Incorporate Other Healthy Lifestyle Changes One At A Time
Dont try to fix everything at once. Thats especially true if one of the habits you want to break is smoking.
Quitting smoking can be difficult. If you smoke, talk with your health care professional to determine if you need medications or other help to quit. Therapies may include nicotine replacement or prescription medicines. You could also ask for a referral for a smoking cessation program.
Ultimately, you have to take care of yourself to break the cycle of feeling down. That could be doing something structured, such as a yoga class or tai chi practice, or something you can do anywhere, such as meditating, listening to music or reading a book.
Written by American Heart Association editorial staff and reviewed by science and medicine advisers. See our editorial policies and staff.
Diagnosis Of Depression In People With Heart Disease
Diagnosing depression in people with heart disease is not always easy, because symptoms of depression, such as tiredness and low energy levels, are shared with heart disease or can be side effects of medication used to treat heart conditions.Doctors can screen for depression using questionnaires or interviews that address the symptoms of depression. Screening for depression should occur during your first visit to your GP for coronary heart disease, and at your next follow-up visit. If you have a major heart event such as a heart attack it is recommended that you be screened at two to three months after that event, and then on a yearly basis.This type of screening will help to detect any depression early so you can have treatment and improve your mental and physical health.
Regions That Affect Mood
Increasingly sophisticated forms of brain imaging such as positron emission tomography , single-photon emission computed tomography , and functional magnetic resonance imaging permit a much closer look at the working brain than was possible in the past. An fMRI scan, for example, can track changes that take place when a region of the brain responds during various tasks. A PET or SPECT scan can map the brain by measuring the distribution and density of neurotransmitter receptors in certain areas.
Use of this technology has led to a better understanding of which brain regions regulate mood and how other functions, such as memory, may be affected by depression. Areas that play a significant role in depression are the amygdala, the thalamus, and the hippocampus .
Research shows that the hippocampus is smaller in some depressed people. For example, in one fMRI study published in The Journal of Neuroscience, investigators studied 24 women who had a history of depression. On average, the hippocampus was 9% to 13% smaller in depressed women compared with those who were not depressed. The more bouts of depression a woman had, the smaller the hippocampus. Stress, which plays a role in depression, may be a key factor here, since experts believe stress can suppress the production of new neurons in the hippocampus.
You May Like: Which Of The Following Signs Is Commonly Observed In Patients With Right-sided Heart Failure
Can Depression Be Prevented
Many people wonder if depression can be prevented and how they may be able to lower their risk of depression. Although most cases of depression cannot be prevented, healthy lifestyle changes can have long-term benefits to your mental health.
Here are a few steps you can take:
- Be physically active and eat a healthy, balanced diet. This may help avoid illnesses that can bring on disability or depression. Some diets including the low-sodium DASH diet have been shown to reduce risk of depression.
Are Type As Addicted To Their Own Adrenaline Secretion
As previously proposed, I believe it is quite plausible that Type A is a self-perpetuating behavior due to stress induced adrenaline addiction. It is possible that other stress-related neurohumoral secretions such as serotonin, dopamine or beta-endorphin also have the potential for inducing addiction. Support for this comes from Solomons opponent-process theory of acquired motivation, which basically asserts that man is by nature susceptible to various habits and addictions that provide a sense of pleasure. However, when deprived of the thing that is craved, an opposing emotional state often results. The exhilarating feeling of being in love changes to melancholy if one is deprived of any contact with their beloved. People who are hooked on skydiving may become severely depressed if the weather interferes with their activities for a few days. Similarly, withdrawal from cigarettes, alcohol, narcotics, tranquilizers, or recreational drugs often produces an emotional state directly opposite from the pleasurable sensations those substances induce.
You May Like: Does Benadryl Lower Heart Rate
How Depression And Heart Disease Relate To Each Other
Depression and heart disease are among the most disabling diseases we face. They are both very widespread among the general population and often occur simultaneously in the same individual.
