Types Of Cardiomyopathy & Heart Failure
NYU Langone heart specialists are familiar with all types of cardiomyopathy, which means sickness of the heart muscle. This condition changes the shape and function of the heart. It reduces the hearts ability to pump blood and can cause heart arrhythmias, in which the heart beats too slowly or quickly.
Schedule an Appointment
Heart failure occurs when conditions such as cardiomyopathy, heart valve disease, or congenital heart disease damage the heart, reducing its ability to pump blood to the body.
Despite its name, heart failure isnt a complete loss of heart function, as occurs in sudden cardiac arrest, when the heart suddenly stops beating. Heart failure means the organ isnt pumping blood to the rest of the body as well as it should. This is a serious and progressive conditionyet manageable.
Doctors use a test called an echocardiogram to determine the percentage of blood the heart pumps with each contraction. This is called ejection fraction. A normal hearts ejection fraction is typically between 55 percent and 70 percent. The ejection fraction number is used to describe different types of heart failure or cardiomyopathy.
Are There Different Types Of Ejection Fractions
Measurements can be taken on either the left or right ventricle.
Left ventricular ejection fraction
Ejection fraction typically refers to the left side of the heart. It shows how much oxygen-rich blood is pumped out of the left ventricle to most of the bodys organs with each contraction. LVEF helps determine the severity of dysfunction on the left side of the heart.
Right ventricular ejection fraction
This measures the amount of oxygen-poor blood pumped out of the right side of the heart to the lungs for oxygen. It is important if you have right-sided heart failure. But this condition is not as common as left-sided heart failure.
Aha/acc/hfsa Heart Failure Guideline: Key Perspectives
- Heidenreich PA, Bozkurt B, Aguilar D, et al.
- Citation:
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022 Apr 1:.
The following are key perspectives from the 2022 American Heart Association /American College of Cardiology /Heart Failure Society of America Guideline for the Management of Heart Failure:
Don’t Miss: Congestive Heart Failure In Dogs Symptoms
Anemia And Iron Deficiency
Anemia is common among patients with chronic heart failure and is frequently multifactorial. Anemia is associated with worse symptoms and outcomes in HF and so reversible causes should be sought and treated. Iron deficiency Iron Deficiency Anemia Iron deficiency is the most common cause of anemia and usually results from blood loss malabsorption, such as with celiac disease, is a much less common cause. Symptoms are usually nonspecific… read more is among the most common causes of anemia in HF, and iron replacement therapy should be considered once treatable causes such as blood loss have been excluded. Oral iron replacement is often less effective due to poor absorption and other reasons, thus intravenous iron replacement is preferred.
Advanced Therapies And Palliative Care
Patients deteriorating despite optimal medical and device therapy may follow one of two trajectories. A small group of patients may be eligible for mechanical circulatory support, according to INTERMACS classification, and consideration of cardiac transplantation. Early discussion±referral for specialist assessment at a transplant centre in an appropriate patient should always be considered. Prompts for referral include frequent hospitalisation, worsening symptoms, reduced ability to tolerate medical therapy and requirement for inotropic support. Many patients with HFrEF are elderly or will have comorbidity which precludes consideration of cardiac transplantation. These patients require good palliative care, hand-in-hand with their ongoing supported self-management. Experience shows that involvement of these services earlier in the care pathway can be highly beneficial. Recognising the deteriorating patient and developing an appropriate advanced care plan should be the natural progression of care for all members of the wider MDT.
Don’t Miss: Women Heart Attack Symptom
Enhancing Healthcare Team Outcomes
Heart failure is a leading cause of hospitalization and represents a significant clinical and economic burden. The long-term goal of treatment is to avoid exacerbation of HF and decrease hospital readmission rates. It needs an interprofessional approach involving patients, physicians, nurses, pharmacists, families, and caretakers. Those strategies include early identification of high-risk patients, patient education, improving medication and dietary compliance, assuring close follow up, introducing end-of-care issues, and tele-home monitoring if available. Primary care and emergency department providers often are the first to make this diagnosis. Referal to cardiologists is often appropriate. Cardiology, medical/surgical, and critical care nurses administer treatment, provide education, monitor patients, and communicate with the rest of the team so that everyone on the healthcare team operates from the same data set. The managing clinician would do well to consult with a board-certified cardiology pharmacist when initiating pharmaceutical care in HF cases. Pharmacists also review medicines, check the dosages, detect drug-drug interactions, and stress to patients and their families the importance of compliance. In end-stage cases, hospice care and hospice nurses can work with the patient and their family to provide comfort care. These interprofessional collaborations will optimize patient outcomes in HF cases.
