Stroke Prevention In Patients With Af And Concomitant Hf
Anticoagulation
In HF trials, the prevalence of AF ranges from 10% to 50%, with 21% to 68% of subjects having persistent or permanent AF.23 Both AF and HF increase the risk of thromboembolic complications. According to the CHA2DS2VASc score, most patients with AF and HF are expected to be candidates for anticoagulation with a vitamin K antagonist or direct oral anticoagulants unless contraindicated.34 In fact, data from the Get With The Guidelines AF Program demonstrated that 95% of patients with AF and HF were discharged on an anticoagulant: 44% on warfarin and 51% on DOAC.35 A cross-sectional outpatient registry of 429417 patients with AF, however, demonstrated much lower adherence, with fewer than half of the high-risk patients receiving an oral anticoagulant prescription. Only 24.9% of the study population had a history of HF, and an analysis of this subgroup was not reported. Moreover, the data were collected from 2008 to 2012, and warfarin was used in 90.3% of those receiving oral anticoagulation.36
In patients with HFrEF who undergo CA for AF, the 2020 European Society of Cardiology/European Association of Cardio-Thoracic Surgery AF guidelines recommend continued oral anticoagulation with warfarin or a DOAC for at least 2 months after ablation. Long-term oral anticoagulation beyond that should be determined by the patients stroke risk profile, not by success or failure of CA .33
Prognosis Of Patients With Atrial Fibrillation And Heart Failure
Despite the knowledge of the association between atrial fibrillation and heart failure, the data regarding the joint prognosis of these two conditions are conflicting.14 A retrospective study of 390 patients with advanced heart failure found that patients with atrial fibrillation had significantly higher mortality rates than those in sinus rhythm, despite similarities in heart failure etiologies, pulmonary capillary wedge pressures, left ventricular ejection fractions, and the presence of
