How Is Congestive Heart Failure Diagnosed
Heart failure is diagnosed with a physical exam and tests that may include:
- Electrocardiogram to measure the electrical activity in the heart
- Brain natriuretic peptide or N-terminal pro-BNP blood tests
- BNP or NT-proBNP level is high in people with heart failure
What Is Stage 3 Of Heart Failure
Stage 3 of Congestive Heart Failure Small bouts of exercise or minimal doses of physical activity will cause the same symptoms mentioned in stage two fatigue, shortness of breath, and heart palpitations. In stage three, lifestyle changes are not as effective, and a surgical procedure may be necessary.
The Four Stages Of Heart Failure
- Reactions 0 reactions
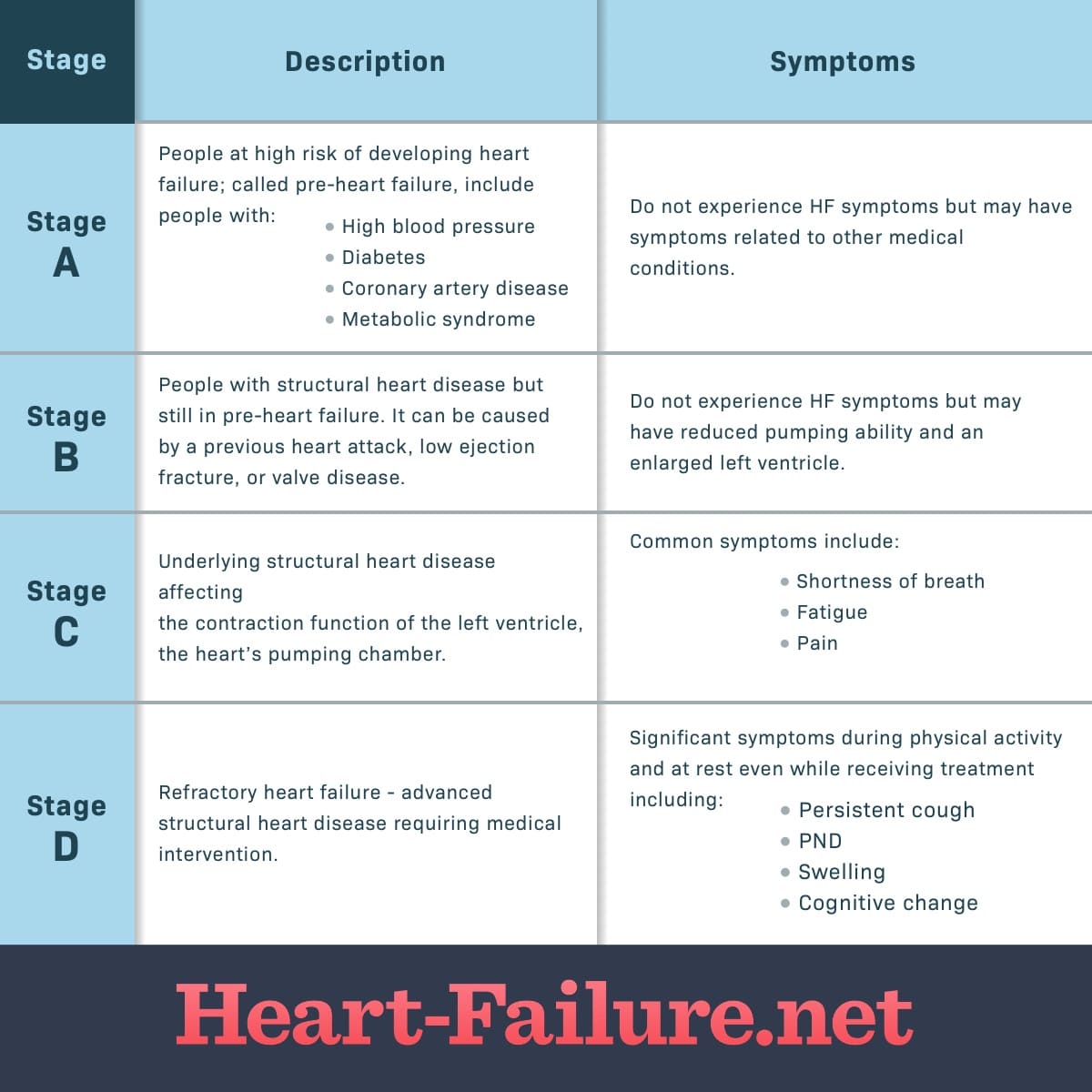
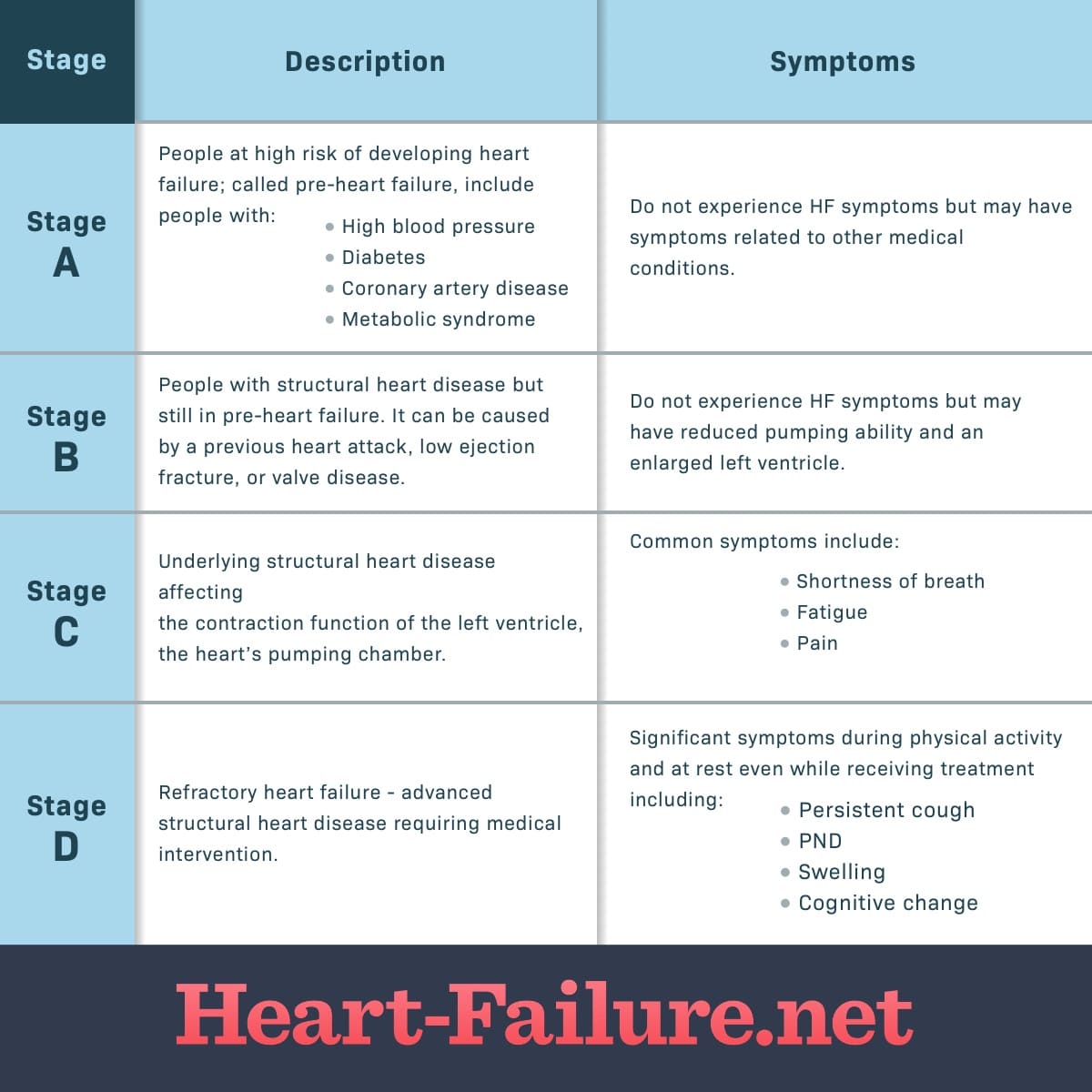
There are four stages of heart failure. The stages range from being at risk of heart failure to having advanced heart failure. These stages were created by the American Heart Association and the American College of Cardiology and were given letter titles A, B, C, and D. Each stage has different recommended treatments depending on a multitude of factors.1
Don’t Miss: Heart Attack Symptoms.women
What Should The Caregiver Remember When The Patient Is At The End
Various important decisions of the patients life have to be taken by the caregivers surrounding the patient. Great responsibilities come up on the caregiver as the patient gradually becomes completely dependent. The caregiver should always be on his toes because there can arise an emergency at any point of time. The patient may have to be admitted to the hospital frequently during the last stage. Symptoms can worsen overnight and the caregivers should be prepared for it.
