Diuretic Pseudoresistance And Resistance
Diuretic therapy with a relatively high dose of a loop diuretic, eg 160mg furosemide daily, may fail to produce the desired reduction in excess bodily fluid in patients without important renal function impairment. Most frequently this is due to low compliance with treatment, to excess sodium intake, or to the effect of co-medications that cause renal retention of sodium. The latter include agents for heart failure, such as vasodilators, or for other conditions . In other instances, the prevailing mechanism conducing to failure of loop diuretic therapy to control excess bodily fluid is significant true resistance of the nephron to the action of loop diuretics.
Diuretics In Patients With Acute Decompensated Heart Failure
Most hospitalizations for acute decompensated heart failure are related to congestion, and thus diuretic therapy remains the primary treatment, administered to > 90% of patients hospitalized with heart failure. Intravenous loop diuretic therapy has a quicker mechanism of action and eliminates uncertainty about gastrointestinal absorption and is therefore the preferred method of treatment in ADHF. Administration of intravenous furosemide to patients with ADHF typically results in a prompt diuretic effect that peaks at 1.5hours. This effect leads to a decrease in ventricular filling pressures and improvement in symptoms in the majority of patients with ADHF. Intravenous loop diuretics should generally be continued until euvolemia is achieved, at which time patients can be transitioned back to oral diuretic regimens. Monitoring of patients for 24hours on oral diuretic therapy to ensure that volume retention does not recur may prevent short-term rehospitalizations.
Who Cannot Take Potassium
There are very few people who are not able to take these medicines. They should not be taken by anyone who has high levels of potassium in their blood, severe kidney problems, or Addison’s disease.
In addition, potassium supplements should not be taken with these medicines. Some salt substitutes that you can buy are high in potassium. These should be avoided if you take a potassium-sparing diuretic.
Taking a potassium-sparing diuretic at the same time as an angiotensin-converting enzyme inhibitor or an angiotensin receptor antagonist medicine can also cause very high blood potassium levels.
How to use the Yellow Card Scheme
If you think you have had a side-effect to one of your medicines you can report this on the Yellow Card Scheme. You can do this online at www.mhra.gov.uk/yellowcard.
The Yellow Card Scheme is used to make pharmacists, doctors and nurses aware of any new side-effects that medicines or any other healthcare products may have caused. If you wish to report a side-effect, you will need to provide basic information about:
- The side-effect.
Don’t Miss: Why Do Av Nodal Cells Not Determine The Heart Rate
The Clinical And Functional Effects Of Diuretics
Effective diuretic therapy provides impressive symptomatic relief in patients with CHF.25 Haemodynamically, forced diuresis results in a decrease in pulmonary circulation wedge pressure, and stroke volume and cardiac output decrease initially. Upon prolonged administration, the cardiac index may stay below, equal or surpass its pre-treatment value, but the magnitude of these changes is generally low., There is a lack of correlation between variables indicating effort capacity and cardiac output in patients suffering from chronic CHF, but we have found that the NYHA functional class correlates positively and that the 6-min mean walking velocity correlates negatively with clinical and radiological increasing ordinal indicators of the magnitude of lung congestion and pulmonary water and with the cardiothoracic ratio. These findings strongly suggest that the beneficial effects of diuretics on the main symptoms of CHF are mainly due to the decrease in thoracic fluid that results from their diuretic action. Thus, lung congestion and water and cardiac size should be considered operational objectives of diuretic therapy in CHF.
Figure 1
Diuretics provide the prime relief of the symptoms that limit physical activity. In practice, patients with CHF should be treated with diuretics and with other drugs. Certain co-therapies may amplify the beneficial effects of diuretics.
Diuretics In Chronic Heart Failure
| Initial Dose |
|---|
| 1:1 |
- Abbreviations: IV, intravenous PO, by mouth.
Thiazides and metolazone are most frequently used to overcome resistance to escalating doses of loop diuretics alone. Metolazone is most often used for this indication, typically given as a single oral dose 1hour prior to loop diuretics. Although this strategy can often be effective in overcoming diuretic resistance, careful monitoring of fluid status and serum electrolytes such as sodium, potassium, and magnesium is critical, since the combination of metolazone and loop diuretics can induce severe volume depletion or electrolyte disturbances. In general, the chronic use of daily adjunctive metolazone should be discouraged.
