Types Of Cardiomyopathy & Heart Failure
NYU Langone heart specialists are familiar with all types of cardiomyopathy, which means sickness of the heart muscle. This condition changes the shape and function of the heart. It reduces the hearts ability to pump blood and can cause heart arrhythmias, in which the heart beats too slowly or quickly.
Schedule an Appointment
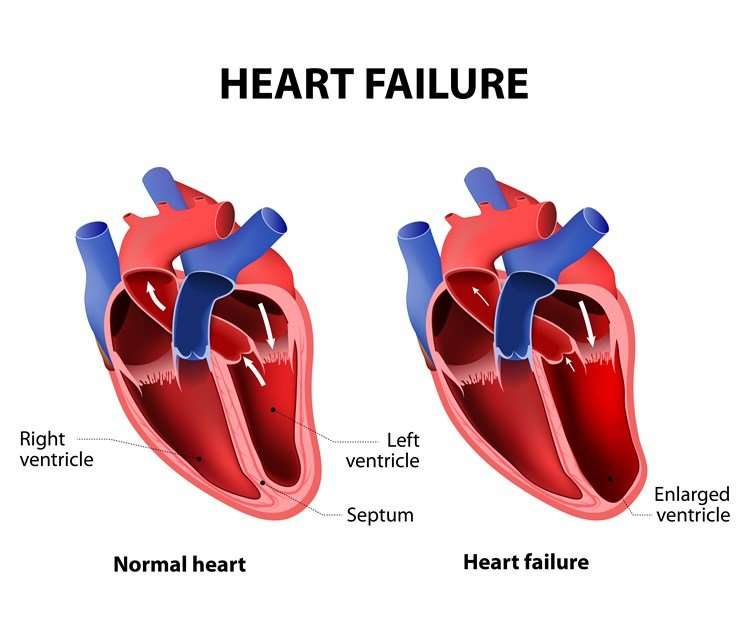
Heart failure occurs when conditions such as cardiomyopathy, heart valve disease, or congenital heart disease damage the heart, reducing its ability to pump blood to the body.
Despite its name, heart failure isnt a complete loss of heart function, as occurs in sudden cardiac arrest, when the heart suddenly stops beating. Heart failure means the organ isnt pumping blood to the rest of the body as well as it should. This is a serious and progressive conditionyet manageable.
Doctors use a test called an echocardiogram to determine the percentage of blood the heart pumps with each contraction. This is called ejection fraction. A normal hearts ejection fraction is typically between 55 percent and 70 percent. The ejection fraction number is used to describe different types of heart failure or cardiomyopathy.
Coronary Artery Disease Linked To Both Conditions
Heart disease and heart attack both share coronary artery disease as a primary cause. This occurs over time when your arteries narrow and harden due to deposits of plaque from fat and other types of substances found in food. This is one reason why a healthy diet low in fat and cholesterol is so important.
What Is Heart Failure
Heart Failure, commonly known as congestive heart failure mainly arises due to improper blood pumping. In this condition, the body fluids are stored in the lungs and hence cause a problem in breathing.
In some critical cardiac diseases such as persistently high blood pressure and coronary artery disease, the cardiac muscles become stiffer and weaker.
Due to this cardiac muscles are unable to fill systolic and diastolic blood in the heart. Heart failure may be categorized as chronic and acute.
The common symptoms of heart failure are shortness of breath, weakness, swelling. Heart failure can be categorized into mainly three types Left-sided heart failure, Right-sided heart failure, and Systolic heart failure.
In Left-sided heart failure, body fluid accumulates in the lungs, which causes breath shortness. In Right-sided heart failure, body fluid deposits in the abdominal cavity and feet hence causing swelling.
In Systolic heart failure, the heartâs left ventricle can not contract actively and efficiently, which indicates a pumping problem.
Heart failure may lead to many other fatal diseases such as liver damage, kidney failure, and heartbeat fluctuation.
Patients can improve their conditions by maintaining a better lifestyle. Patients should eat healthy food and a balanced diet along with no smoking motive.
