What Is Congestive Heart Failure
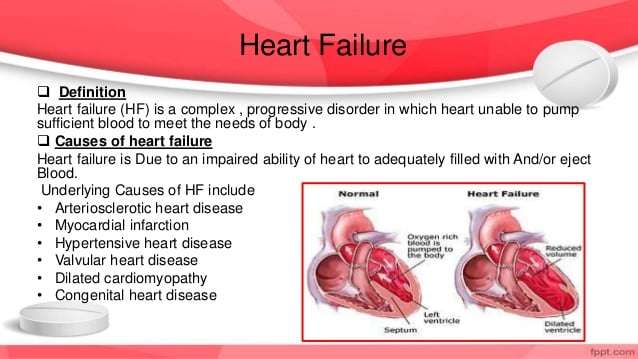
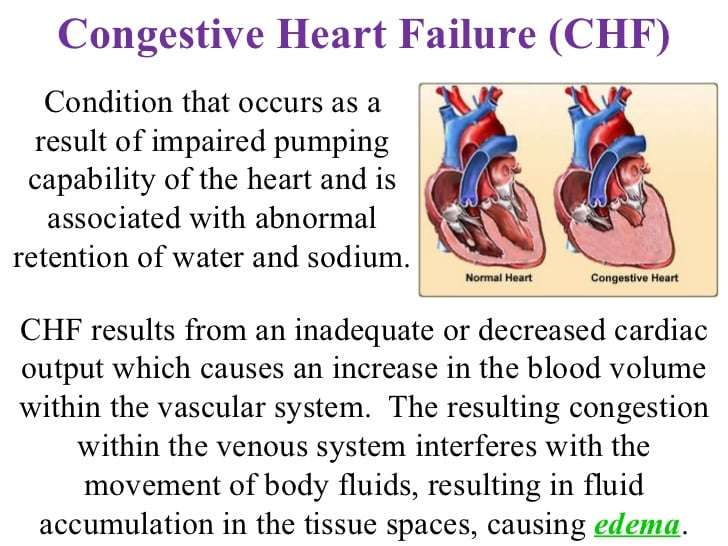
Congestive heart failure is a complex, progressive condition in which the heart does not pump enough blood to the rest of the body.
The heart chambers that pump blood out are called the ventricles. The right ventricle pushes blood into the lungs where it picks up oxygen. The left ventricle pushes oxygenated blood out to the rest of the body to supply cells and tissues with needed oxygen. Congestive heart failure is largely a condition of the left ventricle, but the right ventricle might also be affectedusually as a result of left ventricular dysfunction.
Left-sided heart failure is further classified into one of two categories. Heart failure with reduced ejection fraction, or systolic heart failure, means the ventricle is failing to contract sufficiently to pump enough blood out. Left-sided heart failure with preserved ejection fraction, or diastolic heart failure, describes conditions in which the ventricle is too stiff to sufficiently relax when they fill with blood, resulting in too little blood in the ventricle to pump out.
Congestive heart failure develops as blood flow out of the heart slows, resulting in blood flow back to the heart to become backed up. It can be caused by any number of conditions affecting the heart muscle, heart valves, blood vessels, or metabolism, including
- Heart attack
- Heart valve disease
- High triglycerides
Aside from the progressive worsening of heart function, congestive heart failure can produce many life-threatening complications such as
How Often Should You Visit Your Doctor If You Have Congestive Heart Failure
How often you need to see your doctor depends on the severity of your heart failure. You may be under the care of both a general cardiologist in addition to a heart failure specialist.
People with mild to moderate symptoms can see their doctor two to three times a year. Those with more severe symptoms may need to see their doctor every month. Those who are very unstable may need the care of a nurse daily.
Related Resources For Congestive Heart Failure
- 24 Hours, 7 Days a Week
* Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price.
Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
This article is not medical advice. It is intended for general informational purposes and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
Also Check: Can Spiders Have Heart Attacks
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the “Stages of Heart Failure.” These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
What Are Some Congestive Heart Failure Treatment Options
Your treatment plan for congestive heart failure can consist of lifestyle changes, medications, and in advanced cases surgery.
