Pathogenesis Congestive Cardiac Failure
Heart failure may be caused by one of the following factors either singly or in combination.
Intrinsic Pump Failure: The most common and most important cause of heart failure is the weakening of the ventricular muscle due to disease so that the heart fails to act as an efficient pump. The various diseases which may culminate in pump failure by these mechanisms are as under:
Increased workload on the heart: Increased mechanical load on the heart results in increased myocardial demand resulting in myocardial failure. Increased load on the heart may be in the form of pressure load or volume load.
Increased pressure load may occur in the following states:
Increased volume load occurs when a ventricle is required to eject more than the normal volume of the blood resulting in cardiac failure. This is seen in the following conditions:
Impaired filling of cardiac chambers: Decreased cardiac output and cardiac failure may result from extracardiac causes or defects in filling of the heart in pericarditis.
What Is Heart Failure
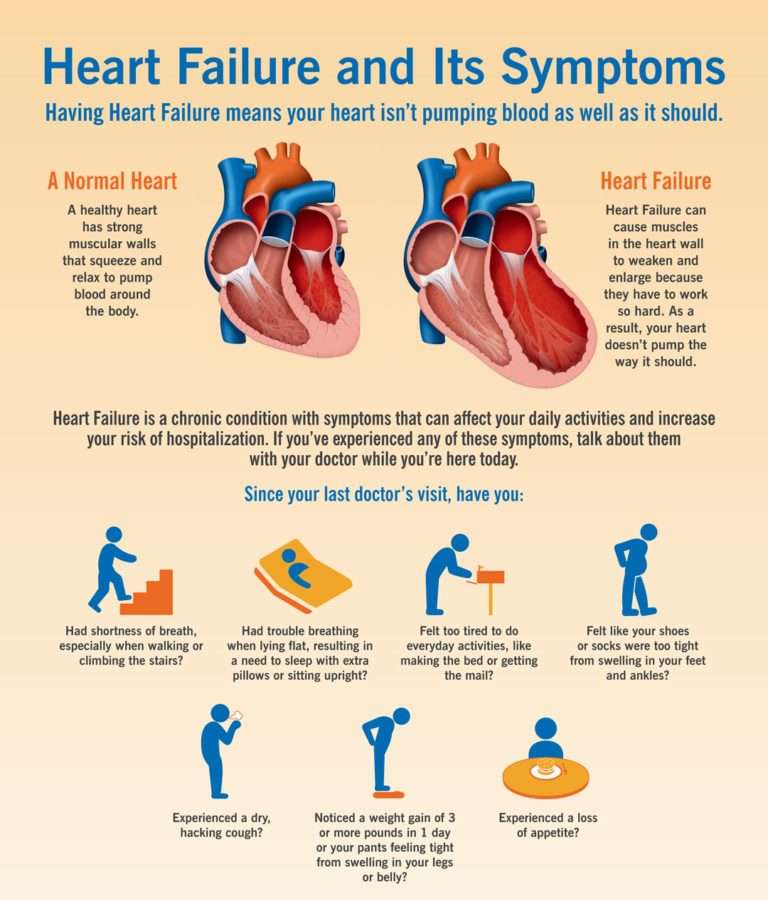
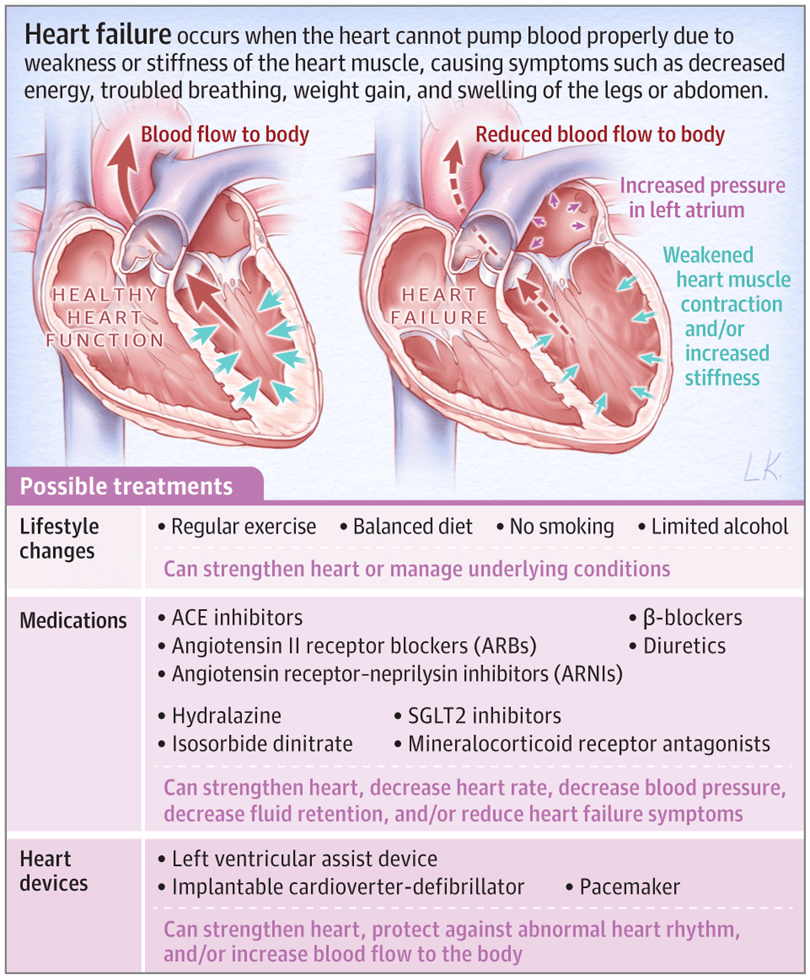
Heart failure, or congestive heart failure, is a long-term condition that gets worse over time. Although the name sounds like your heart has stopped working, heart failure means your heart isnt able to pump blood as well as it should. When your heart has less pumping power, that can damage your organs and fluid can collect in your lungs.
You Don’t Have To Face Hf Alone
The term heart failure makes it sound like the heart is no longer working at all and theres nothing that can be done. Actually, heart failure means that the heart isnt pumping as well as it should be. Congestive heart failure is a type of heart failure that requires seeking timely medical attention, although sometimes the two terms are used interchangeably.