When Should I See My Healthcare Provider
Theres no single schedule to follow. It all depends on your symptoms and treatment plan, and whether you need follow-ups after a procedure. So, its important to talk with your provider and make a plan together. Make sure you go to all your scheduled appointments. Keep track of the medications youre taking, and bring a list of your medications to every appointment. Its also a good idea to keep the list in your wallet so its with you in emergencies.
What should I discuss with my healthcare provider?
At each visit, be sure to share any new symptoms or problems youre having, such as side effects from medication.
Your provider will ask you questions, but its important to ask your own questions, too. For example, ask for advice on how to reduce your risk factors. Starting a new diet or exercise plan can feel overwhelming. Your provider will offer advice and also connect you with others who can help, such as dietitians. You may also want to ask about available health and fitness programs, including those that support your mind-body connection.
Finally, be sure to ask your provider before taking over-the-counter medicines, such as those for cold and flu, and nutritional supplements. Sometimes these products can affect your heart rate or interact with your prescription medications.
A note from Cleveland Clinic
Read Also: Congestive Heart Failure Chf
Atrial Cardiomyopathy: From Cell To Bedside
Stroke Centre and Department of Neurology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
Department of Neurology, Shaanxi People’s Hospital, Xi’an, China
Gary Tse
Kent and Medway Medical School, Canterbury, UK
Tianjin Key Laboratory of Ionic-Molecular Function of Cardiovascular Disease, Department of Cardiology, Tianjin Institute of Cardiology, Second Hospital of Tianjin Medical University, Tianjin, China