Also Read:
Stage 4 Congestive Heart Failure
Congestive heart failure is a condition that is characterized by the heart’s inability to pump enough blood and supply it to the various parts of the body. Scroll down to find out more about the symptoms of stage 4 congestive heart failure along with the treatment options for the same.
Congestive heart failure is a condition that is characterized by the hearts inability to pump enough blood and supply it to the various parts of the body. Scroll down to find out more about the symptoms of stage 4 congestive heart failure along with the treatment options for the same.
The human heart is the key organ of the circulatory system of our body. The heart is divided into four chambers. The upper chambers and the lower chambers are referred to as atria and ventricles respectively. The right atrium and the right ventricle pump the deoxygenated blood that is received from the veins into the lungs. The left atrium and the left ventricle receive the oxygenated blood from the lungs.
The oxygenated blood is then carried to various parts of the body by the arteries. The term heart failure refers to the state in which the heart is unable to pump enough blood for fulfilling the bodys requirements. If the pumping action of the heart becomes weak, blood may back into the liver, lungs, abdomen and the lower extremities. Under such circumstances, one is diagnosed with congestive heart failure .
You May Like: How Are Hypertension Heart Disease And Stroke Related
How Is Pulmonary Hypertension Diagnosed
Your provider will perform a physical exam and run tests to reach a pulmonary hypertension diagnosis.
First, youll have a physical exam to check for signs of pulmonary hypertension as well as other heart or lung issues. During this exam, your provider will:
- Ask you questions about your health and your medical history.
- Ask about your symptoms.
- Check the size of the veins in your neck. Bulging neck veins could be a sign of right-sided heart failure.
- Check the size of your liver by feeling the upper right area of your tummy.
- Listen to your heart and lungs with a stethoscope.
- Look at your belly, ankles and legs for edema.
- Measure your blood pressure.
- Measure the oxygen level in your blood using a pulse oximeter.
Pulmonary hypertension can be difficult to diagnose since many signs of PH are similar to those of other conditions. So, after your physical exam, your provider may run some tests to get more information.
Your provider may also refer you to a pulmonologist or cardiologist.
Stage 4 Heart Failure Life Expectancy: Stage D Heart Failure Life Expectancy
Heart failure disease is a very risky term these days. Stage 4 heart failure life expectancy is out of hand because this stage, stage 4 or stage D, is the final stage of heart failure. People from young to adults suffer from this problem. It is one of the most complex diseases.
The number of these patients is increasing day by day. Heart failure can occur due to various reasons, including unhealthy living and changes in food habits.
Jump to…
Don’t Miss: Does Heart Attacks Run In Families
What Is Nyha Class 4 Heart Failure
Class IV: Inability to carry on any physical activity without discomfort but also symptoms of heart failure at rest, with increased discomfort if any physical activity is undertaken.
Is Stage 4 heart failure serious?
Stage four of congestive heart failure produces severe symptoms such as rapid breathing, chest pain, skin that appears blue, or fainting. These symptoms may occur whether you are exercising or at rest. In this stage, your doctor will discuss if surgery is beneficial.
