Congestive Heart Failure And Weight Loss
First, weight loss congestive heart failure may occur because of a lack of blood flow to the gastrointestinal tract. A 2014 study which observed a small group of patients noticed that those with the most drastic unintentional weight loss also had the lowest intestinal blood flow.
Low blood flow around the gastrointestinal tract may make it harder for the body to absorb nutrients and move food through the body. Along with that, general symptoms of congestive heart failure including dizziness, nausea, and fatigue may make it difficult for late-stage patients to eat.
Mood disorders such as anxiety and depression may also cause unplanned weight loss in late-stage congestive heart failure. Many of these symptoms can be managed with medication and should be discussed with caregivers.
Weight Change Over First 6 Months
The distribution of percentage weight change over 6 months follow-up is shown in Figure A, along with the number dying and crude death rate during a subsequent median further follow-up of 32.9 months. The distribution of BMI is shown in Figure B.
Mortality hazard ratios adjusted for baseline predictors, and crude death rates per 100 person-years, for percentage weight change and BMI, in the fixed 6 month Cox model.
There was a highly significant relationship towards a higher crude death rate with increasing weight loss. Weight gain during the first 6 months of the study was not associated with increased death rates. There was also a marked inverse relationship between the BMI and the death rate.
The associations of percentage weight change and mean BMI with those baseline variables previously shown to predict mortality are presented in Table . More than 5% weight loss within 6 months appeared more commonly in patients who were older, female, NYHA class IV, and with dependent oedema. Patients on candesartan gained a mean 0.71 kg at 6 months compared with placebo , and hence there were fewer patients with over 5% weight loss within 6 months on candesartan .
Relationship of percentage weight change over 6 months, and mean BMI to other patient factors previously shown to predict mortality risk
| Baseline variables . |
|---|
What Is Heart Failure
The term heart failure sounds scary. But it simply means your heart isnt pumping blood as well as it should. It can be caused by many different heart conditions and tends to get worse over time. It does not mean your heart has stopped working or that you are having a heart attack. The most common cause of heart failure is congestive heart failure . This means fluid is building up in the body because the heart isnt pumping properly.
Also Check: Women Heart Attack Signs
Weight Loss Risk Factors
There are several reasons that cause weight loss in this scenario. Some of those are
- Lack of blood flow It is observed that the reason for weight loss after a heart failure may occur from lack of blood flow to the gastrointestinal tract. Low blood flow surrounding the gastrointestinal tract can make the body harder to absorb nutrients and vitamins that move through the body. People have a drastic weight loss, have the lowest intestinal blood flow.
- Mental health Mental and psychological health plays a significant role in heart failure and weight loss as well. Nowadays many people are suffering from anxiety and depression, though it varies from person to person it impacts somewhat the same on weight loss and congestive heart failure.
- Previous illness Sometimes an existing health condition can lead to heart failure. Patients who have diabetes, blood sugar, or similar diseases usually experience a higher chance of heart failure as compared to a normal person. This can result in even poorer metabolism and overall loss of muscle mass.
What Is Congestive Heart Failure
Heart failure describes the inability or failure of the heart to meet the needs of organs and tissues for oxygen and nutrients. This decrease in cardiac output, the amount of blood that the heart pumps, is not adequate to circulate the blood returning to the heart from the body and lungs, causing the fluid to leak from capillary blood vessels. This leads to symptoms that may include shortness of breath, weakness, and swelling.
Understanding blood flow in the heart and body
The right side of the heart pumps blood to the lungs while the left side pumps blood to the rest of the body. Blood from the body enters the right atrium through the vena cava. It then flows into the right ventricle where it is pumped to the lungs through the pulmonary artery, which carries deoxygenated blood to the lungs. In the lungs, oxygen is loaded onto red blood cells and returns to the left atrium of the heart via the pulmonary veins. Blood then flows into the left ventricle where it is pumped to the organs and tissues of the body. Oxygen is downloaded from red blood cells into the various organs while carbon dioxide, a waste product of metabolism, is added to be removed in the lungs. Blood then returns to the right atrium to start the cycle again. The pulmonary veins are unusual in that they carry oxygenated blood, while the pulmonary artery carries deoxygenated blood. This is a reversal of duties versus the roles of veins and arteries in the rest of the body.