Stroke Centre and Department of Neurology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
Correspondence to: Guogang Luo, Stroke Centre and Department of Neurology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China. Email:
Guoliang Li, Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China. Email:
Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
Correspondence to: Guogang Luo, Stroke Centre and Department of Neurology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China. Email:
Guoliang Li, Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China. Email:
Stroke Centre and Department of Neurology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
Department of Neurology, Shaanxi People’s Hospital, Xi’an, China
Gary Tse
Atrial Fibrillation And Congestive Heart Failure
DOI: 10.19102/icrm.2011.020404
1Department of Internal Medicine, Charlton Memorial Hospital, Fall River, MA2Cardiac Arrhythmia Service, Massachusetts General Hospital, Boston, MA
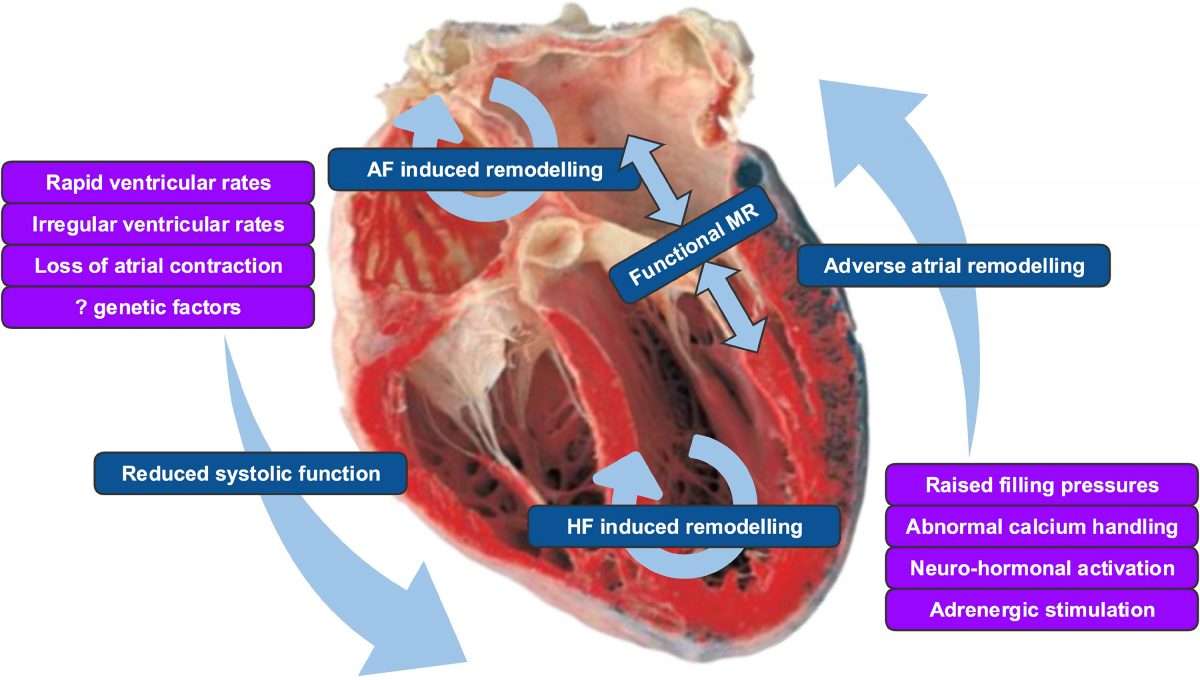
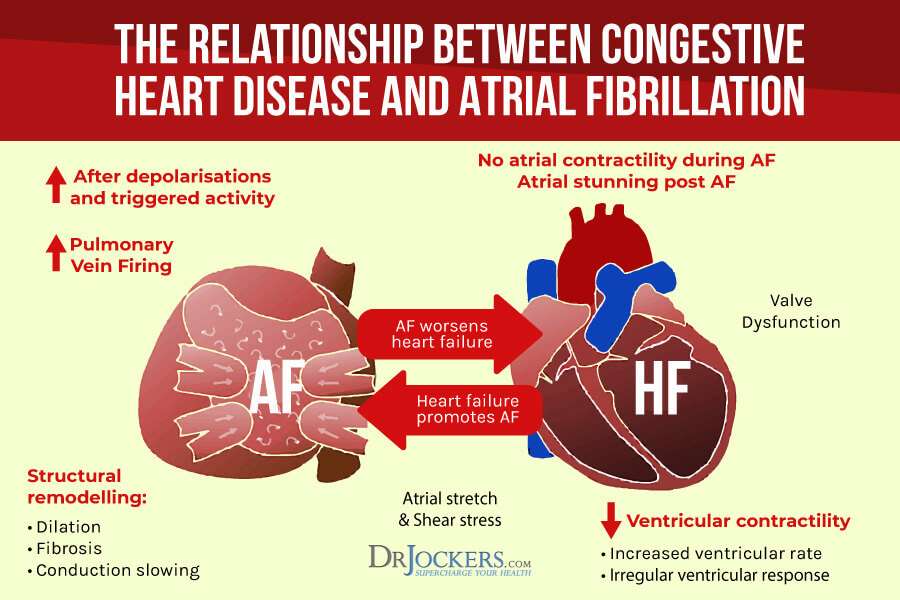
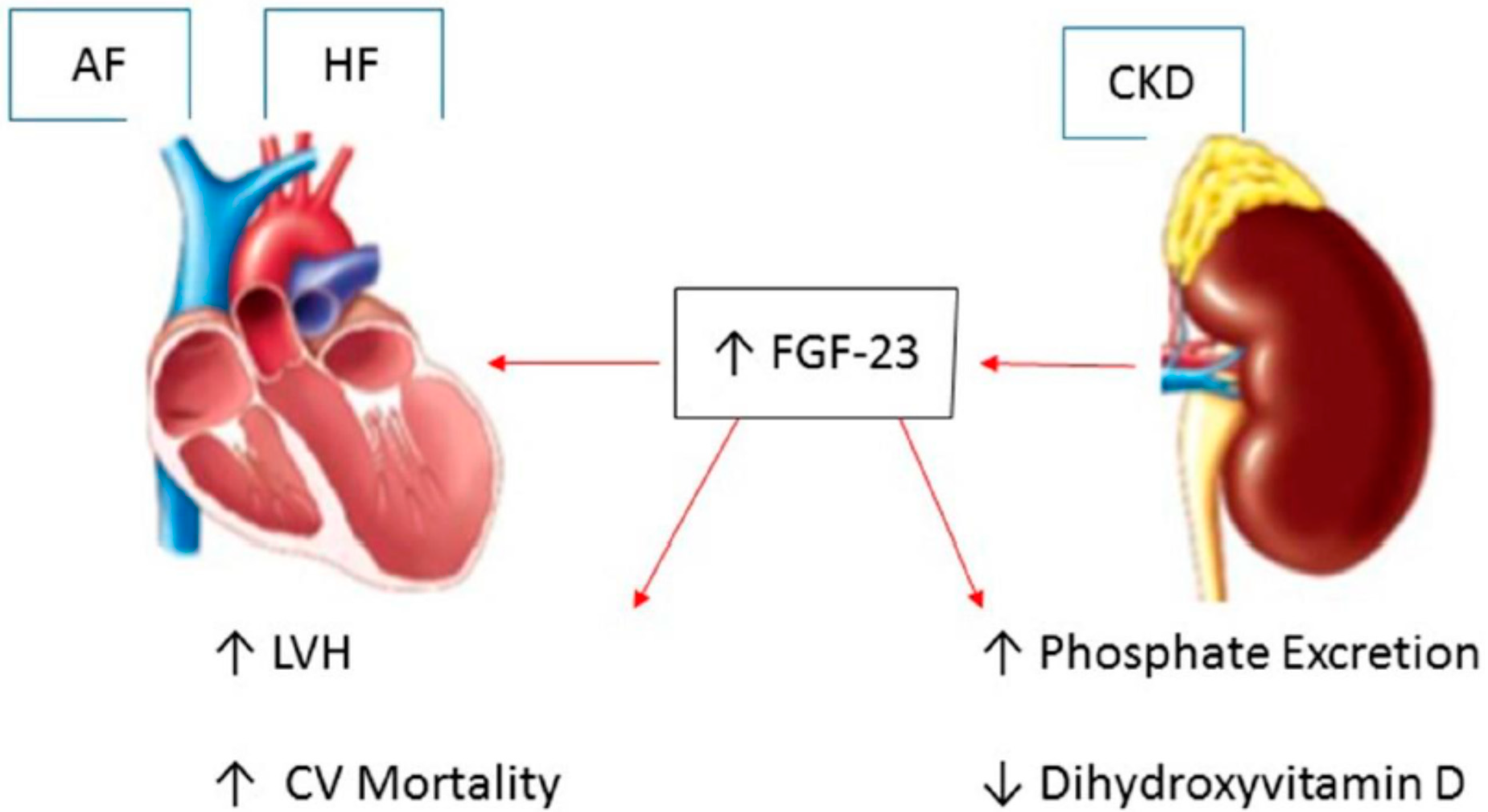
ABSTRACT.Atrial fibrillation and congestive heart failure are common conditions which predispose each other, share risk factors, and are associated with morbidity and mortality. They share common pathophysiology, including structural and electrical remodeling, intracellular calcium dysregulation, and neuroendocrine mechanisms, and also have genetic basis. Despite better survival in patients with sinus rhythm than those with AF, rhythm control has not been found to be superior to rate control. The role of non-antiarrhythimc therapy is also being explored. Catheter ablation and device-based therapy with pacemaker and cardiac resynchronization therapy may also benefit patients with AF and CHF.