How long can you live with stage 4 heart failure?
3. Most people with end-stage heart failure have a life expectancy of less than 1 year. 4. The leading causes of heart failure are diseases that damage the heart, such as heart disease, high blood pressure, and diabetes.
Is Stage 3 heart failure reversible?
CHF is not curable, but early detection and treatment may help improve a persons life expectancy. Following a treatment plan that includes lifestyle changes may help improve their quality of life.
Is Stage 3 heart failure considered advanced?
Patients with end stage heart failure fall into stage D of the ABCD classification of the American College of Cardiology /American Heart Association , and class IIIIV of the New York Heart Association functional classification they are characterised by advanced structural heart disease and pronounced
What Are The First Symptoms Of Pulmonary Hypertension
The first symptom of pulmonary hypertension is shortness of breath during your daily activities. These may include climbing stairs or grocery shopping. You may also feel short of breath when you exercise.
At the start of pulmonary hypertension, you may not have any symptoms. When you do start to notice symptoms, they may be mild. But PH symptoms get worse over time, making it harder for you to do your usual activities.
Don’t Miss: Can Anesthesia Cause Heart Attack
History And Physical Exam
A clinician listens to your heart and lungs and measures your blood pressure and weight. They will also ask about your:
- Familys medical history, especially previous cardiac problems
- Medications, including prescriptions, over-the-counter drugs and supplements
- Personal medical history
Blood tests can measure several things related to heart failure:
- Sodium and potassium levels
- Creatinine, which helps measure how well your kidneys are working
- B-type natriuretic peptide , a hormone released from the ventricles in response to increased wall tension that occurs with heart failure
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
You May Like: When Is Heart Rate Too Low
Heart Failure Survival Rates
The survival rates from heart failure have been improving over the years. The improvement is slow, but gradual. Clinicians measure overall patient survival from a disease by comparing large groups of people with the disease to large groups of the same age range without it. For example, a 1-year survival rate of 90% is good. It means people with the disease are 90% as likely as people without the disease to be alive for at least one year after diagnosis. For heart failure, the 1-year survival rate rose from 74% in 2000 to about 81% in 2016. The 5-year survival rate increased from 41% to 48%, and the 10-year survival rate rose from about 20% to 26%.
Keep in mind prognosis and life expectancy information is based on data registries from several years ago . Someone diagnosed with heart failure today may have a better prognosis because heart failure treatment, including , improves with time.
If you or a loved one has heart failure and you would like to know more about your case, ask your doctor how your age, overall health, and treatment affect your prognosis and life expectancy. Knowing what to expect can help you make plans for the time you have.
Stage C Treatment Options
Treatment at this stage focuses on managing your symptoms, optimizing your heart function, and preventing worsening of your condition.
Medications to treat stage C heart failure include:
- Diuretics to reduce fluid retention
- Beta blockers to help make your heart work less hard
- SGLT2 inhibitors to reduce the risk of cardiovascular death and hospitalization for heart failure
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Entresto , which reduces the risk of death and hospitalization among patients with chronic heart failure
- Aldosterone antagonists
- Digoxin to help the heart beat stronger and more regularly
- Possible cardiac resynchronization therapy
- Possible implantable cardiac defibrillator therapy
In addition to the lifestyle changes for stages A and B, you may need to make the following changes:
- Reduce your sodium intake
- Restrict fluid intake
- Keep track of your weight daily
Remember that even if the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression of your condition to stage D.
Also Check: How To Slow Your Heart Rate
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
Your doctor may recommend:
When Should We Consider Hospice Care For Chf
Hospice can be appropriate for many types of end-stage heart disease, including heart failure, valvular heart disease and coronary artery disease. Regardless of the type of heart disease, hospice is a fitting choice when an individual begins to experience persistent, severe symptoms that interfere with their daily life. Hospice care should also be considered if an individual begins to have recurrent hospitalizations or complicated hospitalizations, such as an ICU stay.
