What Are The Advantages Of Heart Valve Surgery
Heart valve surgery can ease your symptoms, improve your life expectancy and help prevent death.
The potential advantages of heart valve repair vs. valve replacement are:
- Lower risk of infection.
- Less need for lifelong anticoagulant medication.
Valve surgeries, including valve repair and valve replacement, are the most common minimally invasive procedure.
The benefits of minimally invasive surgery include:
- Lower risk of infection.
- Other medical conditions you have.
- How many procedures you have in a single operation.
Your cardiologist and surgeon will talk to you about these risks before your surgery.
If youve had a valve fixed or replaced, you may be at a higher risk of getting infective endocarditis. But this can also happen with a faulty valve that isnt repaired. In certain cases, your healthcare provider may prescribe antibiotics to keep you from getting endocarditis from some types of dental work. You can reduce the risk of endocarditis yourself by taking good care of your teeth.
Indications For Mitral Valve Replacement
Mitral valve replacement is an accepted surgical procedure for patients with severe MS who are not candidates for surgical commissurotomy or percutaneous mitral valvotomy. The risk of MVR is dependent on multiple factors, including functional status, age, LV function, cardiac output, concomitant medical problems, and concomitant CAD. In the young, healthy person, MVR can be performed with a risk of < 5%. However, in the older patient with concomitant medical problems or pulmonary hypertension at systemic levels, the risk of MVR may be 10% to 20%.
Antithrombotic Treatment For Surgical Valve Repair At The University Hospitals Leuven
Surgically repaired valves are much less thrombogenic compared to surgical valve replacement. Aortic valve repair is technically demanding and is mostly performed in expert centers. The population is young with few co-morbidities. In patients without OAC indication, low-dose aspirin is recommended during the first 3 months postoperatively. With an indication for OAC, oral anticoagulants are continued. NOACs are the first choice unless there is a clear, pre-existing indication for VKAs.
You May Like: What The Symptoms Of Heart Attack
H Valvular Heart Disease Associated With Anorectic Drugs
In the summer of 1997, the association between anorexigens and valvular heart disease was reported in 24 patients receiving the drug combination of fenfluramine and phentermine unusual valve morphology and associated regurgitation were identified in both left- and right-sided heart valves. The echocardiographic and histopathologic findings were similar to those described in patients with carcinoid or ergotamine-induced valvular heart disease. All 24 patients were symptomatic and had heart murmurs thus, the frequency of valvular pathology in asymptomatic patients receiving the combination of fenfluramine-phentermine could not be determined. The FDA has reported 5 echocardiographic prevalence surveys in which 86 of 271 patients who received a combination of fenfluramine and phentermine for 6 to 24 months had evidence of significant AR and/or MR, as did 6 of 20 patients who received dexfenfluramine with or without phentermine.
In addition to the uncertainties regarding the prevalence of valvular disease in patients receiving combination or single-drug therapy, the natural history of the valve disease during anorectic drug treatment and after drug withdrawal is unknown and awaits further clinical investigation. Thus, the risk of valvular heart disease relative to the benefit of weight reduction in patients with morbid obesity is unknown.
Recommendations For The Management Of Patients After Heart Valve Surgery
@article, author=rwolf and Manuel J. Antunes and Pilar Tornos and Raffaele de Caterina and Bertrand Cormier and Bernard D. Prendergast and Bernard Iung and Hans Halvor Bjrnstad and Catherine Leport and Roger J. C. Hall and Alec Vahanian}, journal=, year=, volume=, pages=}
- European heart journal
- View 1 excerpt, cites background
- View 1 excerpt, cites background
- Indian Journal of Thoracic and Cardiovascular Surgery
- View 4 excerpts, cites methods and background
- View 9 excerpts, cites background
- Interactive cardiovascular and thoracic surgery
- Interactive cardiovascular and thoracic surgery
- The Journal of heart valve disease
You May Like: Congestive Heart Failure In Dogs Life Expectancy
Esc/eacts Guidelines For The Management Of Valvular Heart Disease
ESC Committee for Practice Guidelines and National Cardiac Societies document reviewers listed in the Appendix.
Representing the European Association for Cardio-Thoracic Surgery .
European Heart JournalEuropean Heart Journal
Other Transcatheter Techniques: Percutaneous Edge
Edge-to-Edge Mitral Repair
Besides TAVI, percutaneous edge-to-edge repair with MitraClip⢠has now become an established technique in transcatheter heart valve interventions. The EVEREST II and the COAPT trial demonstrated the safety and efficacy of transcatheter mitral valve repair with MitraClip⢠in well-selected patients with moderate or severe mitral regurgitation . So far, the antithrombotic policy after MitraClip⢠has been based on expertise. In the EVEREST II trial, patients receiving MitraClip⢠were treated with aspirin, 325 mg/day, for 6 months and clopidogrel, 75 mg/day, for 30 days . In the COAPT trial, standard regimen included aspirin, 81 mg/day, and/or clopidogrel, 75 mg/day, for 6 months or longer . In patients with chronic OAC, OAC was continued without the systematic addition of antiplatelet therapy .
