Key Points From The New Heart Failure Guidelines
Ileana L. Piña, MD, MPH
This transcript has been edited for clarity.
Hello. I’m Ileana Piña. I have recently taken a position at Thomas Jefferson University in Philadelphia. This is my blog.
I wanted to spend a little time today talking about the heart failure guidelines. We have been waiting for the American College of Cardiology/American Heart Association, and now Heart Failure Society of America, guidelines. All three organizations have collaborated here.
It also takes into consideration the definitions of heart failure that were published in the Journal of Cardiac Failure, which is the journal of the Heart Failure Society of America. That was published over a year ago, and I think it set the stage for these guidelines.
Certainly, the Europeans published their guidelines in the summer of 2021 at about the same time as the European Society of Cardiology meeting.
We’ve all been wondering: Is it going to be the same, or are there any differences?
SGLT2 Inhibitors and ARNI
The ESC guidelines already included the sodium-glucose co-transporter 2 inhibitors, and we had a consensus statement from the American College of Cardiology showing the benefits of the SGLT2 inhibitors and including them in the basis of care.
The other thing that I am very happy about is that they really emphasize team care, and I think that’s a stronger point than has been made before. Team care is necessary to take care of the sick patients that are very complicated.
HFpEF and HFmrEF
Value of Care
How To Initiate Add Or Switch To New Evidence
Established therapies for chronic HFrEF include ARNIs, angiotensin-converting enzyme inhibitors , angiotensin receptor blockers , beta-blockers, loop diuretics, aldosterone antagonists, hydralazine/isosorbide dinitrate , and ivabradine, an If channel blocker highly selective for the sinoatrial node pacemaker current. With the exception of loop diuretics, all of these therapies have been shown in randomized controlled trials to improve symptoms, reduce hospitalizations, and/or prolong survival . Use of digoxin as a treatment for HFrEF lacks new data most of its use in modern HFrEF management focuses on its role as a rate control agent for atrial fibrillation in those with low blood pressure.
Following the publication of the 2017 ECDP focused on optimizing therapy for HFrEF, more data have emerged to support an expanded role for ARNIs in patients with HFrEF. These data include their use as a de novo therapy in some patients naive to ACEIs or ARB therapies , evidence for rapid improvement in patient-reported outcome measures , and the demonstration of a reverse-remodeling effect of ARNIs in chronic HFrEF, independent of background therapy with ACEIs/ARBs . It is not yet clear that de novo initiation is best for all patients with HFrEF , and we do recognize access challenges for some patients with regards to payer coverage and associated costs of ARNIs.
Table 1 Starting and Target Doses of Select GDMT and Novel Therapies for HF
5.1.1 Initiating GDMT
Figure 2Figure 3
New Acc Aha Hfsa Guidelines Recommend Sglt
The joint recommendations cite DAPA-HF and EMPEROR-HF as evidence of the drug class’ benefit for differing stages of heart failure.
The American College of Cardiology , American Heart Association and Heart Failure Society of America have released a joint guideline addressing updates to heart failure prevention and treatment of symptomatic disease with the emerging SGLT-2 inhibitor drug class.
The new guidelinepublished and presented during the ACC 2022 Scientific Sessions in Washington DCimplement findings from trials including DAPA-HF and EMPEROR-HF, which previously shown the benefit of SGLT-2 inhibitors dapagliflozin and empagliflozin, respectively, in reducing composite cardiovascular events and mortality in patients with heart failure with reduced ejection fraction among other cardiovascular and cardiometabolic outcomes.
Additionally, the guideline puts further emphasis on primary heart failure prevention through measures including blood pressure control and changes to high-risk patients diet and exercise. More than 120 million Americans currently have high blood pressure another 100 million are obese and 28 million have diabetes, meaning a significant rate of the US population can be categorized as at-risk for heart failureor Stage A, per the new guideline risk stages.
The 4 stages are as follows:
New symptomatic heart failure definitions at stage C from the guideline include:
Read Also: How Long Can You Have Angina Before A Heart Attack
New Heart Failure Guidelines Add 4th Drug To Treatment Regimen
Some heart failure patients may benefit from taking pills known as SGLT2 inhibitors, which are currently approved for type 2 diabetes, according to the new guidelines.
