What Can Hospice Do For A Patient With Congestive Heart Failure Or Heart Disease
Your hospice team evaluates the patients status and updates the plan of care as CHF or heart disease symptoms and conditions change, even on a day-to-day basis. The goal of hospice is to manage symptoms and relieve physical/emotional distress so patients can live as fully as possible, retain their dignity and remain comfortable at home.
The hospice plan of care treats a wide range of heart disease symptoms, including:
- Shortness of breath
- Functional decline
When you turn to hospice, you are not alone in your journey your hospice care team is educated and experienced in advanced cardiac care, such as:
- Monitoring and managing your symptoms
- Communicating with your cardiologists office to intervene early and stabilize worsening conditions
- Providing medication, oxygen and other medical equipment related to your heart disease
- Providing services to reduce acute symptoms and avoid re-hospitalization
- Providing an average of 5 home visits per week and proactive phone calls
Hospice offers comprehensive services for patients with heart disease, such as:
Complications Of Congestive Heart Failure
Heart failure can lead to a number of complications that can influence the chance of survival, including:
- Rapid Weight Loss Severe heart failure can lead to an unintentional rapid loss of weight that can be life-threatening. Heart failure can cause blood to back up into the liver and intestines, causing these organs to swell. This swelling can lead to nausea and loss of appetite, and can prevent the body from absorbing nutrients from food.
- Impaired Kidney Function Congestive heart failure weakens the hearts ability to pump blood, reducing blood flow to the kidneys. This can lead to kidney damage or kidney failure if left untreated.
- Liver Damage Heart failure can cause fluid to build up on the liver, which can lead to scarring. This makes it more difficult for the liver to carry out its day-to-day functions.
- Arrhythmias Heart failure results in damaged heart muscles, which can lead to the development of an arrhythmia, or abnormal heart beat. Arrhythmias can include the heart beating too quickly, beating too slowly, or beating irregularly.
- Heart Valve Problems If the heart is enlarged due to heart failure, the valves of the heart, which ensure appropriate direction of blood flow through the organ, may not function properly.
- Angina and Heart Attack Heart disease is a major contributing factor in many heart failure cases, and people with congestive heart failure are at continued risk of angina and heart attack.
How You Can Help
-
Offer modified foods that are easy to digest.
-
Allow more time for eating and never rush your loved one.
-
Offer high protein supplements such as protein shakes.
-
Try offering popsicles if liquids are being refused.
-
Keep your loved ones mouth and lips moist to aid in comfort.
-
As hard as it is, be patient and understanding that this is part of the natural death and dying process.
Recommended Reading: How Serious Is Congestive Heart Failure
What To Expect During The Final Stages Of Congestive Heart Failure
Heart failure refers to when the heart cant or doesnt work well enough to provide oxygen and nutrients to the parts of the body and brain that need them. This decrease in cardiac output means the heart isnt strong enough to move blood from the body and lungs back to the heart. This causes fluid to leak from capillary blood vessels.
Shortness of breath, weakness, and swelling are some things that might happen because of this. Before we dive into the depths of the heart failure signs of death, lets understand what goes on in the body.
What Happens If You Have Heart Failure
People with heart failure have weak hearts that dont work as well as they should. Over time, the illness causes significant damage to the body.
In the first stages, the heart is less effective. It stretches, grows bigger, and pumps faster to compensate for the lack of strength. The body also changes, with arteries getting smaller and blood being directed away from certain body parts. Many people with heart failure dont know they have a problem in these early stages.
Towards the end stages of CHF, symptoms will worsen even if lifestyle changes are made, and the body will be unable to compensate for the loss of blood flow. As soon as that happens, the person may start to feel tired, have trouble breathing, and have other problems.
People can get help managing their end stages congestive heart failure symptoms and slowing down the progress of their condition with a variety of treatments. Its a long-term condition that cant be cured, as well as heart failure. People will eventually reach the end stages of heart failure.
Even when the person is lying down, they feel a shortness of breath. Their symptoms can change rapidly over a short period of time.