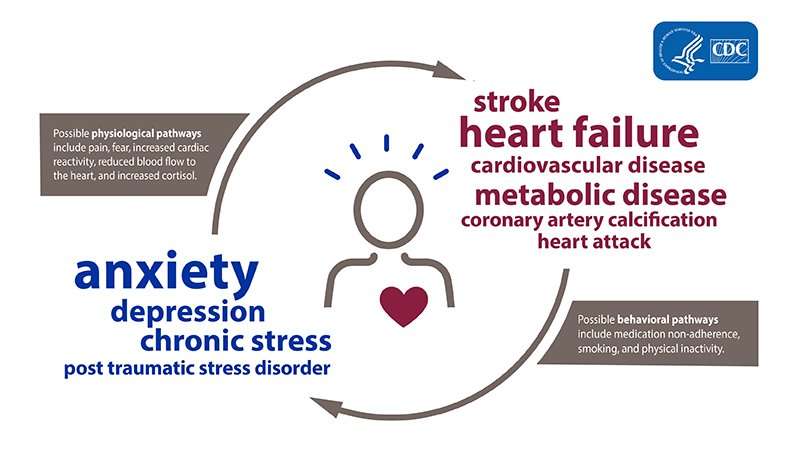
There is thought to be a two-way relationship between heart disease and depression:
A percentage of people with no history of depression become depressed after a heart attack or after developing heart failure. And people with depression but no previously detected heart disease, seem to develop heart disease at a higher rate than the general population.
It is somewhat hard to prove that heart disease directly leads to the development of a first-ever episode of depression. That is because some people who have had previous episodes of depression may not have it formally diagnosed until they see their doctor for heart problems.
What we can say with certainty is that depression and heart disease often occur together, says Dr. Roy Ziegelstein, vice dean for education at the Johns Hopkins University School of Medicine . About one in five who have a heart attack are found to have depression soon after the heart attack. And its at least as prevalent in people who suffer heart failure.
Selected Scientific Articles By Our Researchers
Developing effective collaboration between primary care and mental health providers. Felker BL, Chaney E, Rubenstein LV, Bonner LM, Yano EM, Parker LE, Worley LLM, Sherman SE, Ober S. Programs like TIDES that have implemented collaboration between primary care and mental health services have resulted in improved patient care. Prim Care Companion J Clin Psychiatry, 2006 8:12-16
Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. In this sample of outpatients with coronary heart disease, the association between depressive symptoms and adverse cardiovascular events was largely explained by behavioral factors, particularly physical inactivity. JAMA, 2008 Nov 26 300:2379-88.
Anxiety disorders increase risk for incident myocardial infarction in depressed and nondepressed Veterans Administration patients. Scherrer JF, Chrusclel T, Zeringue A, Garfield LD, Hauptman PJ, Lustman PJ, Freedland KE, Carney RM, Bucholz KK, Owen R, True WR. In VA patients free of heart disease in 1999 and 2000, those with depression, unspecified anxiety disorders, panic disorder and PTSD were at increased risk of heart attack. Am Heart J, 2010 May 159:772-9.
You May Like: What Heart Chamber Pushes Blood Through The Aortic Semilunar Valve
Can Certain Drugs Cause Depression
In certain people, drugs may lead to depression. For example, medications such as barbiturates, benzodiazepines, and the acne drug isotretinoin have sometimes been linked with depression, especially in older people. Likewise, medications such as corticosteroids, opioids , and anticholinergics taken to relieve stomach cramping can sometimes cause changes and fluctuations in mood. Even blood pressure medications called beta-blockers have been linked to depression.
Strengths And Limitations Of The Study
Our review strengths include the comprehensive search strategy, the development of themes from methodologically robust studies, the systematic approach to synthesis and the integration of both qualitative and quantitative data. We used one increasingly common approach to integrating mixed data although others exist . The sensitive search strategy employed meant that many non-relevant articles were found in the searches however this has hopefully ensured that no relevant articles were missed.
Recommended Reading: Flonase Heart Racing
The Pathophysiological Link Between Depression And Cad
There is growing evidence that several pathophysiological links exist that explain depressionâs effect on the cardiovascular system and may explain its role in CAD. Research is focusing on several mediators, seeking to identify how these mediators are activated by depression. Some of the more important mechanisms implicated are described in this section.
The hyperactivity of noradrenergic and hypothalamic pituitary adrenal corticol system. In CVD patients who are depressed, hyperactivity of the noradrenergic system is one important possible mechanism that may explain the association between depression and CAD. Sympathetic outflow is increased in depressed patients as compared to nondepressed patients through negative stress effects of catecholamines on the heart, blood vessels, and platelets. Further support of the catecholamine association with depression is that increased urinary catecholamines levels are associated with negative emotions and decreased social support,, and high norepinephrine and low platelets serotonin are associated with MI and depression.