Peter Dazeley/Getty Images
People with symptomatic heart failure may be able to reduce their risk of premature death by taking a drug originally designed for type 2 diabetes, according to new treatment guidelines from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America.
Heart failure develops when weakened muscles make it harder for the heart to expand and contract to pump blood through the body. Symptoms can include shortness of breath, a persistent cough, swelling in the feet, legs and abdomen, and fatigue and nausea.
The new guidelines, published April 1 in the Journal of the American College of Cardiology, add a fourth drug to the regimen of medications already recommended to treat symptomatic heart failure patients who pump too little oxygen-rich blood out to the body with each heartbeat, a condition known as heart failure with reduced ejection fraction.
A Guideline Chair Acknowledged The New Document Is Already In Need Of An Updatea Nice Problem To Have Said Marco Metra
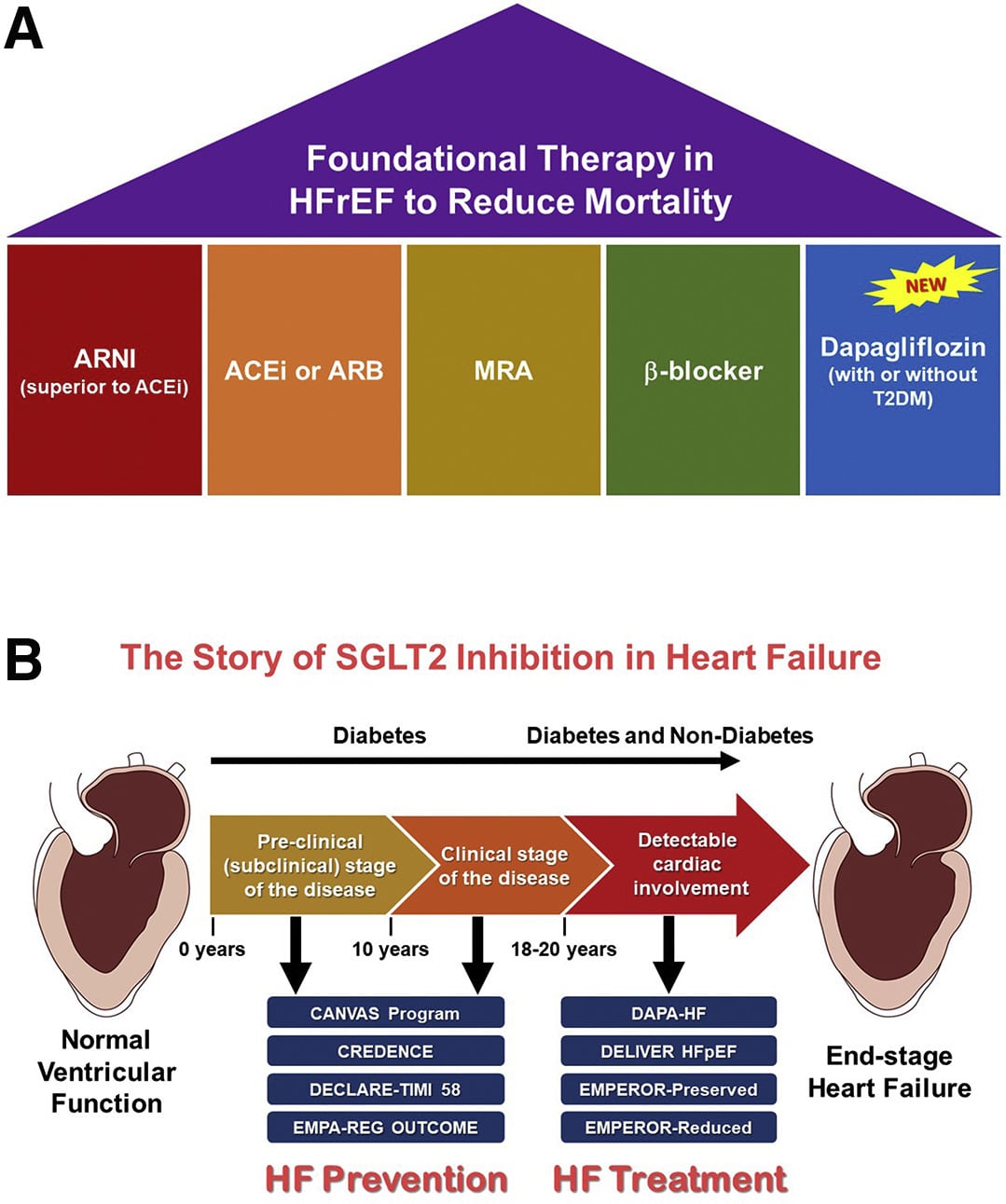
Heart failure guidelines released at the European Society of Cardiology Congress 2021 yesterday give a new class I recommendation for sodium-glucose cotransporter 2 inhibitors in the setting of HF with reduced ejection fraction , and they urge physicians to initiate all four recommended drug categoriesACE inhibitors/angiotensin receptor-neprilysin inhibitors , beta-blockers, mineralocorticoid receptor antagonists , and SGLT2 inhibitorsas swiftly and safely as possible.