KEYWORDS.ablation, antiarrythmic drugs, atrial fibrillation, genetics, heart failure.
The authors report no conflicts of interest for the published content. Manuscript received February 13, 2011, final version accepted March 3, 2011.
Address correspondence to: E. Kevin Heist, MD, PhD, Cardiac Arrhythmia Service, 55 Fruit Street, Massachusetts General Hospital, Boston, MA. E-mail:
Recommended Reading: Can Antihistamines Cause Heart Palpitations
Management Of Concomitant Heart Failure And Reduced Ejection Fraction And Atrial Fibrillation
Currently, clinicians often manage patients with combined HFrEF and AF by focusing on particular therapeutic aspects that have an evidence-base in one or other of these conditions . Researchers have started to investigate if treatment efficacy differs in patients with concomitant disease, but at present these data are limited. In this section, we summarize the evidence-base for common treatment modalities and suggest a simple clinical mnemonic for the initial management of newly diagnosed concomitant HF and AF. The CAN-TREAT HFrEF + AF algorithm distinguishes the management of these patients from those with sinus rhythm. The presence of haemodynamic instability should be treated with urgent cardioversion . Anticoagulation should be instituted to prevent thromboembolism, and diuretic therapy to normalize fluid balance and reduce symptoms of HF. Subsequent therapy should target an initial heart rate < 110 b.p.m. and initiate RAAS antagonism , though with limited data on efficacy . Early rhythm control in patients with symptoms refractory to rate control, and consideration of advanced HF therapies should follow , with aggressive treatment of other concomitant CV disease, particularly ischaemia and hypertension.
CAN-TREAT initial management algorithm for patients with newly identified heart failure and reduced ejection fraction and atrial fibrillation. ACEi, angiotensin converting enzyme inhibitors ARB, angiotensin receptor blockers CV, cardiovascular.
How Do I Manage Atrial Fibrillation
Your doctor will develop a plan to manage your atrial fibrillation based on the options that are best for you. Some options include:
- medications to control heart rate and rhythm
- medications to thin the blood
- controlled electric shocks to the heart
- a procedure to destroy the area of the heart that is causing the electrical malfunction or to limit heart rate.
Recommended Reading: How To Decrease Resting Heart Rate
How Does Afib Lead To Additional Heart Rhythm Problems
Basic answer: The hearts electrical system stops working properly, and fails to keep the heart chambers in rhythm.
Thorough answer: Every heartbeat is controlled by the hearts electrical system. To understand why atrial fibrillation is a problem, it is helpful to understand the normal patterns of the hearts electrical system.
Family History And Genetics
If someone in your family has had atrial fibrillation, you have a higher risk of developing atrial fibrillation, too. Scientists have found somegeneswithmutationsthat raise the risk of atrial fibrillation. Some of these genes influence fetal organ development or heart cellionchannels.
Sometimes these genetic patterns are also linked to heart disease. Some genetic factors may raise the risk of atrial fibrillation in combination with such factors as age, weight, or sex.
Don’t Miss: What To Do When Having A Heart Attack Alone
Facts About Afib Life Expectancy
Atrial fibrillation can impact your health and life span in a number of ways. Overall, mortality rates are four times higher in people with atrial fibrillation than in the general population, although the specific cause of death varies greatly.
Deaths linked to Afib dropped in the early part of the 21st century before hitting a plateau, but mortality rates associated with Afib have been risingespecially in younger peoplesince about 2011.