Don’t Miss: Can Ekg Detect Heart Failure
What Will Happen Towards The End
Heart failure usually gets gradually worse over time. It may eventually reach a point where it becomes very severe and its unlikely the person will live much longer.
Palliative care will usually begin when heart failure reaches this stage.
This involves treatment to help you feel as comfortable as possible, as well as being offered psychological, spiritual and social support for both you and your family.
You can choose whether you want palliative care and where youd like it to be provided.
Care can be provided:
Obesity Paradox In Hf: Myth Or Reality
The obesity paradox has been a long-standing controversy with studies demonstrating lower mortality in obese patients with HF. Horwich et al were the first to report the obesity paradox in HF. Further studies have reported best outcomes in the overweight or obese categories with increasing mortality seen at the extreme ends of the scale. The current meta-analysis confirms the paradoxical decline in all-cause mortality with increasing obesity and demonstrates a U-curve for CV mortality with best outcomes in the overweight group.
You May Like: Leaking Heart Valve Life Expectancy With Surgery
Symptoms Of Heart Failure
Some people who have heart failure have few problems or symptoms. Others may have many symptoms, including:
- Shortness of breath during activity
- Shortness of breath when lying down
- Lack of appetite
- Waking up in the night, suddenly breathless
- General tiredness or weakness, including the reduced ability to exercise
- Swelling of the legs, feet, or ankles
- Swelling of the abdomen
- Rapid weight gain
- Chronic cough or wheezing
What causes heart failure?
Heart failure has many causes. Most of these are other conditions or diseases that damage the heart muscle. These could include:
- Coronary artery disease . This could be with or without a heart attack in the past
- Problems with the heart muscle itself .
- Problems with any of the heart valves
- Abnormal heart rhythms
- The use of toxic substances
- Congenital heart defect
- Thyroid problems
Sometimes, the exact cause cannot be found. Some people are at higher risk of developing heart failure, including those who are:
- 65 years or older
- Have had a heart attack in the past
Unintentional Weight Loss And Cardiac Event
Figure 2 shows the unadjusted hazard ratio for percentage weight change over the six month follow-up period. Patients who experienced unintentional weight loss of greater than 6% had a 2.5 times higher risk for cardiac events compared to those with weight loss or weight gain within 1% .
Unadjusted hazard ratio for percentage weight changes over six months
Table 3 presents the results from hierarchical Cox proportional hazard regression analysis predicting cardiac event-free survival in HF patients. Initially, other clinical variables including age, gender, HF etiology, BMI, NYHA functional class, left ventricular ejection fraction, total comorbidity score, use of ACE inhibitors, diuretics, and beta blockers were included in the first step. After depressive symptoms and log-transformed hsCRP as continuous variables were added in the second step, unintentional weight loss was added in the final step. Decreased LVEF was the only control variable to independently predict cardiac event-free survival . In hierarchical Cox proportional hazard regression, unintentional weight loss predicted cardiac event-free survival after controlling for other clinical variables, depressive symptoms and log-transformed hsCRP. Patients with unintentional weight loss had a 3.2 times higher risk for cardiac events compared to those without unintentional weight loss (p< 0.001
Recommended Reading: How To Get Rid Of Heart Attack Symptoms
What If I Get Thirsty
Being thirsty does not always mean your body needs more fluid. Be careful NOT to replace fluids that diuretics help your body get rid of. Try these tricks if you get thirsty:
- Snack on frozen grapes or strawberries
- Chew sugar-free gum or suck on hard candy
- Suck on ice chips or a washcloth soaked in ice water
- Avoid milk, ice cream and salt as they can make you thirsty
- Use lip balm or petroleum jelly to keep your lips moist
If you sweat a lot or are outdoors in hot weather, make sure you do not become dehydrated. Signs of dehydration/not taking in enough fluids are:
- Feeling dizzy when you move around
- Very dry mouth and tongue
If you have signs of dehydration, have one or more extra cups of water or other fluid.Reviewed: 10/16
Symptoms Of Congestive Heart Failure
Symptoms of congestive heart failure revolve around the bodys inability to keep blood flowing. Depending on what stage a patient is at and how the disease is progressing, symptoms include:
Shortness of breath: Fluids can build up in the lungs, and blood can back up around the lungs. Shortness of breath can persist even while resting, especially while laying down.