Medications. This is the primary congestive heart failure treatment and can include:
Surgery and other procedures. If you dont respond to medications or the medications arent effective, surgery or other procedures may be required to manage your CHF. These procedures include:
Recommended Reading: How To Increase Resting Heart Rate
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
What Medications Are Available To Improve Heart Function
Although diuretics are the first-line agents for congestive heart failure, digoxin is first-line in people who also have atrial fibrillation.
According to Medscape, digoxin produces a small improvement in cardiac output by strengthening the heart muscles. Side effects of digoxin can be serious if dosing is too high.
According to Uptodate, digoxin poisoning can result in life-threatening cardiac arrhythmias, nausea, vomiting, abdominal pain, confusion, delirium, weakness, and electrolyte imbalances.
Don’t Miss: Can Your Heart Rate Be Too Low
Is There A Treatment For Heart Failure
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are to try to keep it from getting worse , to ease symptoms, and to improve quality of life.
Some common types of medicines used to treat it are:
- ACE inhibitors
- Aldosterone antagonists
- ARBs
- ARNIs
- Selective sinus node inhibitors
- Soluble guanylate cyclase stimulator
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. It usually includes workouts that are designed just for you, education, and tips to lower your chance of heart trouble, like quitting smoking or changing your diet.
Cardiac rehab also offers emotional support. You can meet people like you who can help you stay on track.
Congestive Heart Failure In Dogs
Simon Swift
MA, VetMB, CertSAC, DECVIM-CA , MRCVS
After qualifying from Cambridge University, Dr. Swift spent 2 years in mixed practice before moving to a specialist small animal practice in the Northwest of England. He developed an interest in cardiology, taking the RCVS cardiology certificate in 1990. He became a partner in a large emergency and referral hospital building up the cardiology referral service until he left in 2005 to follow an alternative residency program at Liverpool University. Since becoming a European Diplomate in cardiology, he worked in a private referral hospital before moving to Florida to join the College of Veterinary Medicine as Clinical Associate Professor. He is service chief for cardiology and has recently been appointed medical director. He has been involved in breeding programs and the treatment of degenerative valvular disease especially in the cavalier King Charles spaniel having been adviser to the UK CKCS club for 20 years and more recently has helped develop advanced interventional techniques at the University of Florida.
STAGE
A: A dog at risk of heart disease
B1: Signs of heart disease . The dog is asymptomatic.
B2: Signs of heart disease . The dog is asymptomatic.
C: Congestive heart failure is present or has been present and the dog is receiving treatment.
D: Congestive heart failure is present and refractory to standard therapies. The patient requires hospitalization.
Also Check: What Is A Normal Heart Rate For A Pregnant Woman
Work With Your Doctor
Keep everyone on your health care team in the loop about the drugs and supplements you take. This keeps your risk low. Itâs also a good idea to limit any drugs or supplements you donât need. Some tips:
- At each doctor visit, provide a list of each drug and supplement you take. Include the dose and how often you take it.
- Ask your doctor if there are any medications you can limit or stop taking.
- If you have multiple doctors, ask one to be in charge of your medications. Update them when you get a new prescription or when one of your prescriptions changes. That way youâll know about any increased heart risk before you make a medication change.
Show Sources
Doses Of Investigational Drugs In Phase Iii Clinical Trials
While target doses of the investigational agent are specified per protocol in phase III trials and generally achieved in the majority of patients, there are some patients who are unable to tolerate such doses . The Studies of Left Ventricular Dysfunction Prevention trial in asymptomatic patients with an EF 35% targeted 20 mg but achieved only 12.7 mg daily of enalapril. Inability to reach target dose was driven by dizziness, cough, and hypotension. The SOLVD Treatment trial demonstrated a significant reduction in mortality with enalapril after achieving 16.6 mg daily dose while targeting 20 mg daily, a dose that was achieved in less than half the participants. Side effects were reported in 87% of the patients with enalapril, but high rates of side effects were also reported with placebo . Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart failure showed a mortality reduction of 31% when targeting 200 mg/day. This was achieved in 64% of patients and the mean dose was 159 mg/day. In the Carvedilol Prospective Randomized Cumulative Survival Study trial, 4 in 5 patients were able to reach the target dose of 50mg daily. Further, side effects reported with carvedilol were actually significantly less than those reported with placebo.