Also Check: Ibs And Palpitations
Spironolactone In Left Ventricular Chf
Left ventricular CHF is a problem commonly seen in family practice, with a prevalence close to 2 percent. In a typical panel of 2,500 patients, about 50 will have heart failure. In mild failure, the annual mortality is 5 to 10 percent annually in severe cases, it increases to 30 to 40 percent annually.5
The Cooperative North Scandinavian Enalapril Survival Study 6 trial in 1987 was the first to show that ACE inhibitors could decrease mortality related to heart failure. ACE inhibitors are generally well tolerated except in patients with an elevated creatinine level . The angiotensin-II receptor antagonist losartan has also been shown to decrease mortality in patients with heart failure.7
Loop diuretics have been universally used to reduce the symptoms of heart failure, but they have not been shown to reduce mortality.8 Digoxin has recently had a resurgence of use in patients with severe CHF it does not reduce mortality but has been shown to reduce symptoms and hospitalizations.9
In stark contrast to previous conventional wisdom, beta blockers have been shown to reduce mortality in patients with heart failure who can tolerate them. In the Cardiac Insufficiency Bisoprolol Study ,10 patients taking bisoprolol, a beta1 selective blocker, had fewer hospital admissions and cardiovascular deaths than the control group. All patients had NYHA class III or IV failure, were taking ACE inhibitors and diuretics, and had been clinically stable for at least six weeks.
New Use Of Spironolactone In Congestive Heart Failure
The anti-aldosterone substance spironolactone is currently classified as a facultative diuretic and antikaliuretic,, since it increases natriuresis and decreases kaliuresis only when plasma aldosterone concentration is high, as occurs when sodium intake is low or when loop or thiazide-type diuretics are used at diuretic doses. Spironolactone has been classically used in patients with CHF treated with loop or with early distal tubular diuretics mainly to prevent or to co-treat hypokalaemia. Recently, it was found that the addition of a relatively small dose of spironolactone to the classic treatment of CHF with a loop or a thiazide-type diuretic, digitalis and an angiotensin-converting enzyme inhibitor prolongs life and reduces hospitalisation frequency in patients with advanced cardiac failure and systolic dysfunction. It is not known whether this salutary action of spironolactone is due to a decrease in the rate at which cardiac interstitial fibrosis progresses,, to an improvement in bodily potassium turnover, to added natriuresis, or to a combination of factors. The addition of a low amount of spironolactone to antihypertensive treatment with conventional doses of diuretics may result in a supplementary fall in high BP.
You May Like: Can Ibs Cause Palpitations
Diuretics In The Treatment Of Heart Failure
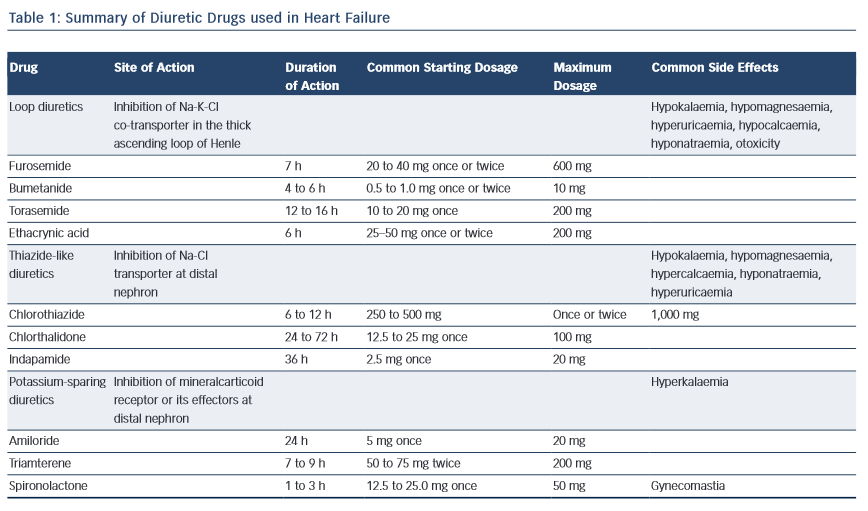
Pharmacologic TreatmentsManagement of HF commences with a careful assessment of etiology and severity of the disease followed by correction of systemic factors , lifestyle modifications , and a review of drugs that may contribute to HF .10Reducing pulmonary and/or systemic congestion along with edema and other clinical symptoms such as dyspnea and shortness of breath is the primary goal of diuretic therapy. Diuretic agents promote an increase in urine output by altering how the kidney handles sodium and water, since sodium excretion is followed by water excretion. Nonetheless, inhibition of sodium reabsorption may take place at different segments of the renal tubular system. A synergistic effect may be seen when using two different diuretic agents that alter sodium reabsorption at multiple nephron sites, therefore enhancing efficacy.Properties of the pharmacologic diuretic agents mainly utilized in treating HF are described in TABLE 2.