Read Also: Signs And Symptoms Of Right Sided Heart Failure
Supporting You And Your Loved Ones
A person-centered care model is how we approach caring for individuals and their families at the end-of-life. Hospice of Southern Illinois provides the personal care, attention and comfort during the final weeks and days of a loved ones prognosis. We want to ensure your loved ones comfort and dignity remains a priority. The circle of care for our patients starts with their needs and wishes and extends out to family, friends and caregivers. We are here to support and help you through what to expect too.
- Managing pain and other symptoms we carefully monitor pain levels and other symptoms, coordinate proper equipment, and evaluate medications to provide as much comfort and peace as possible.
- Providing support hospice offers regularly-scheduled visits from our care team to check in, provide education, listen, advocate, and explain what you need to know about the weeks ahead. Further, we offer emotional support to families along the way. Hospice care doesnt stop there. For several months after the loss of a loved one, we continue to be available for bereavement support.
- Knowing what to expect as the experts in end-of-life care, you can trust that we will work tirelessly to keep your loved one comfortable, supported and safe, all the while keeping you informed of any changes.
What Causes Congestive Heart Failure
There are several conditions that can impair the pumping efficiency of the heart. Below are a few common and rare conditions that can cause congestive heart failure:
- Coronary artery disease : This is the most common cause of congestive heart failure, as the arteries become blocked or severely narrowed, which decreases blood flow to the heart.
Read Also: Can Sinus Infection Cause Increased Heart Rate
Further Resources On Heart Failure & Hospice Care
A selection of resources to support the implementation of a hospice-enabled approach to heart failure, including presentations from Hospice UK’s 2016 conference – ‘People, partnerships and potential’
- Palliative care for heart failure
Palliative care for heart failure: service development in West Hertfordshire
Speaker: Dr. Sharon Chadwick, Medical Director, Hospice of St. Francis.
- Heart Failure: vital steps for palliative care
Speaker: Dr. Karen Hogg, Consultant Cardiologist, Glasgow Royal Infirmary.
- Palliative care for end-stage heart failure
Speaker: Prof. Miriam Johnson, Professor of Palliative Medicine, Hull York Medical School.
When Should We Consider Hospice Care For Chf
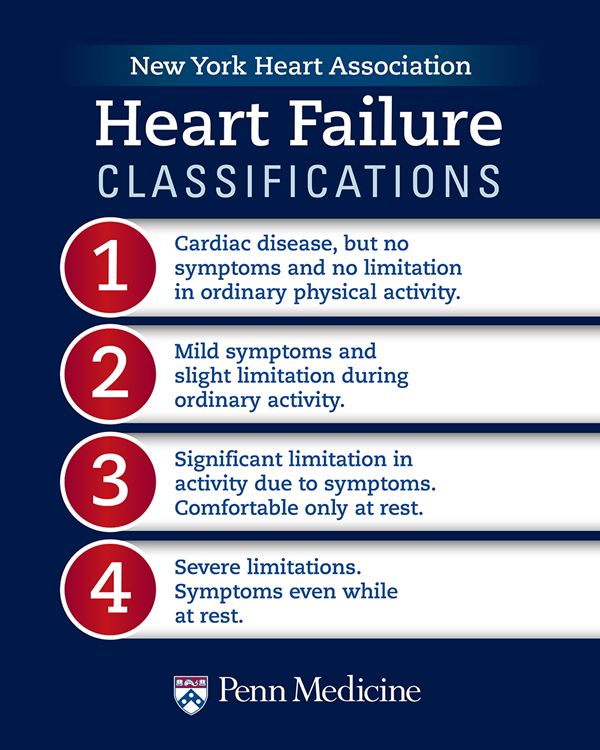
Hospice can be appropriate for many types of end-stage heart disease, including heart failure, valvular heart disease and coronary artery disease. Regardless of the type of heart disease, hospice is a fitting choice when an individual begins to experience persistent, severe symptoms that interfere with their daily life. Hospice care should also be considered if an individual begins to have recurrent hospitalizations or complicated hospitalizations, such as an ICU stay.