Depression-induced altered autonomic tone associated with low heart rate variability leading to dysarrhythmias. Depressed patients may have decreased parasympathetic nervous system responses, leading to an imbalance between sympathetic nervous system and PNS.
Pharmacological Treatment Of Depression: Cardiovascular Implications
This section reviews the importance of treating depression in CAD patients and summarizes several studies addressing pharmacological treatment of depression in CAD patients.
Treating depression is critical in patients with CAD for several reasons. For example, in one study, reducing emotional distress in the short-term may improve long-term mortality in patients with CHD. Liaison between psychiatrists and general practitioners, where psychiatrists give advice to the general practitioners, was helpful in reducing the depressive symptoms of patients with CVD in another study.
The Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy and ENRICHD studies did not find the use of psychotherapy, i.e. interpersonal psychotherapy and cognitive behavioral therapy, substantially useful for the treatment of depression in CAD patients, thus highlighting the use of antidepressants in treatment of depression in this population.
We reviewed the Sequenced Treatment Alternatives to Relieve Depression study and provide strategies for using antidepressants. STAR*D is the largest study done on âreal-world patientsâ to assess the efficacy of antidepressant medications in patients with an average of three medical comorbidities and one psychiatric comorbidity. The study resulted in remission rates of approximately 47 percent at eight weeks of treatment with selective serotonin reuptake inhibitor monotherapy treatment.
Read Also: How To Calculate Target Heart Rate Zone
Iraq And Afghanistan Veterans And Depression
Many Iraq and Afghanistan Veterans have developed mental and behavioral conditions as a result of their combat experiences or other war-zone stressors. A 2015 study by researchers at VA’s Translational Research Center for TBI and Stress Disorders at the VA Boston Healthcare System identified three such conditions that cause the greatest level of difficulty in Veterans when they occur together.
The three conditions are depression, PTSD, and traumatic brain injury . Patients with those conditions, which the researchers call the “deployment trauma factor,” have higher disability scores than those with any other three-diagnosis combination.
The disabilities measured include difficulty in getting around, communicating and getting along with others, self-care, and other daily tasks. Other common problems that appeared to predict disability included anxiety conditions other than PTSD, pain along with sleep difficulty, and substance abuse or dependence.
Challenges Of Recognizing Depression Symptoms
Heart disease and depression often carry overlapping symptoms such as fatigue, low energy, and difficulty in sleeping and carrying on the daily rhythms of life. So its not surprising that sometimes symptoms of depression are thought of by the patient, the patients family, and the cardiologist as being due to heart disease.
Many members of the medical community have stressed the importance of having patients, families, and physicians gain a greater awareness of the prevalence of post-heart attack depression. Physicians need to understand the importance of treating depression, since it is treated differently from heart disease.
Meeting this challenge can result in a vital communication between patient and physician that can start with something as simple as, I wonder if what Im feeling is from depression.
Don’t Miss: Ibs And Heart Palpitations
Coping With Life’s Pressures
Heart disease has many other mind-body connections that you should consider. Prolonged stress due to the pressures at home, on the job, or from other sources can contribute to abnormally high blood pressure and circulation problems. As with many other diseases, the effects vary from person to person. Some people use stress as a motivator while others may “snap” at the slightest issue.
How you handle stress also influences how your cardiovascular system responds. Studies have shown that if stress makes you angry or irritable, you’re more likely to have heart disease or a heart attack. In fact, the way you respond to stress may be a greater risk factor for heart problems than smoking, high blood pressure, and high cholesterol.
Can Depression Cause Heart Disease Or Heart Attack
When you experience depression, anxiety or stress your heart rate and blood pressure rise, theres reduced blood flow to the heart and your body produces higher levels of cortisol, a stress hormone. Over time, these effects can lead to heart disease. Depression and anxiety can also develop after cardiac events, including heart failure, stroke and heart attack.
Don’t Miss: Typical Resting Heart Rate For A Healthy Individual
A New Theory On Depression: Its A Disease Caused By The Bodys Immune System
This article was published more than 2 years ago. Some information may no longer be current.
The idea that depression might be caused by a chemical imbalance in the brain and not a moral failing grew in popularity with the invention of the drug Prozac in the late 80s, and later with the marketing of this and other antidepressants.