Don’t Miss: How Often Are Heart Attacks Fatal
How Much Alcohol Can You Drink If You Have Congestive Heart Failure
Alcohol increases the risk of high blood pressure, which can exacerbate congestive heart failure. Therefore, people with congestive heart failure should drink alcohol in moderation.
The American Heart Association recommends limiting alcohol to 1 drink per day for women and 1-2 drinks per day for men.
Medications Can Contribute To And Exacerbate Congestive Heart Failure
While medications play an important role in improving heart function and prolonging the lives of those with CHF, medications can have the opposite effect. Mayo Clinic notes that some diabetes medications, nonsteroidal anti-inflammatory drugs , anesthesia medications, and those used to treat high blood pressure, cancer, blood conditions, irregular or abnormal heartbeats, nervous system diseases, mental health conditions, lung and urinary problems, inflammatory diseases, and infections have been found to increase the risk of heart failure and heart problems.
Also Check: What Is A Normal Heart Rate
Diagnosis Of Congestive Heart Failure In Dogs
While a cage-side echocardiogram can provide support for a diagnosis of CHF if needed, the stress of a full echocardiogram could further decompensate the patient without providing additional information.
Thoracic radiographs often confirm the diagnosis of left-sided CHF but should be postponed if the patient is unstable . Radiographic cardiomegaly can be documented, and the presence of an interstitial/alveolar pattern centered on the perihilar region, consistent with pulmonary edema, confirms the diagnosis of CHF. While dilated pulmonary veins can be suggestive of left heart failure, in acute cases, it is not uncommon for these to be normal in size.
FIGURE 1. Lateral and dorsoventral thoracic radiographs of an 8-year-old Doberman pinscher with DCM in CHF. Note the cardiomegaly with a straightened caudal border, prominent left atrium, and tracheal elevation. There is a diffuse alveolar/interstitial pattern in the lung fields with air bronchograms and dilated pulmonary veins.
The clinical signs and history can also help in increasing the clinical suspicion of CHF. Sympathetic stimulation associated with heart failure should cause tachycardia, while cough and crackles are nonspecific signs.
Deprescribing Should Also Play A Valuable Role
Another important facet of medication management for heart failure patients is safe, appropriate deprescribing. Deprescribing is “the planned and supervised process of dose reduction or stopping of medication that might be causing harm, or no longer be of benefit,” according to the informative website Deprescibing.org. The site continues, stating, “Deprescribing is part of good prescribing backing off when doses are too high, or stopping medications that are no longer needed.”
As we note in the aforementioned Cureatr blog post concerning polypharmacy, “Lack of deprescribing can indirectly contribute to polypharmacy when opportunities to safely eliminate medications immediately or via gradual reduction are missed.”
Deprescribing in older adults with cardiovascular disease was the subject of research in 2019 in the Journal of the American College of Cardiology. The authors grouped common triggers to consider deprescribing into four categories:
- Adverse drug reactions
- Prescribing cascades
- End of life and as part of palliative care
The authors include the following in their conclusion: “The cardiovascular clinical team must recognize, particularly in reference to older adults, that deprescribing is an important resource that can improve clinical care and enhance quality of life.”
You May Like: Which Areas Of The Heart Contract To Circulate Blood
Can Surgery Be Used To Treat Heart Failure
In heart failure, surgery may sometimes prevent further damage to the heart and improve the heart’s function. Procedures used include:
- Coronary artery bypass grafting surgery. The most common surgery for heart failure caused by coronary artery disease is . Although surgery is more risky for people with heart failure, new strategies before, during, and after surgery have reduced the risks and improved outcomes.
- Heart valve surgery. Diseased heart valves can be treated both surgically and non-surgically .