This is not only a name change, but this means that patients with an ejection fraction below 50% . . . have a milder form of heart failure with the reduced ejection fraction, and this means that likely the same drugs that are used in patients with reduced ejection fraction may also be started in the patients with an ejection fraction from 41% to 50% or even maybe a little bit more, guideline co-chair Marco Metra, MD , told TCTMD. And this applies to all the drugs that are indicated for heart failure with reduced ejection fraction.
But given the timingthe guidelines were released just hours ahead of the presentation of the EMPEROR-Preserved trialthe advice, for some, is already woefully out-of-date.
Don’t Miss: Heart Attacks And Headaches
When To Refer To An Hf Specialist
Appropriate and timely referral to an HF specialist and/or HF program is essential in selected patients to optimize therapies and evaluate advanced HF care options . Referrals should be made for consultation and, if indicated, for comanagement as well as consideration of advanced therapies , recognition and management of specific or unusual cardiomyopathies, or annual review . Clinical triggers for referral include persistent or worsening symptoms, adverse clinical events, or other features suggesting that the patient is at high risk for disease progression or death .
Adding An Sglt2 Inhibitor May Be Cost Prohibitive For Some Patients
An SGLT2 inhibitor costs, on average, $500 to $600 for a 30-day supply, which may be prohibitive for some patients.11 Integration of SGLT2 inhibitors into a patients medication regimen may require dose adjustments of other medications, particularly glucose-lowering therapies, and the optimal prioritization of medications is not yet known.
Integration of SGLT2 inhibitors into a patients medication regimen may require dose adjustments of other medications.
Read Also: Signs Of Heart Attack Women
Acc Aha And Hfsa Partner To Release 2022 Heart Failure Guidelines
Released on the eve of ACC.22, the 2022 heart failure guidelines represent a collaborative effort by the ACC/AHA/HFSA and include major additions, including a new focus on the use of SGLT2 inhibitors and revisions to the ACC/AHA stages of heart failure.
The American College of Cardiology, American Heart Association, and Heart Failure Society of America have released a new joint guideline outlining evidence-based strategies for prevention, diagnosis, and management of heart failure.
One primary goal with the new guideline was to use recently published data to update our recommendations for the evaluation and management of heart failure, said Paul A. Heidenreich, MD, MS, guideline writing committee chair, in a statement from the American College of Cardiology. One focus was prevention of heart failure through optimizing blood pressure control and adherence to a healthy lifestyle.
Published on April 1, which is just a day prior to the start of the American College of Cardiologys 71st annual Scientific Session , the 159-page document broken down into 14 sections with multiple subsections and cites more than 700 reference documents. Composed by Heidenreich and a team of more than 50 fellow authors, the guideline is based on an evidence review of relevant studies and data published through September 2021.