One of the earliest symptoms of a declining heart is exercise intolerance. This begins with symptoms present with significant exertion and can progress to symptoms present with doing our activities of daily living, such as bathing and dressing. At its worst, symptoms are present at rest. Heart disease, depending on the etiology, can present with other more specific symptoms, including fluid overload, chest pain, lightheadedness, shortness of breath and arrythmias. Patients may experience unintentional weight loss despite a normal appetite. As the disease progresses, cardiac output can decline, resulting in low blood pressure and poor prefusion of our vital organs. This can lead to dysfunction of further organ symptoms, such as worsening kidney function.
Read Also: Arm Pain And Heart Attack
When To Begin Planning
It can be hard to know when to start making plans for the end of life. The progression of a long-term condition like heart failure can be unpredictable, which makes it difficult to know when the time is right. Its important to discuss things with your healthcare professional as early as you can. Many routine face-to-face appointments are being cancelled because of coronavirus, so check if your nurse or doctor is running telephone appointments instead. By discussing things as early as possible, it means you to have time to think about treatment options and preferences and where youd want to be cared for towards the end of your life. This may help you achieve some peace of mind and a sense of control.
A: Patient Understanding Of Disease And Prognosis
A1: Dealing with advanced heart failure and ageing
Patient statements revealed different levels of perspectives related to heart failure, ranging from descriptions of their illness adaption to changing conditions , appraisal of their own quality of life , and their handling of information regarding their illness .
A1.a: Perception of heart failure
The patients described various experiences with symptoms of heart failure, in particular, limitations such as shortness of breath, dizziness, and restrictions in activities of daily living. Frequently, they did not perceive heart failure as a life-limiting, chronic disease with a long-term course, but rather as a disease with acute life-threatening events. The patients often believed their condition was a result of their old age and not a genuine illness. Medical definitions and personal experiences may diverge: Despite their specific diagnosis and treatment, the patients reported feeling well. Consequently, they may play down their symptoms and not take their medications. However, changes in the patients perceptions were sometimes observed when their condition worsened:
Patient P1, T3 : But my heart, thats not really the problem. That is high blood pressure. Yes, I have that! Oh, yeah! You know, now now I have it under control. You know, I have never taken any pills. Yeah, and I watch out for my blood pressure. But if I say I take my tablets, that I do not do that anymore.
A.1b: Adaption to changing conditions
You May Like: What Does Heart Attack Look Like On Ekg
Management Of End Stage Cardiac Failure
Palliative care can be used for anyone who is in the advanced stages of an illness, including end stage heart failure. While it does not suspend any treatment of the illness, it does help an individual improve his or her quality of life by focusing on finding relief from the symptoms and stress caused by the illness. Palliative care is provided by a team of doctors, nurses and other health care specialists who work together with a patients primary physician to give an ailing loved one the support services he or she requires.
Weeks Before Death Symptoms
Several weeks before death, your loved one may start exhibit a range of behavioral changes relating to their sleeping patterns, eating habits and sociability. They may begin to sleep more often and for longer periods. They will start to refuse foods that are difficult to eat or digest, but eventually they will refuse all solid foods. Do not try to force them to eat, as it will only bring discomfort to them. Your loved one may enjoy ice during this time, since it will keep them cool while also hydrating them.
Unfortunately, your loved one may become withdrawn, less active and less communicative. They may spend more time alone introspecting and may turn down company. Some also appear to become comatose and unresponsive, but this is a symptom of withdrawal. Your loved one can still hear you, so speak in a calm, reassuring voice while holding their hand. Children may become more talkative, even if they withdraw from other activities. Its important to let your loved one set their own pace during this time. Your loved one may also start to use metaphorical language, which could be a way of coping with death. It may also be used to allude to a task they feel they need to accomplish, such as seeking forgiveness.
Common symptoms in this period also include physical changes, such as:
- Chronic fatigue
- Swelling of the abdomen, such as edema or ascites
Also Check: Pathophysiology Of Congestive Heart Failure
What Are The Types Of Heart Failure
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure
Heart failure with reduced left ventricular function The lower left chamber of your heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of your body.
Heart failure with preserved left ventricular function Your heart contracts and pumps normally, but the bottom chambers of your heart are thicker and stiffer than normal. Because of this, your ventricles can’t relax properly and fill up all the way. Because there’s less blood in your ventricles, your heart pumps out less blood to the rest of your body when it contracts.
