations for treatment of patients with HFpEF included in the 2013 American College of Cardiology Foundation/American Heart Association HF guidelines . The following two strong recommendations were included: 1) Systolic and diastolic hypertension should be controlled in accordance with published clinical practice guidelines to prevent morbidity 2) Diuretics should be used to relieve symptoms due to volume overload. Similar recommendations were included in the 2016 European Society of Cardiology HF guidelines Developed with the special contribution of the Heart Failure Association of the ESC. Eur Heart J 2016 37: 21292200, doi: 10.1093/eurheartj/ehw128.).
Diastolic function worsens as part of aging even in individuals without other forms of cardiovascular disease . Asymptomatic diastolic dysfunction is a predictor of future cardiovascular morbidity, but prognosis differs from that in patients with symptoms of HFpEF (55. Borlaug BA, Redfield MM, Melenovsky V, Kane GC, Karon BL, Jacobsen SJ, et al. Longitudinal changes in left ventricular stiffness: a community-based study. Circ Heart Fail 2013 6: 944952, doi: 10.1161/CIRCHEARTFAILURE.113.000383.
You May Like: Ibs And Heart Palpitations
Obesity And Related Comorbidities
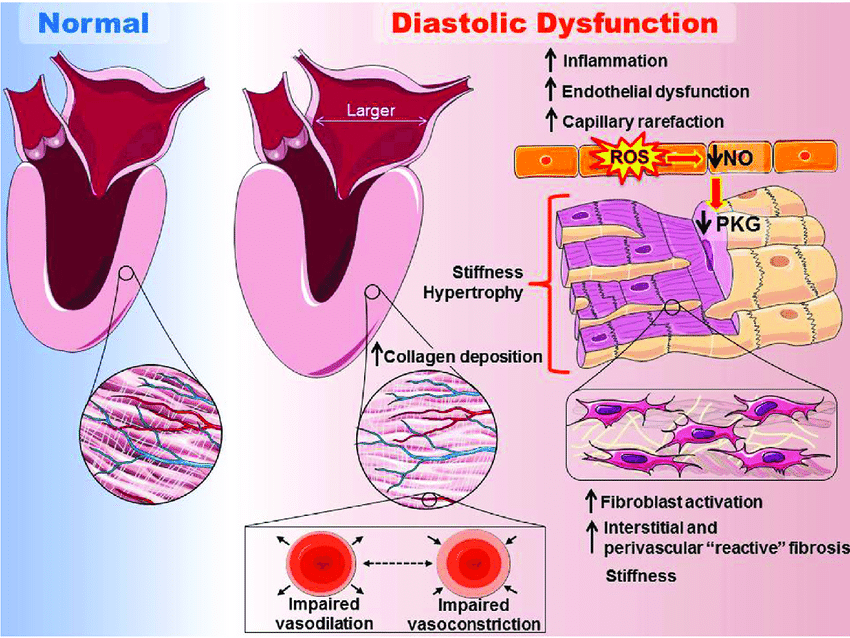
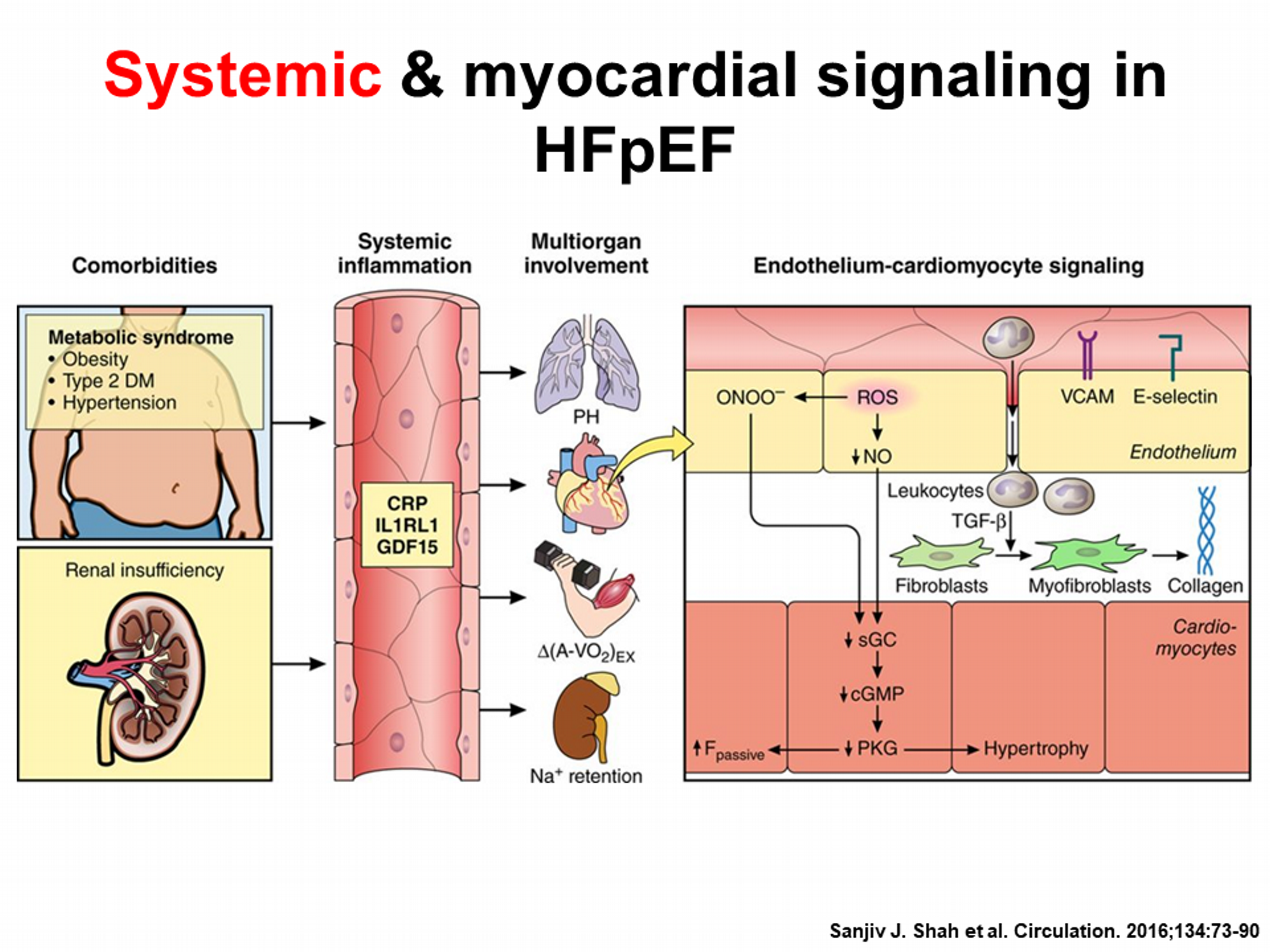
Aging seems to be the dominant risk factor for HFpEF. However, obesity and obesity-related comorbidities, such as metabolic syndrome, sedentary lifestyle, and hypertension, are also commonly observed and interact with aging to confer an increased risk of HFpEF . Symptoms in HFpEF patients were ascribed to comorbidities that are very frequent among HFpEF patients such as obesity, hypertension, and diabetes. Considering that obesity represents an incubator for other comorbidities , it is expected that more than 80% of HFpEF patients are overweight or obese . Earlier studies suggested that symptoms of dyspnea in obese patients were likely simply related to excess body mass, not cardiac abnormalities , but current disease paradigms have begun to embrace the importance of obesity in the pathophysiology of HFpEF, particularly as a cause of systemic inflammation, oxidative stress, and depressed nitric oxide availability that drive cardiac and extracardiac manifestations of disease . The increases in blood volume and thus cardiac loading in obesity may cause structural and functional alterations that contribute to HF .