Future Perspective
Don’t Miss: How To Tell Heart Attack
How To Use These Guidelines
The Committee emphasizes that many factors ultimately determine the most appropriate treatment in individual patients within a given community. These factors include the availability of diagnostic equipment, the expertise of cardiologists and surgeons, especially in the field of valve repair and percutaneous intervention and, notably, the wishes of well-informed patients. Furthermore, owing to the lack of evidence-based data in the field of VHD, most recommendations are largely the result of expert consensus opinion. Therefore, deviations from these guidelines may be appropriate in certain clinical circumstances.
Management Of Patients After Valvotomy Or Commissurotomy
Recurrent symptoms after successful surgical commissurotomy have been reported to occur in as many as 60% of patients after 9 years, but recurrent stenosis accounts for symptoms in < 20%. In patients with adequate initial results, progressive MR and development of other valvular or coronary problems are more frequently responsible for recurrent symptoms. Thus, in patients presenting with symptoms late after commissurotomy, a comprehensive evaluation is required to look for other causes of the symptoms. Patients undergoing percutaneous mitral valvotomy have a higher incidence of recurrent symptoms at 1- to 2-year follow-up if there was an unfavorable mitral valve morphology due to either an initial inadequate result or restenosis.
Repeat percutaneous balloon valvotomy can be performed in the patient who has restenosis after either a prior surgical commissurotomy or balloon valvotomy. The results of these procedures are less satisfactory than the overall results of initial valvotomy because there is usually more valve deformity, calcification, and fibrosis than with the initial procedure. MVR should be considered in those patients with recurrent severe symptoms and severe deformity of the mitral apparatus.
Don’t Miss: What Should Your Target Heart Rate Be
Acc/aha Joint Committee Members
Patrick T. OGara, MD, MACC, FAHA, Chair
Joshua A. Beckman, MD, MS, FAHA, Chair-Elect
Glenn N. Levine, MD, FACC, FAHA, Immediate Past Chair
Sana M. Al-Khatib, MD, MHS, FACC, FAHA
Anastasia Armbruster, PharmD, AACC
Kim K. Birtcher, PharmD, MS, AACC
Joaquin Ciggaroa, MD, FACC
Anita Deswal, MD, MPH, FACC, FAHA
Dave L. Dixon, PharmD, FACC
Lee A. Fleisher, MD, FACC, FAHA
Lisa de las Fuentes, MD, MS, FAHA, FASE
Federico Gentile, MD, FACC
Zachary D. Goldberger, MD, MSc, FACC, FAHA
Bulent Gorenek, MD, FACC, FESC
Norrisa Haynes, MD, MPH
Adrian F. Hernandez, MD, MHS
Mark A. Hlatky, MD, FACC, FAHA
José A. Joglar, MD, FACC, FAHA
W. Schuyler Jones, MD, FACC
Joseph E. Marine, MD, FACC
Daniel Mark, MD, MPH, FACC, FAHA
Latha Palaniappan, MD, MS, FAHA, FACC
Erica S. Spatz, MD, MHS, FACC
Jacqueline Tamis-Holland, MD, FACC
Duminda N. Wijeysundera, MD, PhD
Y. Joseph Woo, MD, FAHA, FACC
Former Joint Committee member current member during the writing effort.
Iii Specific Valve Lesions
A. Aortic Stenosis
Grading the Degree of Stenosis
The aortic valve area must be reduced to one fourth its normal size before significant changes in the circulation occur. Because the normal adult valve orifice is 3.0 to 4.0 cm2, an area 0.75 to 1.0 cm2 is usually not considered severe AS. In large patients, a valve area of 1.0 cm2 may be severely stenotic, whereas a valve area of 0.7 cm2 may be adequate for a smaller patient.
The committee used a variety of hemodynamic and natural history data to grade the degree of AS as mild , moderate , or severe . When stenosis is severe and cardiac output is normal, the mean transvalvular pressure gradient is generally > 50 mm Hg. Some patients with severe AS remain asymptomatic, whereas others with only moderate stenosis develop symptoms. Therapeutic decisions, particularly those related to corrective surgery, are based largely on the presence or absence of symptoms. Thus, the absolute valve area is not usually the primary determinant of the need for aortic valve replacement .