Right-sided heart failure
Heart failure can also affect the right side of your heart. Left-sided heart failure is the most common cause of this. Other causes include certain lung problems and issues in other organs.
Planning Ahead Heart Failure And The End Of Life
To be told that youre approaching the end of your life, even if youve been ill for a long time, can be very upsetting and difficult to come to terms with.
If you or a loved one is approaching the end of their life, it may be particularly hard during the coronavirus pandemic. The rules on visiting people in hospital, care homes and hospices have changed, as have funeral arrangements. Its important to be aware of these changes and take them into account when making plans for the end of life. If youve already made plans, you might need to alter them. Although it can seem tough at first, sorting out practical matters such as your will, finances and how and where youd like to be cared for, can be a very positive thing to do and give you peace of mind. Its a good idea to start thinking about these plans and putting things in place as soon as you feel well enough to do so.
-
Visit our coronavirus support hub if you have a heart condition and are worried about coronavirus.
Don’t Miss: Can Prednisone Cause Heart Palpitations
New Moms And Heart Failure Risk
A study published in January 2018 in the journal Circulation: Heart Failure found that women are most at risk for heart failure within the first six weeks after delivery, also known as the postpartum period.
The research supports the notion that at-risk women need closer observation postpartum.
The researchers also say that because many women are discharged from hospital care just a couple of days after they give birth and arent given a follow-up until about six weeks later, the way doctors regard women who might be at risk of heart failure needs to change.
They call for comprehensive discharge health education, with emphasis on signs and symptoms to look for and when or where to seek immediate care.
Taking Care Of Yourself
Knowing youre coming towards the end of your life can be scary and upsetting. You may even feel angry. You might find that these feelings are made worse by the constant coverage of the coronavirus pandemic and the discussions about death on the news as well as the unknown, and the thought of leaving family and loved ones behind.
-
Visit our emotional support hub to get help for anxiety, depression and loneliness.
It can really help your mental wellbeing to keep a sense of structure in your life and practice self-care. Depending on your symptoms and how youre feeling, you might not feel up for doing this. But if you can, try to:
-
do gentle activity exercise if you can, or try to move about
-
do things you enjoy hobbies/reading/watching TV
-
keep in contact with family and friends via telephone or social media.
Also Check: How To Measure Resting Heart Rate
Days Before Death Symptoms
In the days before death, a series of physiological changes will occur. Their pulmonary system will start to degrade and the will become congested, leading to a tell-tale death rattle. Their breathing will also exhibit fluctuations, as they may begin to respirate up to 50 times per minute or as little as six. When exhaling, they may puff their lips. They may also begin to cough more frequently, but in general, the congestion itself is painless.
During their last days, your loved one may begin to experience hallucinations in which they talk to people who arent there or who have also died. It is important to maintain a close eye on your loved one if they begin exhibiting these symptoms. There is no guarantee for how long they may have left, and some people pass through this process faster than others.
Some common symptoms those a few days from death experience include:
- A drop in blood pressure
- The body temperature changes frequently
- Skin changing color or becoming blotchy
- Erratic sleeping patterns
Heart Failure Survival Rates
The survival rates from heart failure have been improving over the years. The improvement is slow, but gradual. Clinicians measure overall patient survival from a disease by comparing large groups of people with the disease to large groups of the same age range without it. For example, a 1-year survival rate of 90% is good. It means people with the disease are 90% as likely as people without the disease to be alive for at least one year after diagnosis. For heart failure, the 1-year survival rate rose from 74% in 2000 to about 81% in 2016. The 5-year survival rate increased from 41% to 48%, and the 10-year survival rate rose from about 20% to 26%.
Keep in mind prognosis and life expectancy information is based on data registries from several years ago . Someone diagnosed with heart failure today may have a better prognosis because heart failure treatment, including heart transplant, improves with time.
If you or a loved one has heart failure and you would like to know more about your case, ask your doctor how your age, overall health, and treatment affect your prognosis and life expectancy. Knowing what to expect can help you make plans for the time you have.
Dont Miss: How To Calculate Target Heart Rate Zone
Also Check: What Is The Best Hospital For Heart Surgery