Sglt2is In Patients With Hfref Regardless Of T2d Status
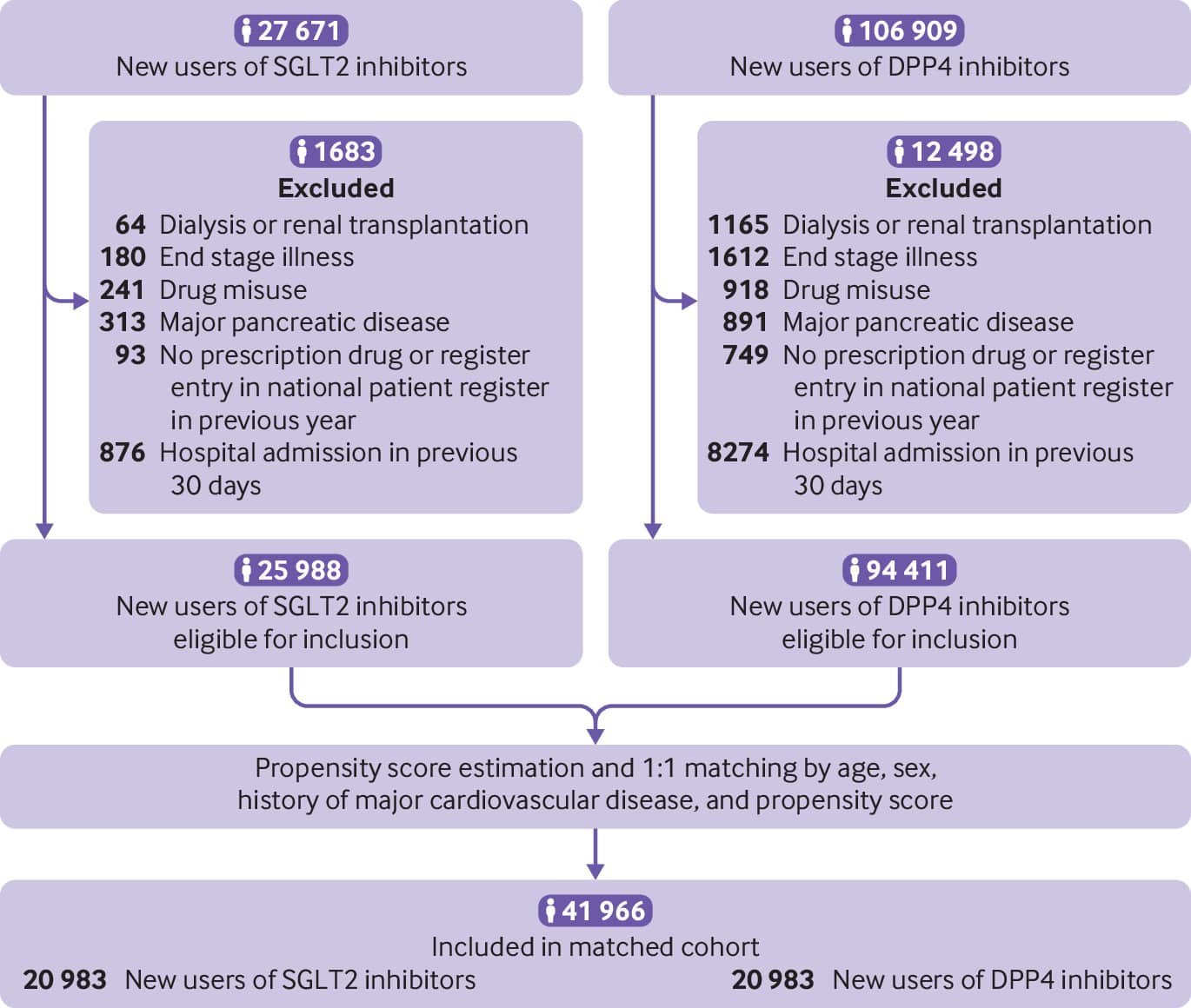
The marked effects of SGLT2is on HF outcomes in CV outcome trials, in which all patients had T2D by definition, led researchers to speculate whether these agents have a benefit in patients with HFrEF without T2D. Therefore, the effects of SGLT2is on CV outcomes among patients with and without T2D are being actively investigated, with published data available from the DAPA-HF and EMPEROR-Reduced studies .
DAPA-HF and EMPEROR-Reduced were both randomized, placebo-controlled studies that evaluated the efficacy and safety of SGLT2is plus standard HF therapy at baseline in patients with HFrEF . Both studies included a high proportion of patients without T2D . The results of both studies were remarkably consistent. In DAPA-HF, the relative risk for the primary outcome, a composite of worsening HF or CV death, was reduced by 26% with dapagliflozin versus placebo , and the secondary outcome of HHF or CV death was reduced by 25% . Similarly, the risk of HHF or CV death was 25% lower with empagliflozin than with placebo in the EMPEROR-Reduced study . Both dapagliflozin and empagliflozin reduced the risk of HHF by approximately 30% . The risk of CV death significantly decreased by 18% with dapagliflozin in the DAPA-HF study . In both studies, the effects of SGLT2is on these outcomes were observed early in the course of treatment and were similar between patients with and without T2D, suggesting a nonglycemic mechanism leading to improved CV outcomes .