Your body depends on the hearts pumping action to deliver oxygen- and nutrient-rich blood to the bodys cells. When the cells are nourished properly, the body can function normally.With heart failure, the weakened heart cant supply the cells with enough blood. This results in fatigue and shortness of breath and some people have coughing. Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult.
Heart failure is a term used to describe a heart that cannot keep up with its workload. The body may not get the oxygen it needs.
Heart failure is a serious condition, and usually theres no cure. But many people with heart failure lead a full, enjoyable life when the condition is managed with heart failure medications and healthy lifestyle changes. Its also helpful to have the support of family and friends who understand your condition.
You May Like: How To Read Heart Rate Monitor
Diagnosis Of Heart Failure Of Acute Onset
|
Data from Ponikowski P, Voors AA, Anker SD, et al: 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology Developed with the special contribution of the Heart Failure Association of the ESC. European Heart Journal 37:2129-2200, 2016. doi: 10.1093/eurheartj/ehw128 |
What Are The Stages Of Congestive Heart Failure
Based on the symptoms and the amount of effort required to provoke them, the New York Heart Association has divided degrees of heart failure into four classes:
- Class I: Patients have no limitation of physical activity.
- Class II: Patients have a slight limitation of physical activity.
- Class III: Patients have marked limitations of physical activity.
- Class IV: Patients have symptoms even at rest and are unable to carry on any physical activity without discomfort.