Bloating: Since the heart cannot maintain the pressure needed to move fluids throughout the body, water retention increases and may cause bloating. Most commonly, this comes in the form of swelling in the ankles and feet.
Irregular heartbeats: The heart is struggling to move blood through the body and may skip beats or beat too quickly, even while resting, to catch up.
Dizziness and Fatigue: Because not enough blood is flowing through vital organs and to the brain, its common to feel fatigued. Dizziness, lightheadedness, or clouded thinking may also occur to a reduced oxygen flow.
Its important to note that congestive heart failure shares symptoms with many other heart problems and other diseases. While having one of these symptoms may not mean heart failure, its always best to speak with a doctor and ask for a heart check.
Read Also: How To Calculate Heart Rate On Ecg Strip
Health Supplements Likely Do More Harm Than Good
The researchers pointed out that many products advertised as nutritional supplements based in wellness not only have no health benefits but could in fact be harmful. Often, these products boast potential outcomes with no clinical evidence to support the companys claims.
As with any drug, it is important to put HDSs through preclinical and clinical scientific studies and postmarketing vigilance so that unknown and potentially harmful causes for severe adverse effects, such as liver failure due to the use of such agents, may be more identifiable and controlled, the researchers wrote.
–
Editors Note Jan 2, 2020:
Losing Weight Can Lower Your Cholesterol
Obesity can lead to high cholesterol, and high cholesterol can lead to heart disease. Just being overweight doesnt necessarily mean your cholesterol levels are high though because genes, hormones, and environmental circumstances all impact your cholesterol levels. However, if youre overweight and you eat lots of unhealthy foods like processed meats, baked goods, and fast food, you could be at risk. Losing weight could lower your cholesterol, which helps balance the fats in your bloodstream, and helps your heart function normally.