You May Like: Which Shoulder Hurts Heart Attack
Sodiumglucose Cotransporter 2 Inhibitor
The SGLT2 inhibitors dapagliflozin and empagliflozin have been evaluated in placebocontrolled, randomised trials enrolling patients with HFrEF.21,22 A study evaluating the efficacy of dapagliflozin in treating HFrEF reported the group randomised to receive dapagliflozin had a significant reduction in the composite primary endpoint of cardiovascular death or worsening heart failure, driven by significant reductions in both heart failure hospitalisation and cardiovascular mortality.21 The Empagliflozin Outcome Trial in Patients with Chronic Heart Failure and a Reduced Ejection Fraction reported that use of empagliflozin was associated with a significant reduction in the composite primary endpoint of cardiovascular death or heart failure hospitalisation, driven by a significant reduction in heart failure hospitalisation and a nonsignificant reduction in cardiovascular mortality.22 A metaanalysis combining these studies reported SGLT2 inhibitor use was associated with significant relative risk reductions in allcause mortality , cardiovascular mortality , first hospitalisation for heart failure and first kidney composite event , with no significant heterogeneity for treatment effect.23
Sglt2 Inhibitors In Hfref
SGLT2 inhibitors carry a class 1 recommendation for reducing HF hospitalization and CV mortality in patients with symptomatic chronic HFrEF, regardless of the presence of T2D.1 Prior data suggested that use of SGLT2 inhibitors offered these benefits in patients without T2D.11 Results of the DEFINE-HF trial found that a greater proportion of patients with symptomatic HFrEF who were treated with dapagliflozin experienced clinically meaningful improvements in HF-related symptoms, functional status, and quality of life than did those given placebo. The observed benefits were consistent, regardless of T2D.
Don’t Miss: What Happens After A Mild Heart Attack
Scope Of The Guideline
The purpose of the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure is to provide an update and to consolidate the 2013 ACCF/AHA Guideline for the Management of Heart Failure for adults and the 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure into a new document. Related ACC/AHA guidelines include recommendations relevant to HF and, in such cases, the HF guideline refers to these documents. For example, the 2019 primary prevention of cardiovascular disease guideline includes recommendations that will be useful in preventing HF, and the 2021 valvular heart disease guideline provides recommendations for mitral valve clipping in mitral regurgitation .
Sglt2 Inhibitors Added To Esc Guidelines For Treatment Of Chronic Hfref
The 5-year update could help solidify the role of sodium glucose co-transporter 2 inhibitors in treating heart failure, years after the first evidence of their effectiveness emerged.
Sodium glucose co-transporter 2 inhibitors empagliflozin and dapagliflozin are now recommended for treatment of chronic heart failure with reduced ejection fraction , according to the latest 5-year update of the European Society of Cardiology Guidelines in acute and chronic heart failure, which were released early Friday during the ESC Congress 2021.
The ESC Congress, being held in a virtual format for the second year due to COVID-19, runs today through Monday.
ESC updates guidelines in various treatment areas on 5-year cycles and releases them throughout its annual Congress. Other updates scheduled this year are valvular heart disease , cardiac pacing , and cardiovascular disease prevention . The heart failure guidelines were simultaneously published in the European Heart Journal.
Chronic heart failure is a condition where the heart is unable to pump blood around the body properly. It usually occurs because the heart has become too weak or stiff. Ejection fraction, which is the percentage of the blood within the ventricles that is ejected during the cardiac cycle, is the most important measure in heart failure.
The rise of SGLT2 inhibitors in heart failure
Changes from 2016
Reference
Recommended Reading: What Factors Affect Heart Rate
Benefits Of The Sodium
There is data about 19 clinical trials that have been initially designed with the aim of elucidating the effect of SGLT2 inhibitors in patients with HFpEF, with and without T2D, on clinical outcomes and the surrogate points , but only eight from these had a completed status along with available results to evaluate . In addition, nine randomised clinical trials have been reported as permanently completed, but the study design provided for the possibility to enrol patients with T2D for whom HF was not determined as inclusion criteria . However, post-hoc analysis was frequently performed with the aim of elucidating the impact of SGLT2 inhibitors on either cardiac biomarkers or HF-related outcomes.