Recommended Reading: How Does Music Affect Your Heart Rate
Pathophysiology Of Heart Failure
Kardiologie, Nephrologie/Hypertonie, Pneumologie, Internistische Intensivmedizin, Medizinische Klinik II, Klinikum Weiden, Weiden, Germany
Correspondence to:
Keywords: Heart failure pathophysiology HFpEF HFrEF treatment of heart failure
Submitted Feb 28, 2020. Accepted for publication May 28, 2020.
doi: 10.21037/cdt-20-302
Congestive Heart Failure: Prevention Treatment And Research
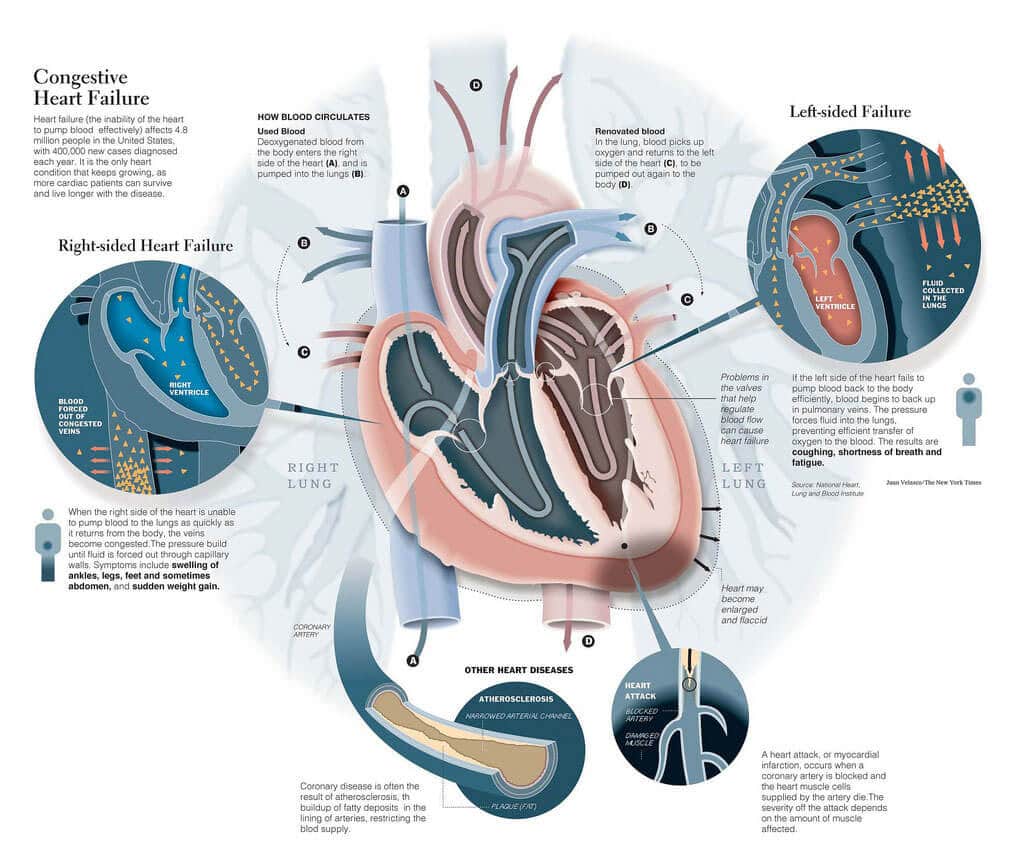
Congestive heart failure is a serious condition in which the heart doesnt pump blood as efficiently as it should. Despite its name, heart failure doesnt mean that the heart has literally failed or is about to stop working. Rather, it means that the heart muscle has become less able to contract over time or has a mechanical problem that limits its ability to fill with blood. As a result, it cant keep up with the bodys demand, and blood returns to the heart faster than it can be pumped outit becomes congested, or backed up. This pumping problem means that not enough oxygen-rich blood can get to the bodys other organs.