Also Check: Can Constipation Cause Heart Palpitations
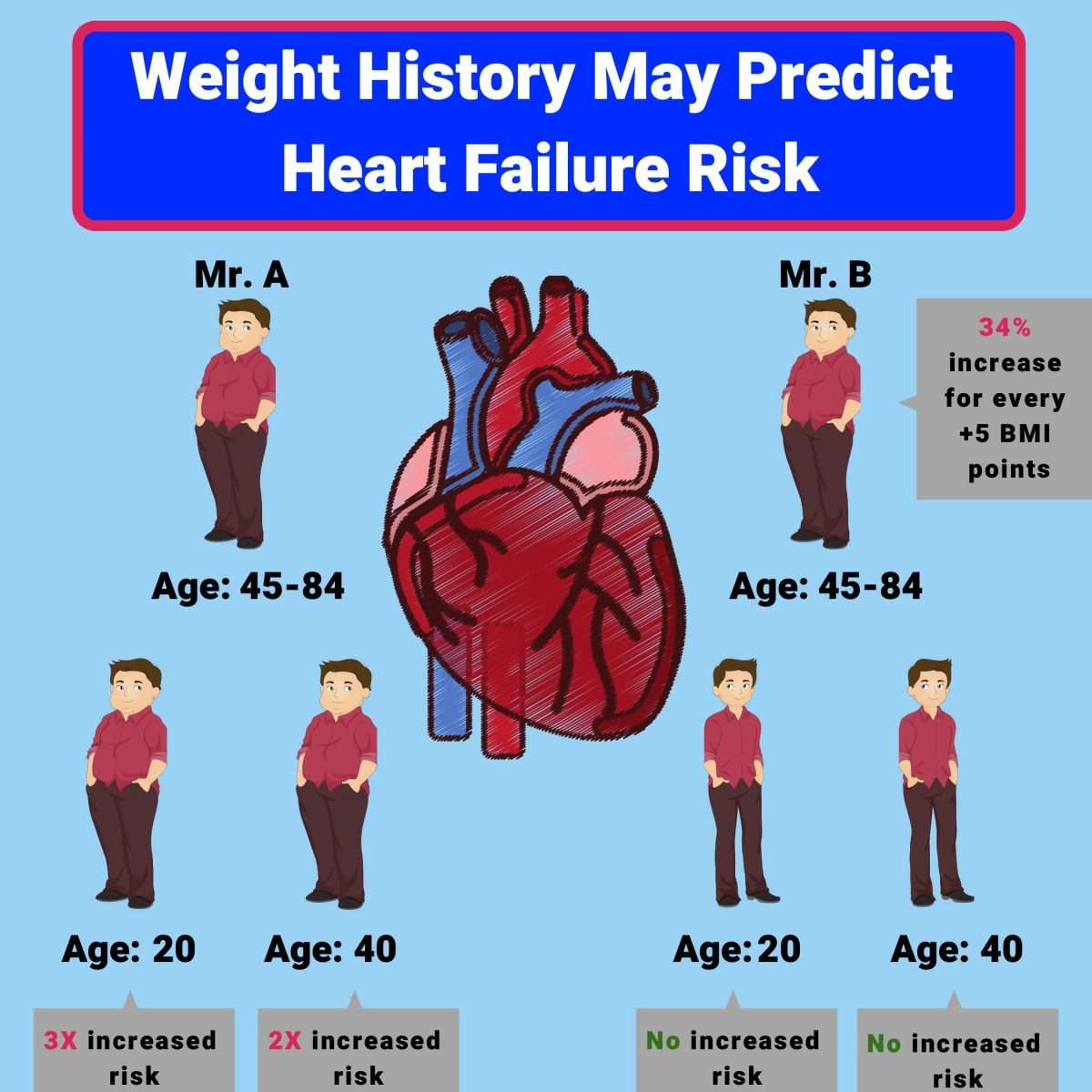
Obesity And The Heart
An obese person requires a heart that is able to pump greater amounts of blood, so the chamber sizethe actual cavity of the heartenlarges, and the muscle gets thicker as well, says Lisa de las Fuentes, MD, a Washington University cardiologist. Over time in some individuals, the heart cannot compensate, and after a while, it begins to lose some of its ability to relax or its ability to pump blood to the rest of the body. Both can lead to heart failure.
De las Fuentes says it was important to evaluate whether moderate weight loss could improve heart health. When the study began, about one-third of the patients were being treated for high blood pressure. .
Hypertension, or high blood pressure, is a huge public-health problem in the United States, says cardiologist Victor Dávila-Román, MD, director of the Cardiovascular Imaging and Clinical Research Core Laboratory at Washington University. Of the 65 million people with hypertension, between 25 percent and 50 percent have some evidence that their heart has been affected, so the presence of high blood pressure in so many of these subjects suggested that we needed to take steps to help them lower their blood pressure if we hoped to make their hearts healthier.
Individuals in the study were instructed to eat either low-fat or low-carbohydrate diets about 1,200 to 1,500 calories per day for women and 1,500 to 1,800 for men.
Small Changes Make A Big Impact
The influence of body weight on heart disease is not one to be taken casually. Being overweight can have serious and far-reaching consequences for the health of your heart and the likelihood of developing other seriously.