You May Like: Life Expectancy Heart Failure
Endoplasmic Reticulum Stress And Impaired Calcium Handling
The endoplasmic reticulum has a major role in Ca2+ handling, lipid synthesis, and protein folding and modification . Moreover, cytosolic Ca2+ levels are involved in the regulation of cellular metabolism, cell signaling, and muscle contraction. Hyperglycemia and IR trigger endoplasmic reticulum stress leading to the accumulation of unfolded proteins and impairment of Ca2+ handling. In diabetic cardiomyopathy, impairment of Ca2+ reuptake by endoplasmic reticulum results in prolongation of diastolic relaxation time . Studies on animal models have indicated that impaired cardiomyocyte Ca2+ handling plays a key role in diabetes-induced diastolic dysfunction .
Why Choose The Upmc Hypertrophic Cardiomyopathy Center For Care
At UPMC’s Hypertrophic Cardiomyopathy Center, people with HCM have access to:
- Coordinated, state-of-the-art care for the diagnosis and treatment of this complex heart disease.
- Innovative treatment options based on the latest research protocols for HCM.
- A team of experts in HCM disease management, advanced cardiac imaging, and cardiovascular genetics.
Also Check: What Kind Of Heart Surgery Did Paxton Have
What To Expect At The Heart & Vascular Center
The Heart & Vascular Center is located in the Shapiro Cardiovascular Center, across the street from our main 75 Francis Street entrance. The center brings together the full range of services in one location, fostering seamless and coordinated care for all cardiovascular patients.
If you are having surgery or a procedure, you will likely be scheduled for a visit to the Watkins Clinic for pre-operative information and tests.
The day of surgery, your care will be provided by surgeons, anesthesiologists and nurses who specialize in surgery for patients with CHD. After surgery, you will go to the post-surgical care unit where you will receive comprehensive care by an experienced surgical and nursing staff.
During your surgery, family and friends can wait in the Shapiro Family Center. Staff members will provide surgery updates and caregivers who leave the hospital will be contacted by cell phone.
Brain Differences Suggest Therapeutic Targets In Takotsubo
A new study has identified differences in the brain present in patients with the cardiac disorder Takotsubo syndrome vs control scans, which may lead to new therapeutic targets.
Takotsubo syndrome is an acute heart failure cardiomyopathy mimicking an acute myocardial infarction in its presentation, but on investigation, no obstructive coronary disease is present. The syndrome, which mainly affects women, typically occurs in the aftermath of intense emotional or physical stress and has become known as “Broken Heart syndrome.”
The mechanism by which emotional processing in the context of stress leads to significant cardiac injury and acute left ventricular dysfunction is not understood. So, the current study examined both structural and functional effects in the brain in patients with Takotsubo syndrome to shed more light on the issue.
“The abnormalities in the thalamus-amygdala-insula and basal ganglia support the concept of involvement of higher-level function centers in Takotsubo syndrome, and interventions aimed at modulating these may be of benefit,” the authors conclude.
The study was January 11 in JACC Heart Failure.
Lead author Hilal Khan, MB BCh, BAO, from the University of Aberdeen, United Kingdom, explained to theheart.org | Medscape Cardiology that patients with Takotsubo syndrome have a substantial drop in heart function and show an apical ballooning of the heart.
JACC Heart Failure. Published online January 11, 2023. Full text
Send news tips to .
Read Also: How To Find Your Max Heart Rate
What Tests Might I Have To Diagnose Cardiomyopathy
If your healthcare provider suspects you have a heart condition, you will see a cardiologist . A cardiologist performs a full assessment that may include a range of diagnostic tests. You may have:
- Ambulatory monitoring uses devices that track your heart rhythm.
- Cardiac CT uses X-rays to make a video of your blood vessels and heart.
- Cardiac MRI uses radio waves and magnets to create images of your heart.
- Echocardiogram uses sound waves to create an image of your blood flow and heartbeat.
- Electrocardiogram records your hearts electrical activity.
- Exercise stress test raises your heart rate in a controlled way to see how your heart responds.
- Cardiac catheterization uses a catheter to measure your hearts blood flow and pressure.
- Myocardial biopsy studies a small sample of your heart muscle tissue to look for cell changes.
Heart Failure Management Programs
Attending a specialised program for people with heart failure can reduce the risk of complications and having to go to hospital. Going to a program can also help you live longer and improve your quality of life.
Heart failure programs, sometimes called chronic disease management programs, are run by health professionals who work as a team to help you manage your condition. The team can include a heart failure nurse, a cardiologist, pharmacist, physiotherapist, dietitian or a psychologist.