What Is Preserved Ejection Fraction
- print page
- Bookmark for later
Ejection fraction measures the percentage of blood pumped out of the hearts left ventricle each time it beats. The left ventricle is a heart muscle that contracts and relaxes with every beat. Each time this happens the heart pumps blood throughout the body. This is the fundamental process of circulation.1
A normal heart does not completely fill or empty each time it beats. The ejection fraction is expressed as a percentage where the normal range is 55% to 70%.1 Sometimes people develop heart failure without any significant decrease in their ejection fraction noted. This is referred to as diastolic heart failure.1
Recommended Reading: Can Flonase Cause Heart Palpitations
Chronotropic Reserve And Autonomic Tone
Chronotropic incompetence, broadly defined as the inability of the heart to increase its rate according to increased activity or demand, is common in patients with cardiovascular disease, produces exercise intolerance, which impairs quality-of-life, and is an independent predictor of major adverse cardiovascular events and overall mortality . Chronotropic incompetence is extremely common in HFpEF, with reported prevalence of 57 to 77%. The chronotropic reserve is depressed in HFpEF even compared with older, age-matched controls and independent of rate-slowing medication use. Similar to HFrEF , this is likely related to downstream deficits in -adrenergic stimulation, because the increase in plasma catecholamines with exercise is identical in HFpEF and healthy controls . Cardiac output is equal to the product of stroke volume and heart rate, and the inability to augment heart rate with exercise, together with the known impairment in stroke volume reserve in HFpEF, significantly limits cardiac output responses to exercise in many patients . While chronotropic incompetence is common in HFpEF, there is no evidence at this time that rate-adaptive pacing is beneficial in patients with HFpEF .
A New The Hfapeff Diagnostic Algorithm: Hfpef Consensus Recommendation From The Heart Failure Association Of The European Society Of Cardiology
Recently, a new position paper from the Heart Failure Association was released, which offers an algorithm for diagnosing HFpEF HFA-PEFF, where P is a pre-test probability, E is a set of data from Echo and natriuretic peptides, F1-functional tests, in particular, diastolic stress test, F2-final conclusions on the aetiology of the pathological process.5 This document provides current clarifications on the features of the echocardiographic diagnosis of HFpEF. This algorithm has been validated in two independent, well-phenotyped cohorts and demonstrated that the HFA-PEFF score is helpful in clinical practice for the diagnosis of HFpEF.23
According to the proposed classification, all criteria, including echocardiographic, were divided into major and minor. The score has functional, morphological, and biomarker domains. Within each domain, a major criterion scores 2 points or a minor criterion 1 point.
Functional Domain
In subjects aged < 75 years: septal e´< 7 cm/s or lateral e´< 10 cm/s.
In subjects aged 75 years: septal e´< 5 cm/s or lateral e´< 7 cm/s.
Major criterion: average septallateral E/e´ ratio 15
Minor criterion: average septallateral E/e´ ratio 9 14
Morphological Domain
Major criterion: > 34mL/m2 for subjects in sinus rhythm
Major criterion: > 40mL/m2 for subjects in atrial fibrillation
You May Like: Why Do Av Nodal Cells Not Determine The Heart Rate
Atrial Fibrillation And Rate Control
Atrial fibrillation co-exists in approximately one-third of patients with HFpEF,44 and may precede or follow the development of heart failure.45 Patients with atrial fibrillation display elevated filling pressures and reduced cardiac output. The loss of atrial contraction in late diastole compounds the impaired left ventricular filling. As a result, the atrial myopathy promotes atrial fibrosis and higher transmission of left ventricular pressures onto the pulmonary circulation.46 In suitable candidates, rhythm control should be considered in view of the potential benefits, although trial data are lacking. If this fails, traditional management principles apply, with long-term rate control and anticoagulation. Catheter ablation appears safe, with similar functional improvements and rates of recurrence as in patients with HFrEF.47 Further studies are in progress.48
Rate control has also been suggested as a treatment target for patients in sinus rhythm to maximise diastolic filling. An increased heart rate is associated with cardiovascular death and hospitalisation in HFpEF,49 although pharmacological rate control has yet to show a mortality benefit.50,51 It may even be detrimental to the patients exercise capacity52 as it exacerbates their inability to compensate for exercise demands by inducing chronotropic incompetence.53 For this reason, adaptive atrial pacing has been suggested as an alternative to pharmacological rate control.54
Reduced Ejection Fraction And Preserved Ejection Fraction
One common way to classify heart failure is based on ejection fraction. The amount of blood pumped out of the heart with each beat is called the ejection fraction . A normal EF is usually around 55 to 70 percent, but it can be lessened in some forms of heart failure.1
People with heart failure with reduced ejection fraction have an EF that is 40 to 50 percent or lower. This is also called systolic heart failure. People with heart failure with preserved ejection fraction do not have much of a change in their ejection fraction. This is often called diastolic heart failure.1
Recommended Reading: Does Benadryl Increase Your Heart Rate
Citation Doi And Article Data
Citation:DOI:Dr Joachim FegerRevisions:see full revision historySystem:
- Heart failure with a preserved ejection fraction
- Diastolic dysfunction
- Cardiac failure with preserved ejection fraction
- Heart failure with preserved systolic function
- Heart failure with preserved ejection fraction
Heart failure with preserved ejection fraction is a type of heart failure with normal or near-normal ejection fraction and objective evidence of diastolic dysfunction.