An ejection systolic murmur may be heard in the presence of a normal valve, one that is thickened and minimally calcified, and one that is stenotic. The 3 conditions must be distinguished.
Natural History
Management of the Asymptomatic Patient
Indications for Cardiac Catheterization
Indications for Aortic Valve Replacement
1. Symptomatic Patients.
2. Asymptomatic Patients.
3. Patients Undergoing Coronary Artery Bypass Surgery.
Aortic Balloon Valvotomy
Read Also: Recovery After Heart Surgery
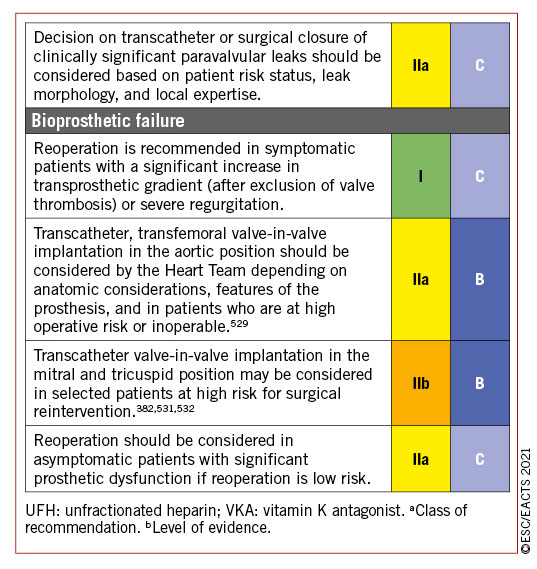
Choice Of Prosthetic Valve
The choice between a mechanical and a biological valve in adults is determined mainly by estimating the risk of anticoagulation-related bleeding and thromboembolism with a mechanical valve versus the risk of structural valve deterioration with a bioprosthesis and by considering the patients lifestyle and preferences. Rather than setting arbitrary age limits, prosthesis choice should be discussed in detail with the informed patient, cardiologists and surgeons, taking into account the factors detailed below . Bioprostheses should be considered in patients whose life expectancy is lower than the presumed durability of the bioprosthesis, particularly if comorbidities may necessitate further surgical procedures, and in those with increased bleeding risk. In women who wish to become pregnant, the high risk of thromboembolic complications with a mechanical prosthesis during pregnancy and the low risk of elective reoperation are incentives to consider a bioprosthesis, despite the rapid occurrence of structural valve deterioration in this age group.
Choice of the aortic/mitral prosthesis in favour of a mechanical prosthesis the decision is based on the integration of several of the following factors
Purpose Of The Executive Summary
This executive summary of the valvular heart disease guideline provides a synopsis with algorithms to guide clinicians in the screening, diagnosis, and management of patients with VHD. Tables and figures that are mentioned in this executive summary, but are not included here, appear in the full guideline .
The full guideline has been updated with new evidence and provides newer options for diagnosis and treatment of VHD. This summary includes only the recommendations from the full guideline which focus on diagnostic work-up, the timing and choice of surgical and catheter interventions, and recommendations for medical therapy. The reader is referred to the full guideline document for graphical flow charts, text, and tables with additional details about the rationale for and implementation of each recommendation, and the evidence tables detailing the data considered in developing these guidelines.
Also Check: Final Stages Of Diastolic Heart Failure
Can A Heart Valve Repair Itself
No, a heart valve cant repair itself. Valve disease doesnt go away. It gets worse with time. As the disease gets worse, youll have more symptoms and your overall health will suffer. These changes often happen slowly, but they can also occur very quickly.
Depending on the type and extent of valve disease you have, you may be able to take medication for the short term. Surgery is the only effective long-term solution, and your healthcare provider will help determine when its time to pursue that option.
Will I Need To Take Blood
The need for anticoagulant medication after surgery depends on the type of surgery you have. The medication prevents blood clots from forming and causing problems with your heart valve. Currently, warfarin is the only approved blood thinner for mechanical heart valves.
If you have a mechanical heart valve, youll need to take this medication for the rest of your life.
If you have valve repair or a biological valve replacement, you may need to take this medication for several weeks after surgery, or maybe not at all.
You may need to take an anticoagulant for a condition not related to your heart valves. This medication also treats:
- An irregular heartbeat.
Recommended Reading: Do All Heart Attacks Damage The Heart
Concept Of The Heart Team And Heart Valve Centres
The main purpose of heart valve centres as centres of excellence in the treatment of VHD is to deliver better quality of care. This is achieved through greater volumes associated with specialization of training, continuing education and clinical interest. Specialization will also result in timely referral of patients before irreversible adverse effects occur and evaluation of complex VHD conditions. Techniques with a steep learning curve may be performed with better results in hospitals with high volumes and more experience. These main aspects are presented in Table .