One of the earliest symptoms of a declining heart is exercise intolerance. This begins with symptoms present with significant exertion and can progress to symptoms present with doing our activities of daily living, such as bathing and dressing. At its worst, symptoms are present at rest. Heart disease, depending on the etiology, can present with other more specific symptoms, including fluid overload, chest pain, lightheadedness, shortness of breath and arrythmias. Patients may experience unintentional weight loss despite a normal appetite. As the disease progresses, cardiac output can decline, resulting in low blood pressure and poor prefusion of our vital organs. This can lead to dysfunction of further organ symptoms, such as worsening kidney function.
Also Check: Which One Of The Following Instructions For Monitoring Your Exercise Heart Rate Is Correct
Interactive Multiple Choice Questions
This Education in Heart article has an accompanying series of six EBAC accredited multiple choice questions .
To access the questions, click on BMJ Learning: Take this module on BMJ Learning from the content box at the top right and bottom left of the online article. For more information please go to: Please note: The MCQs are hosted on BMJ Learningthe best available learning website for medical professionals from the BMJ Group.
If prompted, subscribers must sign into Heart with their journals username and password. All users must also complete a onetime registration on BMJ Learning and subsequently log in on every visit.
Acute Or Chronic Heart Failure
Heart failure can be acute or chronic.
Acute heart failure happens when either:
- symptoms come on suddenly
- it’s the first time the patient has had heart failure
- symptoms suddenly become worse during chronic heart failure.
Chronic heart failure is when someone’s heart failure develops gradually over time and is a long-term condition.
Don’t Miss: Signs And Symptoms Of Right Sided Heart Failure
Stage 3 Of Congestive Heart Failure
Its not uncommon for congestive heart failure to be accompanied by other heart conditions. If you are diagnosed with stage three CHF, along with another heart condition, its likely that youll have difficulty performing regular tasks. Small bouts of exercise or minimal doses of physical activity will cause the same symptoms mentioned in stage two fatigue, shortness of breath, and heart palpitations. In stage three, lifestyle changes are not as effective, and a surgical procedure may be necessary. However, its never too late to talk to a doctor about your heart condition and what the future may look like.
What Are The Advantages And Disadvantages Of This Procedure
The biggest advantage of heart transplantation is that its a life-saving option when other options didnt work, were too risky to use, or were unlikely to help.
The biggest disadvantages of heart transplant are:
- More people need a heart transplant than there are available donor hearts.
- Its an extremely complicated surgery, limiting it to only the most well-equipped and best-staffed hospitals.
- Some people may be too ill to survive the procedure.
- The procedure has several potential risks and complications .
What are the risks or complications of this procedure?
The most common risks and complications of heart transplant include the following:
- Organ rejection.
Written bySmall Doors medical experts
Congestive heart failure is fairly common in dogs. Approximately 10% of all dogs, and 75% of senior dogs, have some form of heart disease. CHF itself is not a disease: it is a condition that is a result of heart disease.
In This Article
You May Like: How Do Veins Return Blood To The Heart
What Happens Before This Procedure
Because there are far more people who need hearts than donors, theres a strict selection process that you have to undergo to receive a heart transplant. The goal of this process is to select recipients who have the best chance of long-term survival based on their overall health.
After a healthcare provider refers you to a transplant program, youll undergo the following.
Medical evaluation
To ensure that donor hearts go to people with the best chance of survival, healthcare providers will evaluate your overall health by running several different tests. Some, but not all, of the possible tests are listed below.
Lab tests will include tests on your blood, urine and other screenings. These tests will look for the following:
- Blood composition. This analyzes your bloods levels of red blood cells, platelets, and more. These tests will also analyze your blood chemistry, looking for signs of other conditions that might affect your ability to undergo a heart transplant.
- Immune system analysis. These tests help providers anticipate how well your immune system can tolerate a donor organ.
- Kidney function. These tests analyze your urine to see how well your kidneys are working.
- Tests for alcohol, tobacco and drugs. These are often important tests if you have a history of using recreational drugs or drinking too much alcohol. Most transplant centers require that youre sober and avoid using tobacco products and recreational drugs for an extended time before your transplant.