The body tries to compensate in different ways. The heart beats faster to take less time for refilling after it contractsbut over the long run, less blood circulates, and the extra effort can cause heart palpitations. The heart also enlarges a bit to make room for the blood. The lungs fill with fluid, causing shortness of breath. The kidneys, when they dont receive enough blood, begin to retain water and sodium, which can lead to kidney failure. With or without treatment, heart failure is often and typically progressive, meaning it gradually gets worse.
More than 5 million people in the United States have congestive heart failure. Its the most common diagnosis in hospitalized patients over age 65. One in nine deaths has heart failure as a contributing cause.
Don’t Miss: Does Diltiazem Lower Heart Rate
Changes In Function And Expression Of Ion Channels And Contractile Proteins
Various processes involved in the conversion of an electrical stimulus to a mechanical response i.e., excitation contraction coupling are altered in human heart failure part of these alterations are expression and function of the ion channels or transporters , contractile proteins , intracellular calcium transport processes . Both, the calcium induced calcium release and the intracellular calcium handling is affected in heart failure leading to reduced contractility and prolonged relaxation . In consequence, in human heart failure the frequency-induced force generation is reduced or even absent i.e., negative force-frequency-relationship the intracellular free calcium concentration is enhanced and the Ca2+ sensitivity of the contractile proteins is increased . Following reduced ß-adrenoceptor response in heart failure phosphorylation of several Ca2+-handling proteins is reduced and Ca2+ affinity of contractile proteins is increased. Both mechanisms impair contraction and relaxation further. In addition, Na efflux via the NCX is affected as well leading to increased intracellular Na and reduced K. In consequence, the resting membrane potential is shifted to depolarization which acts proarrhythmogenic. The altered intracellular Ca2+ handling in human heart failure affect also mitochondria energy production and in consequence further deteriorate myocardial function .
Symptoms Of Heart Failure
Symptoms of heart failure include:
- new or worsening shortness of breath
- difficulty lying flat at night
- fainting or passing out
- muscular fatigue, tiredness
- swelling of ankles or legs
- swelling of abdomen
- heart palpitations
- chest pain or discomfort in parts of the upper body
- unexplained coughing and wheezing
Recommended Reading: Congestive Heart Failure Lasix
Anemia And Iron Deficiency
Anemia is common among patients with chronic heart failure and is frequently multifactorial. Anemia is associated with worse symptoms and outcomes in HF and so reversible causes should be sought and treated. Iron deficiency Iron Deficiency Anemia Iron deficiency is the most common cause of anemia and usually results from blood loss malabsorption, such as with celiac disease, is a much less common cause. Symptoms are usually nonspecific read more is among the most common causes of anemia in HF, and iron replacement therapy should be considered once treatable causes such as blood loss have been excluded. Oral iron replacement is often less effective due to poor absorption and other reasons, thus intravenous iron replacement is preferred.
Clinical Manifestations Of Heart Failure
The clinical manifestation of heart failure is largely influenced by the primary side of dysfunction as left sided, right sided or biventricular. Left ventricular dysfunction increases pulmonary pressure and consequently pulmonary congestion occurs leading to dyspnoea and tachypnoea . As the peripheral circulation is reduced , renal dysfunction, peripheral malperfusion and malabsorption of nutrition with the signs of cardiac cachexia develop. In a chronic state, the permanent activation of neurohumoral systems lead to further volume overload , peripheral vasoconstriction , increased heart rate at rest and during exercise, and to a further deterioration of the cardio-renal system. Anemia , increased pulmonary pressure and muscle fatigue deteriorate the symptoms of dyspnoea as well. Overload of the heart leads to enlargement of the heart itself and as a measure the cardiothoracic index increases with leftward shift of the palpable cardiac pulsation. Mostly in volume overload situations filling volume of the ventricle increases periodically and a typical 3rd or 4th heart sound as protodiastolic gallop occurs . In consequence, heart failure influences almost all organ systems and thus heart failure is a systemic disease or a syndrome with a broad clinical spectrum.