When you attend a heart failure management program, youll get information to help you manage your condition. This can include:
- how to manage your heart failure medicines
- when to act if your symptoms get worse
- how to monitor your fluid levels and salt intake
If you have heart failure and havent been referred to a heart failure management program, ask your doctor to help you enrol. Some services are now available from your own home using telephone and internet services.
Don’t Miss: Congestive Heart Failure Legs
The Relationship Between Diabetes And Comorbidities
Traditional modifiable CVD risk factors, such as hypertension, obesity, dyslipidemia, and cigarette smoking are prevalent among individuals with diabetes. Hypertension affects 66% to 76% of adults with diabetes in the US . According to the 2020 National Diabetes Statistics Report, 45.8% of adults with diabetes are obese and 15.5% are morbidly obese .
Coexisting CVD risk factors significantly contribute to the risk of HF in patients with diabetes. A large prospective cohort study, including > 270,000 participants with T2DM in the Swedish National Diabetes Register, examined the relationship between five risk factors and CVD outcomes after a median follow-up of 5.7 years , The analyses revealed that participants with T2DM who had no risk-factor variables outside the target ranges had a 45% higher risk of hospitalization for HF when compared to that of a control group without diabetes. However, the excess risk of hospitalization for HF was substantially higher when patients with T2DM had all five risk-factor variables outside the target range. These findings indicated the importance of the control of coexisting CV risk factors for the prevention of HF in diabetes.
What Is Cardiomyopathy In Adults
Cardiomyopathy is a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body. The various types of the disease have many causes, signs and symptoms as well as treatments. In most cases, cardiomyopathy causes the heart muscle to become enlarged, thick or rigid. In rare instances, diseased heart muscle tissue is replaced with scar tissue.
As cardiomyopathy worsens, the heart becomes weaker. The heart becomes less able to pump blood throughout the body and incapable of maintaining a normal electrical rhythm. The result can be heart failure or irregular heartbeats called arrhythmias. A weakened heart also can cause other complications, such as heart valve problems.
Read Also: Why Anxiety Feels Like Heart Attack
Epidemiology Of Diabetes And Hf
There is a bidirectional link between diabetes and HF . Diabetes, either type 1 or type 2, is a strong risk factor for the development of HF . In addition, HF may contribute to the pathogenesis of IR and T2DM . The shared underlying risk factors and the overlap of the pathophysiological mechanisms play a critical role in the frequent coexistence of T2DM and HF.
Based on the data from the National Health and Nutrition Examination Survey 2013 to 2016, the prevalence of HF is 2.2% in the US general adult population . The prevalence of HF in individuals with diabetes ranges between 9% and 22% depending on the characteristics of the population studied . Diabetes is also highly prevalent among patients with HF. In major contemporary drug trials of HF, 32% to 43% of patients with chronic HF had concomitant diabetes . A report from a nationwide US registry showed that the prevalence of diabetes was 44% among individuals hospitalized with HF and had increased over the past decade . In this registry, individuals with diabetes had more extended hospital stays compared to those without diabetes. Similarly, the prevalence of diabetes was reported as 45.6% among individuals with HF in Olmstead County, MN .
Can Surgery Be Used To Treat Heart Failure
In heart failure, surgery may sometimes prevent further damage to the heart and improve the heart’s function. Procedures used include:
- Coronary artery bypass grafting surgery. The most common surgery for heart failure caused by coronary artery disease is . Although surgery is more risky for people with heart failure, new strategies before, during, and after surgery have reduced the risks and improved outcomes.
- Heart valve surgery. Diseased heart valves can be treated both surgically and non-surgically .
- Implantable left ventricular assist device . The LVAD is known as the “bridge to transplantation” for patients who haven’t responded to other treatments and are hospitalized with severe systolic heart failure. This device helps your heart pump blood throughout your body. It allows you to be mobile, sometimes returning home to await a heart transplant. It may also be used as destination therapy for long-term support in patients who are not eligible for transplant.
- Heart transplant. A heart transplant is considered when heart failure is so severe that it doesn’t respond to all other therapies, but the person’s health is otherwise good.