Mortality rates with Afib aren’t usually directly linked to the condition itself, but rather to the complications that arise from it. The leading causes of death related to atrial fibrillation include:
- Cerebral infarcts or ischemic stroke
How Heart Failure Leads To Afib
It works in the other direction, too. Your heart’s rhythm is controlled by electrical signals. For those signals to work well, they need healthy heart tissue.
But heart failure can actually stretch your atria and cause tissue in your heart to thicken and scar. Those changes throw off the electrical signals, and that messes up the heart’s rhythm and can cause AFib.
Read Also: How To Check Heart Rate On Apple Watch
Af And Chf: Therapeutic Approaches
Rate or rhythm control
In a substudy of Danish Investigations of dysrhythmia and mortality on Dofetilide trial and in CHF-STAT the subgroup of heart failure patients who maintained sinus rhythm demonstrated reduced mortality., The Atrial Fibrillation in Congestive Heart Failure trial, a large multicenter prospective randomized trial, involving 1,376 patients which assessed cardiovascular mortality among patients with concomitant AF and CHF treated with a rate or rhythm control strategy, did not describe any morbidity or mortality benefit or any improvement in secondary outcome of rhythm over rate control. SWORD , a trial of d-sotalol in patients with LVEF â¤40% post myocardial infarction demonstrated increased mortality with d-sotalol use compared with placebo. SWORD was not a trial looking specifically at AF patients, but does raise concern about the use of this class of antiarrhythmic drugs in patients with CHF post myocardial infarction.
Antiarrhythmic therapy
Class I agents: sodium channel blockers
These are commonly used for patients with structurally normal hearts and AF but avoided in patients with CHF and ischemic heart disease as they may increase mortality.
Class III agents: potassium channel blockers
Rate control
Other drug therapies
Anticoagulation
How Is Afib Related To Stroke
AFib increases a persons risk for stroke. When standard stroke risk factors were accounted for, AFib was associated with an approximately fivefold increased risk of ischemic stroke.6 AFib causes about 1 in 7 strokes.7
Strokes caused by complications from AFib tend to be more severe than strokes with other underlying causes. Strokes happen when blood flow to the brain is blocked by a blood clot or by fatty deposits called plaque in the blood vessel lining.
Read Also: Can Statins Cause Heart Palpitations
When To Talk To Your Doctor
If you have symptoms of atrial fibrillation, it is important to talk to your doctor to confirm a diagnosis. Feeling your heart racing is not uncommon and is usually not AF, but it’s important to talk to your doctor about it to get the correct diagnosis.
If you’ve already been diagnosed with AF, it’s important to keep track of your symptoms. If they get worse or change over time, you should discuss these changes with your doctor. It may be that your medication needs to be adjusted or that you need another kind of treatment.
Dr Fraser Hamilton talks about how common atrial fibrillation is and what it means for you to have the condition.
If you’re experiencing chest pain and other heart attack warning signs call 111 immediately.
Discussing atrial fibrillation with your doctor
Record any symptoms you’re experiencing , when they occurred and what you were doing at the time.
Write down key personal information, including any family history of heart disease, stroke, high blood pressure or diabetes and any major stresses or recent life changes.
Make a list of all medications, vitamins or supplements that you’re taking.
Take a family member or friend along if possible. Sometimes it can be difficult to understand and remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
Write down questions to ask your doctor. Common questions about atrial fibrillation include:
How Is Atrial Fibrillation Diagnosed
If your pulse is fast and has an irregular beat, your doctor may think you have atrial fibrillation. A painless test that shows a graph of the electrical activity of the heart, called an electrocardiogram , can confirm whether or not you have atrial fibrillation. You may also be asked to wear a Holter monitor, which is a small portable device that records and saves a series of ECGs over a specific time period .
Don’t Miss: What Kind Of Jaw Pain Is Associated With Heart Attack
Electrical Problems In Atrial Fibrillation:
- In AFib, the SA node may not start the contraction. Instead, the contraction might start randomly in other areas of the atria or even in the pulmonary veins.
- In AFib, the electrical current doesnt flow in an organized top-to-bottom fashion. Instead, contractions are rapid and disorganized.