Don’t Miss: What Should My Heart Rate Be When Walking
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Stages Of Heart Failure
CHF is usually an irreversible condition that gets worse over time. The stages of heart failure describe the severity of the conditions. Here are the four stages of heart failure according to the American College of Cardiology:
- Stage A: People have a high risk for developing heart failure, but there are no symptoms or changes in heart function. People in this category often have one or more conditions that may lead to heart failure.
- Stage B: People with stage B heart failure have changes to the heart function but havent experienced symptoms of heart failure. The ejection fraction may be below normal range.
- Stage C: During this stage, people will experience decreased heart function and currently or previously experienced symptoms of heart failure.
- Stage D: In stage D, people experience constant symptoms of heart failure. If they have heart failure with reduced ejection fraction. the ejection fraction will be significantly lower.
Recommended Reading: How To Lower Heart Rate Instantly
What Is Congestive Heart Failure
Heart failure is a condition in which the heart is unable to pump blood to body tissues efficiently. Congestive heart failure is a chronic disease that progresses with time if left untreated. Heart failure can occur due to diseases of the heart, the blood vessels supplying oxygen and nutrients to the heart, or sometimes from factors outside the heart . A healthy lifestyle plays a role in the treatment and prevention of congestive heart failure.
Surgery And Percutaneous Procedures
Surgery may be appropriate when certain underlying disorders are present. Surgery in patients with advanced HF should be done in a specialized center.
Surgical closure of congenital or acquired intracardiac shunts can be curative.
If HF is primarily due to a valvular disorder Overview of Cardiac Valvular Disorders Any heart valve can become stenotic or insufficient , causing hemodynamic changes long before symptoms. Most often, valvular stenosis or insufficiency read more , valve repair or replacement should be considered. Patients with primary mitral regurgitation are more likely to benefit than patients with mitral regurgitation secondary to LV dilation, in whom poor myocardial function is likely to continue postoperatively. Surgery is preferably done before myocardial dilation and damage become irreversible. More recently, percutaneous mitral valve repair procedure, in which a clip is applied to approximate the anterior and posterior mitral leaflets, has been shown to reduce death and HF hospitalization in carefully selected patients with symptomatic HF despite optimal medical management and moderate to severe or severe mitral regurgitation with preserved LV size is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal fluid read more ).
Don’t Miss: What Effect Does The Nervous System Have On The Heart Rate
Energetic Aspects In Heart Failure
The contractile machinery is dependent on a substrate utilization , oxidative phosphorylation , and high-energy phosphate metabolism . Each of these components or a combination of these may be affected in heart failure and lead to energy starvation and in consequence affect contractile function . Mitochondrial high-energy phosphate production is the predominant energy source for cardiomyocytes. Alterations in the mitochondrial energy support lead to myocyte dysfunction , promote apoptosis and thus may favor heart failure further . Thus, reduced energy levels inhibit Ca2+ influx via the sarcolemmal L-Type calcium channel and reduce sarcoplasmatic Ca2+-re-uptake via reduced phosphorylation of phospholamban. These mechanisms reduce contractility and slower relaxation and may also be the target for treatment options . In patients with heart failure treatments targeting substrate utilization and/or oxidative stress in mitochondria will be tested in addition to the well defined neuroendocrine inhibition .
About Congestive Heart Failure
Heart failure, sometimes called congestive cardiac failure , is a condition in which the heart muscle is weakened and cant pump as well as it usually does. The main pumping chambers of the heart can change size and thickness, and either cant contract or cant relax as well as they should. This triggers fluid retention, particularly in the lungs, legs and abdomen.
The major causes of heart failure include coronary heart disease and heart attack, high blood pressure, damage to the heart muscle , heart valve problems and abnormal heart rhythms. Of these, coronary heart disease and heart attack are the most common causes.