However, even a small weight loss can reduce the risk factors significantly. Losing weight not only involves filling your diet with nutritious foods, but it also means creating a calorie deficit.
This deficit doesnt have to be extreme to see significant weight loss. Reducing daily calorie intake by 500 calories, while increasing the general activity level to at least 90 minutes a day can be an effective way to bring the weight down to a healthier level.
Read Also: Can Congestive Heart Failure Be Cured
Questions To Ask Your Doctor
- What is the likely cause of my heart failure?
- How serious is my condition?
- How will my life change now that we know I have heart failure?
- How will I know if my condition is getting worse? When should I contact you or seek treatment?
- What is the best treatment option for me? Will I need medicine? Surgery?
- What are the side effects of the medicines used to treat heart failure?
- Will I need a heart transplant?
- Is it safe for me to exercise? What kind of exercise should I do?
- Should I make any lifestyle changes at home to reduce my risk of complications?
When To Get Medical Advice
See your GP if you experience persistent or gradually worsening symptoms of heart failure.
The symptoms can be caused by other, less serious conditions, so it’s a good idea to get them checked out.
Call 999 for an ambulance or go to your nearest accident and emergency department as soon as possible if you have sudden or very severe symptoms.
This is a medical emergency that may require immediate treatment in hospital.
Page last reviewed: 19 May 2022 Next review due: 19 May 2025
Recommended Reading: Where Does Oxygenated Blood Enter The Heart
If I Have Obesity How Do I Reduce My Risk Of Heart Disease
Losing 5% to 10% of your weight can lower your risk factors for heart disease. Small lifestyle changes can help improve metabolic syndrome, which lessens your heart disease risk. These changes include:
- Aerobic exercise: 150 minutes a week of aerobic exercise can help reduce abdominal fat and overall obesity. That works out to 30 minutes of activity, five days a week. Choosing activities that you enjoy, such as brisk walking, dancing or swimming, can help you stay motivated.
- Dietary changes: Eating fewer calories can help reduce abdominal fat. Changing your diet can also help you lose weight and improve overall obesity. There are studies that support recommending the Mediterranean diet to help reduce your risk of heart attack and death related to heart problems. This diet includes eating mostly plant-based foods such as root and green vegetables, fresh fruits, legumes, nuts and whole grains, plus moderate servings of dairy, eggs, fish, lean poultry and seafood.
What other steps can I take to reduce my risk of heart disease?
Besides lifestyle changes, other options to help reduce your risk of heart disease include:
See your healthcare provider to come up with a plan for your weight loss that makes the most sense for you.
A note from Cleveland Clinic
Nutrition Guide For Heart Failure
Following a low-sodium diet and drinking less fluid can help you feel better and allow your heart failure medicines to work better. A low-sodium diet may even keep you out of the hospital. It is not an easy diet to follow. You may find eating with heart failure is a bit of a balancing act. While you dont want to eat too much of high sodium foods, you have to be sure to eat enough to maintain good nutrition.
Nutrition and Heart Failure
The recommended salt intake is 2,000 mg of sodium per day.
Salt is a mineral that is made of sodium and chloride. It is found in food, table salt and sea salt. Sodium acts like a sponge and makes the body hold water.
Eating too much sodium when you have heart failure can cause fluid buildup in your legs, stomach and lungs and force you heart to work harder.
Most of the sodium we eat is hidden in foods. Even food that does not taste salty can contain a lot of sodium.
You should restrict the amount of sodium you eat to 2,000 mg or less each day. Try to keep the sodium content of each meal to less than 600 mg. This helps spread out your sodium intake over the day to prevent excessive fluid retention.
You can take a few basic steps to reduce the amount of sodium in your diet:
- Dont add salt when you cook or at the table
- Learn to read food labels
- Choose more foods that are lower in sodium
- Limit high sodium foods
Reading a Food Label for Sodium
Follow these easy steps to read the label:
Low-Sodium Foods
Read Also: Congestive Heart Failure And Personality Changes