- In AFib, the AV node often cant regulate the chaotic current. It does its best to protect the ventricle from extra electrical impulses, but it cant stop all of them. As a consequence, the ventricle beats more often than it should giving rise to the noticeable symptoms of breathlessness and fatigue.
- When the beat is off, the blood supply can be unpredictable. So, even though the ventricles may be beating faster than normal, they aren’t beating as fast as the atria. Thus, the atria and ventricles no longer beat in a coordinated way. This creates a fast and irregular heart rhythm. In AFib, the ventricles may beat 100 to 175 times a minute, in contrast to the normal rate of 60 to 100 beats a minute.
The amount of blood pumped out of the ventricles to the body is based on the randomness of the atrial beats.
The body may get rapid, small amounts of blood and occasional larger amounts of blood. The amount will depend on how much blood has flowed from the atria to the ventricles with each beat.
Prevalence Of Atrial Fibrillation And Heart Failure
A complex relationship exists between heart failure and atrial fibrillation. Chronic heart failure affects more than 50% of patients with atrial fibrillation.10 The prevalence of atrial fibrillation has been observed to increase in proportion to the severity of chronic heart failure.11, 12, 13 Recent data have shown that the total proportion of heart failure patients with atrial fibrillation at any time was 41%. Forty-two percent of subjects with atrial fibrillation developed heart failure at
Don’t Miss: How To Stop Worrying About Heart Attack
Premature Menopause Women Are At Higher Risk Of Heart Failure And Atrial Fibrillation
A Korean population-based study that showed that premature menopause before the age of 40 is closely related to an increased risk of heart disease caught the attention of academia.
The European Heart Association paid attention to Professor Nam Ga-euns thesis of Family Medicine at Korea University Guro Hospital published in the European Heart Journal, the official journal of the Society, through a press release on the 4th .
Cardiovascular disease typically occurs up to 10 years later in women than men, ESC said. It could make them more susceptible to disease.
Early menopause affects about 1% of women under the age of 40, he said. Or, the evidence for individual diseases of atrial fibrillation was limited.
According to Professor Nams paper, menopause before the age of 40 is associated with an increased risk of heart failure and atrial fibrillation.
Professor Nams study investigated the association between early menopause and age at menopause, and heart failure and atrial fibrillation. The data were obtained from the National Health Insurance data, which conducts health checkups at least once every two years, which included 97% of the total population.
The analysis included 1,401,175 postmenopausal women aged 30 years and older who had a health checkup in 2009, and they were followed up for new onset heart failure and atrial fibrillation until the end of 2018.
Changes In Heart Tissue
Aging, heart disease, infection, genetics, or other factors change heart tissue and can keep the heart cells from working together to contract in rhythm. This can happen because of fibrosis, inflammation, thinning or thickening of the heart walls, less blood flow to the heart, or a buildup of protein, cells, or minerals in heart tissue.
Recommended Reading: What Happens After A Mild Heart Attack
Rationale For Rhythm Control In Atrial Fibrillation And Heart Failure
What is the optimal management of this subset of patients who have concomitant heart failure and atrial fibrillation, and what is the rationale? The loss of atrial transport and an irregular ventricular rhythm both make important contributions to the worsening of cardiac output and other hemodynamic parameters. The subsequent hemodynamic changes may then explain the clinical alterations that are observed in this population.
The clinical and hemodynamic consequences of developing atrial
Can You Prevent Atrial Fibrillation
- To help you lower your risk of atrial fibrillation, your doctor may recommend certainheart-healthy lifestyle changes, including aiming for a healthy weight, being physically active, controlling your blood sugar, limiting alcohol, lowering your blood pressure, managing stress, and quitting smoking.
- Some illegal drugs, such as cocaine, can trigger atrial fibrillation or make it worse. If you use illegal or street drugs, ask your provider how to get help to stop. You can also call the Substance Abuse and Mental Health Services Administrations National Helpline at 1-800-662-HELP.
- If you are having heart surgery, your medical team will monitor you. To prevent arrhythmia, your doctor may recommend antiarrhythmic medicine or treatment to maintain or supplementelectrolytelevels during or after the procedure.
Read Also: What Is The Normal Resting Heart Rate For A Woman