This viewpoint helped reduce the stigma around mental illness, but did not provide a cure-all. Rates of depression have risen by more than 18-per-cent worldwide since 2005, according to the World Health Organization. At the same time, so too has the consumption of antidepressants. Canada has the worlds fourth-highest use of these drugs, according to a recent study from the Organisation for Economic Co-operation and Development.
Now, a new theory about the cause of depression has emerged: That it is a disease caused by the bodys immune system. The idea is that chronic stress causes hormonal dysregulation, and this leads to depression and other inflammatory disorders, such as arthritis, lupus, heart disease and even some forms of cancer.
One of Canadas leading proponents of this thesis is Dr. Diane McIntosh, a Vancouver-based psychiatrist, and assistant professor at the University of British Columbia and author of the new book, This is Depression: A Comprehensive, Compassionate Guide for Anyone who Wants to Understand Depression.
If cortisol is a key culprit, is stress a leading cause of depression?
Depression Contributes To Unhealthy Lifestyle And Poor Adherence To Treatment
Depression is associated with poor medication adherence, which may have an impact on treatment outcomes for cardiovascular disease. In an analysis of studies looking at depression and adherence, DiMatteo et al concluded that depression exhibited a significant relationship to nonadherence with treatment recommendations with an OR of 3.03 .
Patients with depression are also more apt to have an unhealthy lifestyle, choosing behaviors like smoking, sedentary lifestyle, drinking, and nonadherence with prescribed medications.â Depression is also related to poor secondary prevention behaviors like exercise and quitting smoking in patients with acute coronary syndromes . There is also a higher incidence of depression among severely obese patients, which may have implications for changing to more healthy lifestyles.
Read Also: Does Higher Heart Rate Burn More Calories
What Is Type A Coronary Prone Behavior
In 1959, a paper by Meyer Friedman and Ray Rosenman appeared in the Journal of the American Medical Association entitled Association of specific overt behavior patterns with blood and cardiovascular findings: Blood cholesterol level, blood clotting time, incidence of arcus senilis and clinical coronary artery disease. The subtitle linking specific behavioral traits with things like blood cholesterol, clotting time, arcus senilis and coronary disease that had no apparent relationship to each other must have seemed strange to many readers. Neither of these two cardiologists had any expertise in psychology, which may have been fortuitous, since they had no preconceived notions. What they did have was an unusual combination of curiosity, diagnostic acumen and a bio-psychosocial approach to the patient as a person, rather than someone to be treated in a cookbook fashion based on laboratory tests, symptoms or signs.
Such individuals exhibited certain characteristic activity patterns, including.
About Heart Disease And Mental Health
You may know that coronary heart disease is the leading cause of death in Australia. But did you know that your mental health can affect your heart health and your heart health can affect your mental health?
Heart conditions such as heart attack and angina are also known as cardiovascular disease. These conditions are more common in people living with depression, compared to the general population. In fact, we now know depression is a considerable risk factor for coronary heart disease along with smoking, high cholesterol and high blood pressure. Less is known about the links between anxiety and heart disease, but we do know that many people with anxiety also have depression.
Depression can also affect how well people with heart disease recover and increase their risk of further heart problems. So, let’s learn some more about the links between heart health and mental health.
Read Also: Heart Palpitations Prednisone
Rein In The Rage: Anger And Heart Disease
Experts explore the connection between anger and heart disease, and give tips for getting your anger under control.
If a caller upsets you, do you hurl the phone across the room? Do you curse and blast the horn furiously if the driver in front of you takes three seconds to notice the green light? An angry temperament can hurt more than relationships — anger and heart disease may go hand in hand, according to experts.
“You’re talking about people who seem to experience high levels of anger very frequently,” says Laura Kubzansky, PhD, MPH, an assistant professor at the Harvard School of Public Health who has studied the role of stress and emotion on cardiovascular disease.
Moderate anger may not be the problem, she says. In fact, expressing one’s anger in reasonable ways can be healthy. “Being able to tell people that you’re angry can be extremely functional,” she says.
But explosive people who throw things or scream at others may be at greater risk, as well as those who harbor suppressed rage, she says. “Either end of the continuum is problematic.”
Gender doesn’t appear to make much difference, she adds. “Once people are chronically angry, men and women seem to be at equally high risk.”
Scientists don’t all agree that anger plays a role in heart disease, she says. But many studies have suggested a significant link. “I think the case is strong,” Kubzansky says.