A heart valve centre should have structured training programmes. Surgeons and cardiologists performing any valve intervention should undergo focused training as part of their basic local board certification training. Learning new techniques should take place through mentoring to minimize the effects of the learning curve.
Transcatheter Aortic Valve Implantation
As the prevalence of severe aortic stenosis increases with age, there is a growing interest in minimally invasive valve replacement techniques for fragile patients with multiple co-morbidities who are not suitable for surgery. After two decades of technological refinement, TAVI is now an established treatment for patients with severe symptomatic aortic stenosis at high or intermediate surgical risk . Recent studies have also shown that TAVI is a valid alternative for surgical aortic valve replacement in low risk groups .
As with surgical prosthetic heart valves, thromboembolic and bleeding complications are an important concern after TAVI and uncertainty regarding the optimal antithrombotic strategy remains. Despite antithrombotic treatment with DAPT or OAC, the incidence of stroke remained 4.1 and 7.0% at 30 days and 1 year after the procedure, respectively . The rate of major bleeding amounts to 10.2% during the first 30 days and rises to 16.0% in the 1st year, reflecting the frailty of TAVI patients .
Many TAVI patients have an indication for longstanding OAC. Approximately 40% of patients have associated atrial fibrillation and up to 15% develop new-onset atrial fibrillation after TAVI . Consequently, a stratification according to the need for OAC is recommended in the choice of antithrombotic therapy.
Without Indication for Oral Anticoagulation
With Indication for Oral Anticoagulation
Role of NOACs: Ongoing Trials
Also Check: Heart Rate Svt
Antithrombotic Treatment For Mechanical Valves At The University Hospitals Leuven
All mechanical valves that are currently being implanted at the University Hospitals Leuven are bileaflet valves. After aortic valve replacement the standard target INR ranges from 2.0 to 2.5. In patients with an On-X aortic valve, a lower target INR of 1.5 to 2.0 in combination with low-dose aspirin can be considered from 3 months after surgery. For the mitral and tricuspid position an INR of 2.5 to 3.0 is targeted. In the presence of thromboembolic risk factors an increase of the target INR range by 0.5 can be considered: INR 2.5 to 3.0 for aortic prostheses and INR 3.0 to 3.5 for mitral and tricuspid prostheses. In case of thromboembolic events under standard VKA therapy, low-dose aspirin is associated. In patients with chronic coronary syndrome or atherosclerotic disease, we do not recommend the systematic addition of aspirin because the benefit has not been clearly demonstrated and concerns about an increased risk of bleeding remain.
Finally, few patients remain with older generation mechanical valves . These valves are no longer implanted nowadays, but given their thrombogenicity, a higher INR is targeted, and antithrombotic management needs to be individualized.
Document Review And Approval
This document was reviewed by 2 official reviewers each nominated by both the ACC and the AHA, as well as content reviewers nominated by the ACC and AHA. Authors RWI information is published in Appendix 1 of the full guideline . Reviewers RWI information is published in Appendix 2 of the full guideline .
Recommended Reading: Miracle Cure For Congestive Heart Failure
Indications For Surgical Or Percutaneous Valvotomy
With the development of cardiopulmonary bypass in the 1960s, open mitral commissurotomy and replacement of the mitral valve became the surgical procedures of choice for treatment of MS. Percutaneous mitral balloon valvotomy emerged in the mid 1980s. This procedure has become an accepted alternative to surgical approaches in selected patients. The procedure itself is technically challenging and involves a steep learning curve. There is a higher success rate and lower complication rate in experienced high-volume centers. Thus, results of the procedure are highly dependent on the experience of the operators, which must be taken into consideration when making recommendations for proceeding with this technique.
Relative contraindications to percutaneous balloon valvotomy include the presence of a left atrial thrombus and significant MR. Transesophageal echocardiography is frequently performed before the procedure to determine the presence of left atrial thrombus, specifically examining the left atrial appendage. If a thrombus is found, 3 months of anticoagulation with warfarin may result in resolution of the thrombus.
Implications To Current Practice And Future Research
While in Europe and the USA, patients following myocardial infarction and revascularisation and with heart failure can be offered CR currently, such a policy is generally not the case for patients following open aortic valve surgery and TAVI.29 To inform future practice and policy, further evidence on the impact of CR following valve surgery is needed. Future studies of exercise-based CR post open aortic valve surgery or TAVI should aim to measure outcomes and costs that are relevant to the patients, clinicians and the policy makers. The studies should also aim to minimise bias and fully report all processes carried out. This would allow a more robust systematic review to be conducted, which would help inform recommendations for CR in TAVI and SAVR patients and therefore improve current practice.
You May Like: How To Take Your Own Heart Rate