What Laboratory Studies Should Be Ordered To Help Establish The Diagnosis How Should The Results Be Interpreted
Measurement of circulating B-type natriuretic peptide and N-terminal proBNP may assist in the diagnosis of HFPEF, since these cardiac neurohormones are released by cardiomyocytes in response to LV stretch from increased LV filling pressure. However, an elevated BNP or NT-proBNP on its own is insufficient for the diagnosis or exclusion of HFPEF.
Even in the absence of heart failure, levels of BNP or NT-proBNP increases with age, and are higher in women than men. BNP and NT-proBNP levels are also influenced by conditions, such as renal or hepatic impairment, and sepsis.
Notable cases where patients with HFPEF may display a falsely low BNP or NT-proBNP level include obese patients and patients with flash pulmonary edema. In general, levels of natriuretic peptides during an episode of decompensation are substantially higher in the HFREF compared to the HFPEF population.
This is likely related to the presence of LVH in many of the HFPEF patients and absence of LV dilatation, both of which tend to lower the level of wall stress in the LV. The presence of obesity may further alter the diagnostic accuracy of the natriuretic peptides since levels tend to be reduced as the extent of obesity increases.
Standard labs should also be performed to assess cardiovascular risk factors, measure renal function, exclude differential diagnoses, and look for comorbidities .
You May Like: Does Benadryl Raise Heart Rate
Rv Dysfunction And Pulmonary Vascular Disease
Roughly 70 to 80% of patients with HFpEF display pulmonary hypertension . As left atrial and pulmonary venous pressures increase due to diastolic dysfunction, this increases the pulmonary artery pressure through passive back-transmission of this hydrostatic pressure. With more advanced stages of HFpEF, there may also be changes in pulmonary vascular structure and function leading to a “precapillary” component where pulmonary vascular resistance increases . In patients with HFpEF, each 10-mmHg increment in pulmonary artery pressure is associated with a 28% increase in 3-year mortality . The chronic obstructive pulmonary disease commonly coexists with HFpEF, can worsen pulmonary hypertension, and also makes determining whether symptoms of dyspnea are primarily related to the heart or lungs . The presence of pulmonary hypertension in HFpEF is associated with adverse outcomes, including increased mortality and HF hospitalization rates . Reducing pulmonary artery pressure through diuretic use decreases HF hospitalizations in HFpEF , but other trials testing PH-specific therapies in HFpEF have failed to show a convincing benefit .
Stages C And D With Preserved Ef
Treatment for patients with Stage C and Stage D heart failure and reserved EF includes:
- Treatments listed in Stages A and B.
- Medications for the treatment of medical conditions that can cause heart failure or make the condition worse, such as atrial fibrillation, high blood pressure, diabetes, obesity, coronary artery disease, chronic lung disease, high cholesterol and kidney disease.
- Diuretic to reduce or relieve symptoms.
YOU ARE THE MOST IMPORTANT PART OF YOUR TREATMENT PLAN!