The major factors that contribute to coronary heart disease include:
- reduced emotional and social wellbeing
- physical inactivity.
Heart failure is more common in elderly people. The survival rate for people with this disorder depends on the severity of their condition.
Most common treatments for heart failure are medications and self-managed lifestyle changes. Some less-common treatments may require insertion of implantable cardiac devices or valve replacement.
Don’t Miss: What Do Beta Blockers Do To Heart Rate
How The Normal Heart Works
The normal healthy heart is a strong, muscular pump a little larger than a fist. It pumps blood continuously through the circulatory system.
The heart has four chambers, two on the right and two on the left:
- Two upper chambers called atria
- Two lower chambers called ventricles
The right atrium takes in oxygen-depleted blood from the rest of the body and sends it through the right ventricle where the blood becomes oxygenated in the lungs.
Oxygen-rich blood travels from the lungs to the left atrium, then on to the left ventricle, which pumps it to the rest of the body.
The heart pumps blood to the lungs and to all the bodys tissues through a sequence of highly organized contractions of the four chambers. For the heart to function properly, the four chambers must beat in an organized way.
Read Also: What Should Heart Rate Be
Congestive Heart Failure Pathophysiology And Schematic Diagram
Congestive heart failure otherwise known as cardiac failure refers as the inability of the heart to pump sufficient blood to meet needs of tissues for oxygenation and nutrition. This disease can affect the hearts ability to respond to circulation demands of the body. CHF is a slowly developing condition where cardiac output is lower-than-normal.
Recommended Reading: Can Congestive Heart Failure Be Reversed
What Causes Heart Failure
Although the risk of heart failure doesnt change as you get older, youre more likely to have heart failure when youre older.
Many medical conditions that damage the heart muscle can cause heart failure. Common conditions include:
- Tobacco and recreational drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
How Is Heart Failure Diagnosed
To find out if you have heart failure, your doctor will:
- Ask about your medical history, including your symptoms
- Ask about your family health history, including relatives who have had heart failure
- Do a physical exam
In some cases, your doctor may refer you to a cardiologist for tests, diagnosis, and care.
You May Like: What Causes Increased Heart Rate
Myocytes And Myocardial Remodeling
In the failing heart, increased myocardial volume is characterized by larger myocytes approaching the end of their life cycle. As more myocytes drop out, an increased load is placed on the remaining myocardium, and this unfavorable environment is transmitted to the progenitor cells responsible for replacing lost myocytes.
Progenitor cells become progressively less effective as the underlying pathologic process worsens and myocardial failure accelerates. These featuresnamely, the increased myocardial volume and mass, along with a net loss of myocytesare the hallmark of myocardial remodeling. This remodeling process leads to early adaptive mechanisms, such as augmentation of stroke volume and decreased wall stress and, later, to maladaptive mechanisms such as increased myocardial oxygen demand, myocardial ischemia, impaired contractility, and arrhythmogenesis.
As heart failure advances, there is a relative decline in the counterregulatory effects of endogenous vasodilators, including nitric oxide , prostaglandins , bradykinin , atrial natriuretic peptide , and B-type natriuretic peptide . This decline occurs simultaneously with the increase in vasoconstrictor substances from the RAAS and the adrenergic system, which fosters further increases in vasoconstriction and thus preload and afterload. This results in cellular proliferation, adverse myocardial remodeling, and antinatriuresis, with total body fluid excess and worsening of heart failure symptoms.
When Should I Get Emergency Care
Go to the ER or call 911 if you have:
- New, unexplained, and severe chest pain that comes with shortness of breath, sweating, nausea, or weakness
- Fast heart rate , especially if you are short of breath
- Shortness of breath that doesnt get better if you rest
- Sudden weakness, or you cant move your arms or legs
- Sudden, severe headache
- Fainting spells
You May Like: Tyrone Davis Heart Failure