Renal Handling Of Sodium And Water
To understand the action of diuretics, it is first necessary to review how the kidney filters fluid and forms urine. The following discussion and accompanying illustration provide a simple overview of how the kidney handles water and electrolytes. For more detailed explanation, particularly related to ion and fluid movement across the renal tubular cells, the reader should consult a physiology textbook.
Also Check: Reflux And Palpitations
Why Are Diuretics Used In Heart Failure
Diuretics are an integral part of heart failure treatment, along with other medications to treat the underlying cause of heart failure. Diuretics help the kidneys flush out the excess fluid and maintain normal blood volume.
The elimination of excess fluid reduces pressure in the veins and the overload of venous blood into the heart. As a result, the heart requires less effort to pump out blood, and the blood pressure in the arteries drops. The fluid accumulated in the lungs and other tissues drains back into the circulation, providing symptom relief.
Drug Interactions And Toxicity:
Drug interactions and adverse effects/toxicities are typically those described for diuretics as a class. However, some special considerations for furosemide bear mentioning. Furosemide has the potential for ototoxicity. When administered as the sole agent, furosemide in dosages > 20 mg/kg, IV, can result in loss of hearing in dogs. Dosages of 50â100 mg/kg result in profound loss of hearing. Furosemide can also potentiate the ototoxic and nephrotoxic effects of other drugs such as the aminoglycosides.
Don’t Miss: 10 Second Trick To Prevent Heart Attack
Diuretics To Treat Heart Failure
There are different classes of diuretics and each works in a distinct way in the kidneys to remove fluid buildup from the body which reduces pressure on blood vessel walls.2-3 As the kidneys eliminate the excess water from the blood, the total blood volume that the heart has to pump is reduced, which causes blood pressure to go down and makes it easier for the heart to pump forward.4
The different kinds of diuretics include carbonic anhydrase inhibitors, loop diuretics, potassium-sparing diuretics, and thiazide diuretics.3
Loop diuretics are the preferred diuretic for use in patients with heart failure. They are also used to treat hypertension and edema due to chronic kidney disease.4 They cause the kidneys to excrete more urine, decreasing the volume of water in the body thus lowering blood pressure.4
Potassium-sparing diuretics, like an aldosterone antagonist, also reduce the amount of water in the body without also losing potassium.4 They are often prescribed with another diuretic to better control blood pressure and to help prevent low potassium levels.4
Carbonic anhydrase inhibitors help remove sodium, potassium, and water from the kidneys. Relatively weak diuretics, they are also are effective at reducing fluid levels in the eyes and are prescribed to treat glaucoma and sometimes used off-label to treat altitude sickness.4
Thiazide Diuretics And Metolazone
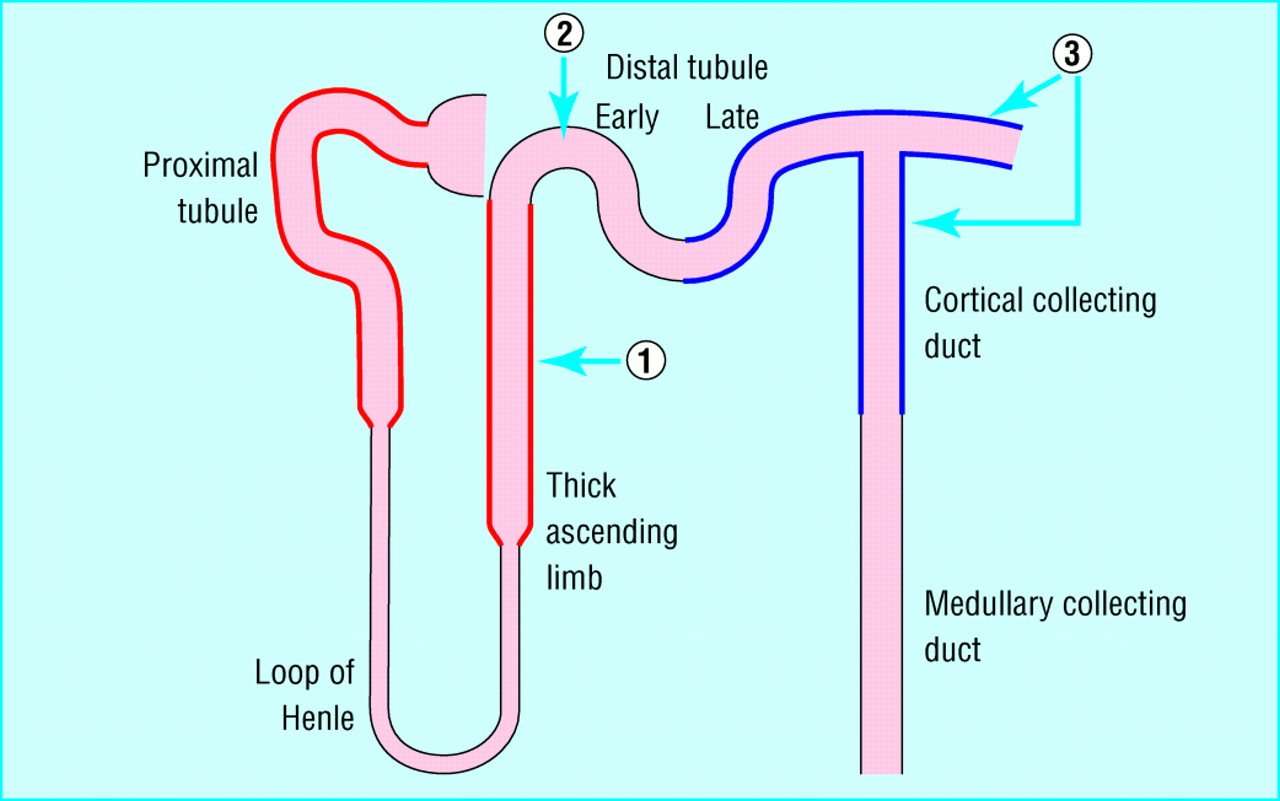