- Implantable left ventricular assist device . The LVAD is known as the “bridge to transplantation” for patients who haven’t responded to other treatments and are hospitalized with severe systolic heart failure. This device helps your heart pump blood throughout your body. It allows you to be mobile, sometimes returning home to await a heart transplant. It may also be used as destination therapy for long-term support in patients who are not eligible for transplant.
- Heart transplant. A heart transplant is considered when heart failure is so severe that it doesn’t respond to all other therapies, but the person’s health is otherwise good.
How Common Is Chf
Its estimated that about 6.5 million Americans have heart failure. That number is expected to rise dramatically in the next decade as the population gets older. The lifetime risk of getting heart failure is 20% for all Americans older than 40 years of age. Over 650,000 new cases of heart failure are diagnosed each year.
Don’t Miss: Where Is The Heart Attack Grill
What Are The Most Common Side Effects Of Congestive Heart Failure Medications
As with all medicines, those used for congestive heart failure will have some side effects, depending on the class you are taking:
- ACE inhibitors and ARBs can commonly cause low blood pressure, headache, dizziness, and high blood potassium levels. ACE inhibitors are also notorious for a dry and often bothersome cough that recent studies show may develop in around 10% of the patients on them. In half of these patients, the ACE inhibitor has to be discontinued. ARBs also carry the risk of a cough but it is significantly lower than that related to ACE inhibitors.
- Diuretics increase the amount of water and salt your body gets rid of so you commonly see electrolyte imbalances, dehydration, dizziness, and fatigue.
- Beta-blockers can cause low blood pressure, low heart rate, headache, fatigue, and dizziness.
- Meds that contain a vasodilator like BiDil commonly cause flushing, low blood pressure, and headache.
- Verquvo is a newer class of medication called soluble guanylate cyclase stimulators. It can cause birth defects so pregnancy should be ruled out before starting this medication. It can commonly cause low blood pressure and anemia.
Pharmacists Should Take The Lead On Chf Medication Management
Considering the complexity of medication management for congestive heart failure patients everything from multiple medications prescribed for CHF and other conditions the risks associated with these medications the importance of performing medication reconciliation at every transition of care, including post-discharge the value of executing appropriate deprescribing and other essential steps the member of the patient’s healthcare team in the best position to take the lead on CHF medication management is undoubtedly the pharmacist.
We recently discussed how pharmacists improve medication management during care transitions, highlighting such factors as a pharmacist’s medication expertise, access to more detailed and complete drug information, and proper completion of med rec and MRP. Meanwhile, a recent column in Pharmacy Times explained why pharmacists are so well-suited to polypharmacy management of CHF patients, with the authors noting, “The complexity of CHF management provides many opportunities for pharmacists to adopt impactful roles in these patients’ lives through medication therapy management, patient education, interdisciplinary collaboration, and coordinated transition of care.”
Read Also: How Did Bob Harper Have Heart Attack
How Is Congestive Heart Failure Diagnosed
Congestive heart failure is diagnosed primarily from a history and a physical examination. A primary care physician may be the first healthcare professional to recognize symptoms during a routine physical, but a cardiologist will make the final diagnosis.
A medical history will help identify risk factors such as high blood pressure, smoking, obesity, lack of exercise, and diabetes. Be prepared to answer questions like:
- Is there a family history of congestive heart failure?
- Are you short of breath?
- Have you been fatigued or unable to do physical work?
- If you have swelling or edema, when did it start?
- Have you had chest pain?
Research has shown that the most accurate indicators of heart failure are physical symptoms, so a physical exam is the most important diagnostic tool. Symptoms are due to either reduced heart pumping volume or swelling and fluid retention . Heart failure symptoms include:
- Shortness of breath especially when lying down
- Weakness
- Nausea
- Lowered appetite
The doctor will also take your pulse and listen to the heart to identify distinctive symptoms of heart failure:
- Alternating weak and strong pulse
- A shift in the location of the maximum pulse that can be felt on the chest surface
- Presence of a brief vibration that can be heard through a stethoscope as one of the ventricles fills with blood, called the S3 gallop
In addition to a physical exam, the cardiologist will use tests to confirm the diagnosis:
Treatment will depend on the conditions stage.