Table 1: Completed randomised clinical trials dedicated the impact of sodium-glucose co-transporter-2 inhibitors on clinical status of patients with heart failure with preserved ejection fraction.BNP: brain natriuretic peptide CV: cardiovascular eGFR: estimated glomerular filtration rate HF: heart failure HFpEF: heart failure with preserved ejection fraction HFrEF: heart failure with reduced ejection fraction KCCQ-TSS: Kansas-City Cardiomyopathy Questionnaire-Total Symptom Score LVEF: left ventricular ejection fraction NT-proBNP: N-terminal proB-type natriuretic peptide NCT: National Clinical Trial T2D: Type 2 diabetes 6MWD: 6-minute walk distance.
Heart Failure With Reduced Lvef
The 2018 NHFA/CSANZ heart failure guidelines strongly recommend an ACE inhibitor , beta blocker and MRA in all patients with HFrEF to decrease mortality and hospitalisation, and an angiotensin receptor neprilysin inhibitor , sinus node inhibitor , diuretic and intravenous iron in selected patients.3,4 In this section, we will review new evidence regarding the use of an ARNI , intravenous iron , SGLT2 inhibitors , a guanylate cyclase stimulator and a selective cardiac myosin activator .
Read Also: Canine Congestive Heart Failure Stages Of Dying
Acc/aha Joint Committee Members
Joshua A. Beckman, MD, MS, FAHA, FACC, Chair
Patrick T. OGara, MD, MACC, FAHA,Immediate Past Chair
Sana M. Al-Khatib, MD, MHS, FACC, FAHA
Anastasia L. Armbruster, PharmD, FACC
Kim K. Birtcher, PharmD, MS, AACC
Joaquin E. Cigarroa, MD, FACC
Lisa de las Fuentes, MD, MS, FAHA
Anita Deswal, MD, MPH, FACC, FAHA
Dave L. Dixon, PharmD, FACC
Lee A. Fleisher, MD, FACC, FAHA
Federico Gentile, MD, FACC
Zachary D. Goldberger, MD, FACC, FAHA
Bulent Gorenek, MD, FACC
Adrian F. Hernandez, MD, MHS
Mark A. Hlatky, MD, FACC, FAHA
José A. Joglar, MD, FACC, FAHA
W. Schuyler Jones, MD, FACC
Joseph E. Marine, MD, FACC
Daniel B. Mark, MD, MPH, FACC, FAHA
Debabrata Mukherjee, MD, FACC, FAHA
Latha P. Palaniappan, MD, MS, FACC, FAHA
Tanveer Rab, MD, FACC
Erica S. Spatz, MD, MS, FACC
Jacqueline E. Tamis-Holland, MD, FAHA, FACC
Duminda N. Wijeysundera, MD, PhD
Y. Joseph Woo, MD, FACC, FAHA
Former Joint Committee member current member during the writing effort.
How To Address Challenges Of Care Coordination
Delivering optimal patient-centered HF care is complex. The range of treatments available, particularly those for patients with HFrEF, include multiple medications, cardiac devices, surgery, and lifestyle adaptations, all of which require education, monitoring, and engagement. For example, patients with HFrEF frequently require consultative care delivered by electrophysiology specialists to implant, monitor, and adjust devices such as implantable cardioverter-defibrillator or cardiac resynchronization therapy devices. As outlined in , the complexity of HF care is further exacerbated by the frequent coexistence of both cardiac and noncardiac comorbidities found in patients with HF. Comorbidities are particularly common in the elderly. More than 50% of patients with HF on Medicare have 4 or more non-CV comorbidities and more than 25% have 6 or more . The care needs for comorbidities can complicateand in some cases preventthe optimal use of HF therapies. Finally, the medical complexity inherent in most patients with HF generally requires the involvement of multiple clinicians across many care settings . This raises the risk of inefficiencies in care delivery, miscommunication, potential drugdrug interactions and drugdisease interactions, and missed opportunities to achieve optimal HF outcomes.
Table 7 Essential Skills for an HF Team
|
Coordination of care for concomitant comorbidities |
HF = heart failure.
| Modality |
|---|
|
Prompts for medication and lifestyle adherence |
Read Also: At What Heart Rate Should I Go To The Hospital