Thiazide diuretics inhibit sodium-chloride symporters at the distal portion of the ascending limb and the early part of the distal tubule, thereby increasing the excretion of sodium, chloride, and water across the renal tubular epithelium. Because they exert their diuretic effects from the luminal side of the nephron membrane, they must be adequately filtered in order to reach their site of action. Their effectiveness is therefore limited in patients with reduced glomerular filtration. Although they are less intrinsically potent than loop diuretics, they have synergistic effects with loop diuretics via sequential segmental nephron blockade. Metolazone is an oral quinazoline diuretic that is not a true thiazide but is a sulfonamide derivative with a similar site of action. Metolazone is much more potent than hydrochlorothiazide and remains effective even when the glomerular filtration rate is < 30mL/min, making it a useful adjunct to loop diuretics in patients with diuretic refractoriness or severe renal insufficiency.
Recommended Reading: Does Tylenol Increase Heart Rate
Aldosterone Receptor Antagonist Diuretics In The Treatment Of Congestive Heart Failure
Aldosterone is a hormone secreted by the adrenal gland . Aldosterone was classified as a mineralocorticoid hormone as it was found to play a major role in sodium reabsorption and potassium excretion. The primary action of aldosterone
Aldosterone receptor antagonists are a type of diuretic used in patients with CHF. They also have other properties that can prevent heart failure from becoming worse, along with improving symptoms of heart failure. Aldosterone receptor antagonists are proven to be beneficial in heart failure patients even if they are already on angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers .
- These medicines cause the kidneys to get rid of extra water and they help to retain potassium by inhibiting secretion of potassium into distal tubule of the nephron.
Because of this, they are called potassium-sparing diuretics.
Blocking the aldosterone receptor prevents an increase in aldosterone, ultimately preventing changes to the cardiovascular system and allowing for increased water excretion.
Most aldosterone receptor antagonists are used in conjunction with other medications, specifically Beta Blockers and Ace Inhibitors.
Alternatives To Diuretics: Future Directions
Given the limitations of traditional diuretics in heart failure, there has been substantial interest in developing alternative strategies to manage congestion and volume retention in heart failure patients. Vasopressin antagonists block the effects of vasopressin at the distal renal tubule, leading to an increase in free water excretion . The vasopressin antagonists conivaptan and tolvaptan are approved for the treatment of hyponatremia in heart failure patients. However, data on vasopressin antagonists in the broader heart failure population have been disappointing. In the Efficacy of Vasopressin Antagonism in Heart Failure: Outcome Study With Tolvaptan of patients hospitalized for ADHF, tolvaptan resulted in greater weight loss and in modest improvement in patient-reported dyspnea compared with placebo, both without worsening of renal function. However, tolvaptan did not demonstrate any long-term benefit on morbidity or mortality and is not currently approved for heart failure treatment.