Don’t Miss: Chronic Congestive Heart Failure
Impact Of Glycemic Control
In patients with T1DM and T2DM, intensive glycemic control significantly reduces the risk and severity of microvascular complications . However, despite the strong epidemiologic link between poor glycemic control and HF risk, the effects of intensified glycemic control in the prevention of development of HF remain controversial. Major clinical trials that established the CV benefits and risks of intensive glycemic control did not include HF as a primary endpoint. However, post hoc or secondary outcome analyses of prospective trials have shed light on the relationship between glycemic control and HF prevention.
The impact of specific antidiabetic agents on the prevention of HF in high-risk patients is discussed in the treatment section below.
What Are Its Symptoms
In its initial stages, ischemic cardiomyopathy usually doesnt show any outward symptoms. However, as the disease progresses, people with this disease can experience the following symptoms:
- Chest pain, which can happen after eating large meals, or after vigorous exercise
- Heart palpitations or a sensation that your heart is skipping or pounding
- Shortness of breath
- Irregular heartbeat
- Swelling in the feet or ankles
Its also possible for patients with this type of cardiomyopathy to experience just some of the symptoms above. The symptoms typically vary from person to person, and depend on their current state of health as well as any preexisting conditions that they might have.
Read Also: Heart Attack And Arm Pain
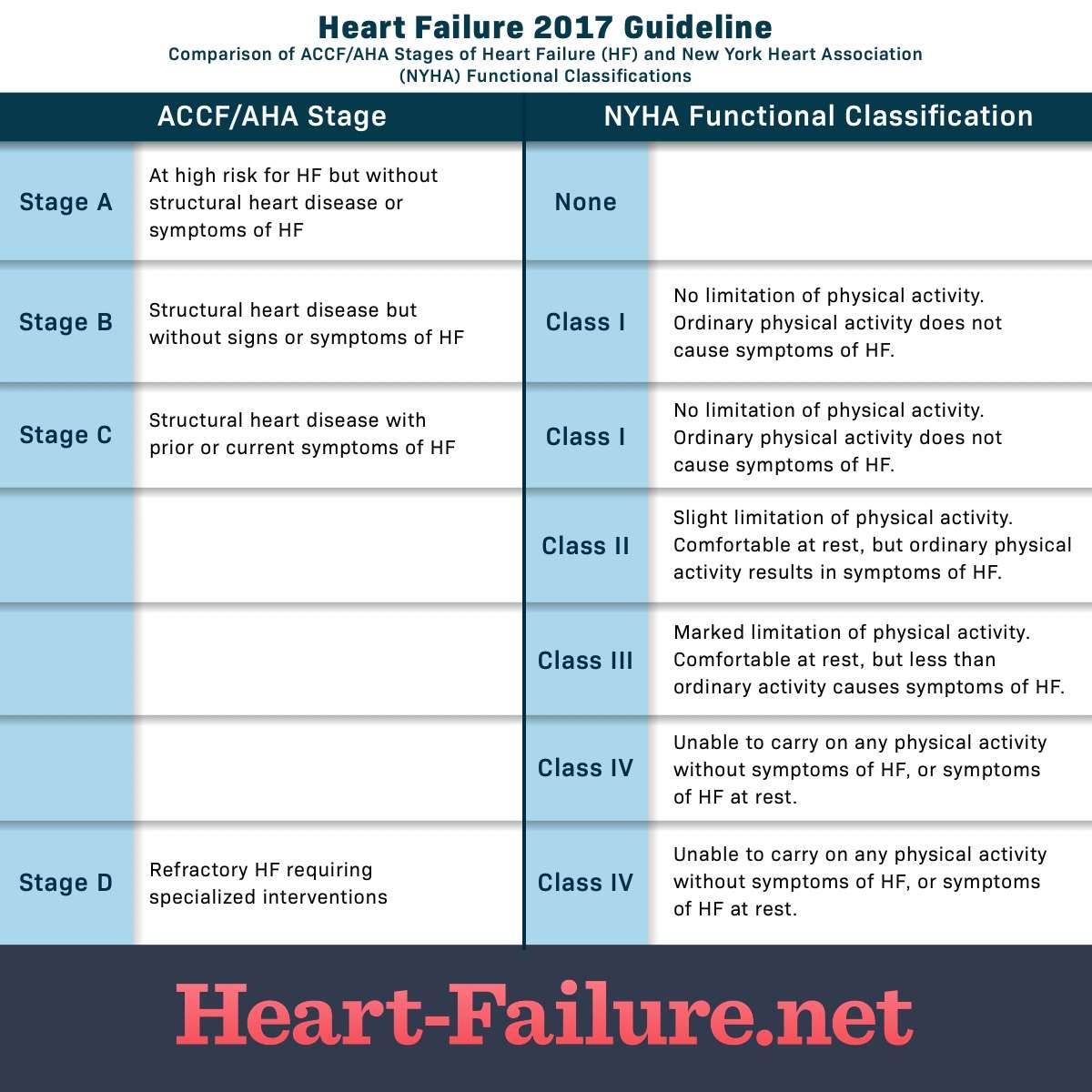
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the “Stages of Heart Failure.” These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
Surgical Options For Cardiomyopathy
If the obstruction of outflow of blood from the left ventricle to the body is extremely severe, the thickened heart muscle can be trimmed using one of two surgical techniques:
- Surgical myectomy open-heart surgery performed to cut away the portion of the muscle that is thickened, relieving the obstruction to blood flow.