It is up to you to take steps to improve your heart health. Take your medications as instructed, follow a low-sodium diet, stay active or become physically active, take notice of sudden changes in your weight, live a healthy lifestyle, keep your follow-up appointments, and track your symptoms. Talk to your healthcare team about questions or concerns you have about your medications, lifestyle changes or any other part of your treatment plan.
Read Also: Does Benadryl Lower Heart Rate
Lifestyle Interventions In Hfpef
Recent data support the beneficial impacts of lifestyle modification, including weight reduction, dietary and nutrient consumption, physical activity, and cardiorespiratory fitness on HF risk. In a pooled analysis of 51000 participants from the Women’s Health Initiative, Multiethnic Study of Atherosclerosis, and Cardiovascular Health Study cohorts, the risk for incident HFpEF increased in a dosedependent manner as BMI increased and leisuretime physical activity declined. Recently, Kitzman et al showed that among older obese patients with chronic, stable HFpEF, intentional weight loss via calorie restriction diet significantly improved exercise capacity to a degree similar to and was additive to exercise training . In addition, CR but not exercise significantly improved the HF specific quality of life measures . Even though, a recent metaanalysis of randomized trials among older patients without HF indicates that CR is associated with a 15% reduction in total mortality, because of the reported HF obesity paradox, further studies are needed to determine role of CR in older patients with HFpEF.
Is There A Cure For Hfpef
HFpEF is a progressive condition with no cure, but its progression can be slowed or halted in many people through aggressive treatment and lifestyle changes. In most people, heart failure is a chronic condition that requires lifelong treatment.
Most treatments are geared toward slowing down the progression of your heart failure and managing your symptoms.
Your doctor will likely suggest that you follow a treatment regimen that includes a combination of:
- Diet and lifestyle changes
- Sometimes a device to protect your heart from abnormal rhythms
If you have heart failure, the following lifestyle changes will help manage your symptoms:
- Regular low-intensity aerobic exercise to strengthen the heart
- Eating a heart-healthy diet
- Cutting back on salt
- Limiting your alcohol consumption
- Quitting smoking
The best way to manage diastolic heart failure is to treat its underlying cause, such as hypertension, diabetes, or coronary artery disease.
The efficacy of medication in the treatment of diastolic heart failure is inconclusive, but diuretics and beta-blockers are commonly used to manage HFpEF symptoms by removing excess fluid from the body and slowing the heart down so it has more time to fill. The use of diureticslike spironolactonehas even been found to increase life expectancy.
The American College of Cardiology and the American Heart Association recommend that cardiologists manage heart failure by its stage:
- Exercise capacity
- Diastolic function
Don’t Miss: How Much Can Marijuana Increase A Person’s Heart Rate
Using Ejection Fraction In Diagnosis
When examined using an echocardiogram, a significant number of patients with heart failure are revealed to have normal ventricular ejection fraction. This condition was previously called diastolic heart failure its now referred to as heart failure with preserved ejection fraction.
Your doctor may mention one of these two EF-related scenarios:
Proposals For The Future: Clues To Be Remembered
Diastolic dysfunction by itself is not enough to establish HFpEF. HFpEF is not simply a disease of aging nor does it occur only in females. HFpEF has significant phenotypic and etiologic heterogeneity. Due to its heterogeneity, a onesizefitsall strategy is unlikely to work in HFpEF. HFpEF is associated with multiple comorbidities. HFpEF is a multisystem disease, with the heart being a major component but with others providing major contributions. To date, two strategies that have been shown most definitively to be beneficial for improving clinically meaningful outcomes in HFpEF, ET and CR and both of these interventions have broad, pleotropic, systemic, and antiinflammatory effects, as well as favorable effects on multiple organ systems, including on arterial, cardiac, and skeletal muscle. Clinical trials defining optimal management for comorbidities have by and large excluded HFpEF patients. In addition, much broader research into myocardial and nonmyocardial abnormalities at a tissue level in carefully phenotyped HFpEF subgroups is very much needed.
Recommended Reading: How To Calculate Target Heart Rate Zone