Recommended Reading: Does Ibs Cause Heart Palpitations
Cardiovascular Effects Of Diuretics
Through their effects on sodium and water balance, diuretics decrease blood volume and venous pressure. This decreases cardiac filling and, by the Frank-Starling mechanism, decreases ventricular stroke volume and cardiac output, which leads to a fall in arterial pressure. The decrease in venous pressure reduces capillary hydrostatic pressure, which decreases capillary fluid filtration and promotes capillary fluid reabsorption, thereby reducing edema if present. There is some evidence that loop diuretics cause venodilation, which can contribute to the lowering of venous pressure. Long-term use of diuretics results in a fall in systemic vascular resistance that helps to sustain the reduction in arterial pressure.
What Are The Side Effects Of Diuretics
Frequent urination : This may last up to 6 hours after a dose.
Extreme tiredness or weakness: Both should get better as your body adjusts to the medication. If not, call your doctor.
Muscle cramps, thirst, loss of appetite, nausea, or vomiting: If you have any of these, make sure youâre taking your potassium supplement correctly, if you were prescribed one. Call your doctor if these symptoms last.
Dizziness, lightheadedness: Try getting up more slowly when youâre lying or sitting.
Blurred vision, confusion, headache, increased sweating, and restlessness: If these stick around a while or are severe, talk to your doctor.
Dehydration: Signs of this include:
- Dizziness
- You have to pee less
- Your pee is a dark color
- Rapid and excessive weight loss
Skin rash: Stop taking the medication and call your doctor right away.
Also Check: Claritin Heart Racing
Cardiac Medications For Prevention
The prescribing of ACE inhibitors, beta blockers and spironolactone in patients with heart failure presents the physician with challenges because while these agents do slow long-term decline related to heart failure, they have little or no effect on symptoms. In addition, it is not clear how quickly therapy should be started, whether all three approaches should be combined at once or which drugs should be added first. Research to date suggests benefit from all of the options in patients with an ejection fraction of less than 30 percent. A prudent approach would be to begin with an ACE inhibitor and spironolactone in most patients , slowly adding a beta blocker after the patient is stabilized on the first two drugs.
Spironolactone is contraindicated in patients with anuria, acute renal insufficiency, significant renal insufficiency or hyperkalemia. Potassium supplementation should not be combined with spironolactone. Other drug interactions include errors in measurement of and an increase in the half-life of digoxin, decreased effectiveness when used with salicylates and variable effects or side effects with use of nonsteroidal anti-inflammatory drugs. Gynecomastia and hyponatremia can occur, along with metabolic acidosis, which is usually associated with hyperkalemia. Other side effects are rare and include drug fever, drowsiness, lack of coordination, lethargy and gastrointestinal signs and symptoms.
How Do Diuretics Work
The kidney is made up of microscopic functional units known as nephrons. The nephrons produce certain proteins which help filter the wastes from the blood, and reabsorb minerals such as sodium, potassium and chloride for circulation in the blood. Diuretics inhibit the nephrons proteins, inducing the kidneys to flush minerals along with excess water.
Ethacrynic acid is rarely used except by those with sulfa allergies, as the other three are sulfonamide diuretics.
Thiazide and thiazide-like diuretics
Thiazide diuretics are commonly used to treat high blood pressure , but also to manage heart failure. Thiazide diuretics inhibit a different protein than the loop diuretics do, which also helps in mineral reabsorption. Thiazide diuretics include:
- Chlorothiazide
- Metolazone thiazide-like
- Potassium-sparing diuretics
Aldosterone is a hormone produced by the adrenal gland, which activates sodium absorption and potassium removal. Aldosterone antagonists block the release of aldosterone, preventing sodium absorption as well as potassium depletion. Following are the aldosterone antagonists currently available in the US:
- Triamterene
- Carbonic anhydrase inhibitor
A carbonic anhydrase is an enzyme that balances the blood pH levels. Carbonic anhydrase inhibitors block the enzyme, promoting the excretion of sodium, potassium, bicarbonate and water. The carbonic anhydrase inhibitor used for heart failure is:
Non-diuretic alternatives
You May Like: Typical Resting Heart Rate For A Healthy Individual