- Alcohol septal ablation a heart catheterization procedure used to introduce a catheter into one of the small arteries that brings blood to the abnormally thickened septum alcohol is injected into the artery to reduce the size of the muscle.
Don’t Miss: Why Does Heart Rate Increase During Exercise
Are Cardiomyopathy And Congestive Heart Failure The Same Thing
Cardiomyopathy and Congestive Heart Failure are extremely common conditions that are responsible for millions of death around the globe. Cardiomyopathy belongs to the heterogeneous group of diseases that cause either mechanical or electrical dysfunction. The occurrence is due to several factors. They are part of multi-system disorder or confined to the heart alone that leads to cardiovascular death. Congestive heart failure, on the contrary, is the inability of the heart to pump the required quantity of the blood to meet the demands of the body.
How Is Cardiomyopathy Treated
Cardiomyopathy treatment focuses on managing your symptoms. Treatment also slows the diseases progression. You will have regular checkups to keep an eye on your hearts health.
Your healthcare provider may recommend:
- Medications: Heart medications can improve your blood flow, manage symptoms or treat underlying conditions. You may take blood thinners such as warfarin , beta blockers such as propranolol or medications to lower cholesterol.
- Devices to correct arrhythmias:Pacemakers or implantable cardioverter defibrillators treat irregular heart rhythms. These devices monitor your heartbeat. They send electrical impulses to your heart when an arrhythmia starts.
- Devices to improve blood flow: Some devices help your heart pump blood more efficiently. Cardiac resynchronization therapy devices control the contractions between the left and right sides of the heart. A left ventricular assist device helps your heart pump blood.
- Surgery: If you have severe symptoms or underlying heart conditions, your provider may recommend heart surgery. Providers usually only recommend open-heart surgery or a heart transplant when all other treatments have failed to bring relief.
Also Check: Does Heart Failure Go Away
Pharmacological Treatment Of Hfref
Neurohumoral antagonists , with their proven morbidity and mortality benefits, have been the cornerstone of the guideline-directed medical therapy for patients with chronic HFrEF . The guidelines generally do not recommend specific therapeutic approaches in patients with diabetes compared to those without diabetes.
RAAS AND NEPRILYSIN INHIBITORS
AHA/ACC and ESC guidelines recommend the use of an ACE inhibitor therapy for patients with HFrEF. ARBs are considered as acceptable vasodilator treatment options as a first-line alternative to ACE inhibitors or for patients intolerant of ACE inhibitors because of cough or angioedema. The guidelines also recommend the use of an angiotensin receptor-neprilysin inhibitor as a replacement for an ACE inhibitor or an ARB in patients with chronic symptomatic HFrEF who have been stable on a prior regimen of ACE inhibitor or ARB. This recommendation was based on the landmark PARADIGM-HF trial which proved that ARNI therapy was superior to ACE inhibition alone in reducing the HF hospitalization and mortality risk among patients with HFrEF. The more recent PIONEER-HF trial) trial published in 2019 confirmed that the initiation of sacubitril-valsartan is also effective and safe among HFrEF patients who are hospitalized for acute decompensated HF .
BETA-BLOCKERS
MINERALCORTICOID RECEPTOR INHIBITORS
IVABRADINE