What Is Ejection Fraction
Ejection fraction is a measurement, expressed as a percentage, of how much blood the left ventricle pumps out with each contraction. An ejection fraction of 60 percent means that 60 percent of the total amount of blood in the left ventricle is pushed out with each heartbeat.
This indication of how well your heart is pumping out blood can help to diagnose and track heart failure.
Also Check: Does Losartan Lower Heart Rate
What Is Heart Failure
Heart failure means that the heart is not pumping blood efficiently and cant keep up with the bodys needs. Heart failure does not mean that the heart has stopped functioning or will stop at any moment. However, heart failure is a serious, chronic condition that must be managed.
Symptoms of heart failure may include:
- Shortness of breath
If your doctor suspects heart failure based on your symptoms and other health factors, they may order tests to measure your hearts ejection fraction.
Box 1 Implications Of Variability In Ef Measurements
-
Intraobserver and interobserver variability of standard echocardiographic left ventricular ejection fraction assessment is reported to be 821% and 613%, respectively
-
Digit-rounding bias: the tendency is to report EF with numbers ending in 0 or 5, for example as 40% instead of 39% or 41%. Therefore, whether heart failure with mildly reduced EF is defined as EF 4049% or 4149% can have major implications for estimating the prevalence of HFmrEF
-
Regression to the mean
-
Visual estimation: although reliability has been reported as sufficient,, visual estimation can underestimate true EF values
-
Poor image quality
-
Measurement error, in particular in the setting of rapid and/or irregular ventricular rhythm
-
Consequences of measurement variability
-
Misclassification: in randomized clinical trials, estimation of EF at local sites can lead to the misclassification of patients for enrolment. In the TOPCAT trial, core laboratory measurements would have reclassified about 20% of the EF measurements
Future perspectives
Optimization of automated algorithms for the analysis of EF
Systematic adoption of core laboratories fulfilling standard requirements for randomized clinical trials that are based on EF
Improved agreement between imaging techniques: substantial variability in the estimation of EF has been reported across imaging modalities even when quantified by core laboratories
Integrating EF with additional criteria for more accurate and precise categorization of heart failure
Recommended Reading: Why Is My Heart Rate Always High
What Is Too Low
Ejection fractions are grouped by the percentage of blood volume pumped out from the heart.2 An EF from 41 to 49 may be considered borderline. EF is not always an indication of heart failure. For example, it can reflect prior damage from a previous heart attack. As the severity of HF increases, the ejection fraction can get lower. An EF measurement under 40% is generally considered evidence of heart failure and at 35% or lower there is a high risk of developing dangerous changes in heart rhythm that can cause sudden cardiac arrest or death.3
How Can I Improve My Ejection Fraction
Heart failure therapies treat the underlying cause of low ejection fraction. For heart failure due to an arrhythmia, you may benefit from a biventricular pacemaker. People with heart failure due to other causes, like high blood pressure, may need medications.
You can take additional steps to relieve strain on your heart and get the most out of treatment. These include:
- Increasing physical activity. A cardiac rehabilitation program can help you safely get started.
- Maintaining a healthy weight.
- Limiting the amount of sodium and volume of fluids you consume.
- Quitting unhealthy habits, such as smoking, recreational drugs and alcohol.
You May Like: When Checking Your Pulse During Exercise, You Should Measure Your Heart Rate For 30 Seconds.
Why Is The Term Ejection Fraction Important
Assessment of EF has been used in drug trials during the last decades when attention was mainly focused on patients with HFrEF. Only recently, have we recognized the frequency of heart failure symptoms due to impaired relaxation of the heart muscle as opposed to reduced contraction . These different categories of patients usually require somewhat different drug treatment. In that most of the research on treatment has been performed on patients with HFrEF, the evidence confirming effective treatment is best for these patients and therefore treatment guideline recommendations are strongest for patients with HFrEF. However, more recently, there is great interest in research into the most effective therapy in patients with HFpEF. Currently, treatment is based on treating the individuals symptoms.
This single and simple measurement of EF by echocardiography is a helpful tool for clinicians designing an individual management plan for patients with heart failure.
What Is A Normal Ejection Fraction
Ejection fraction in a healthy heart is 50% to 70%. With each heartbeat, 50% to 70% of the blood in your left ventricle gets pumped out to your body.
Ejection Fraction Percentage
| 30% to 40% | Below 30% |
Some people with a normal ejection fraction also have heart failure. This is known as heart failure with preserved ejection fraction .
Why is it important to know my ejection fraction?
Your ejection fraction is an indicator of how well your heart is working. A low ejection fraction typically means you have or are at risk for heart failure.
Also Check: Open Heart Surgery Name
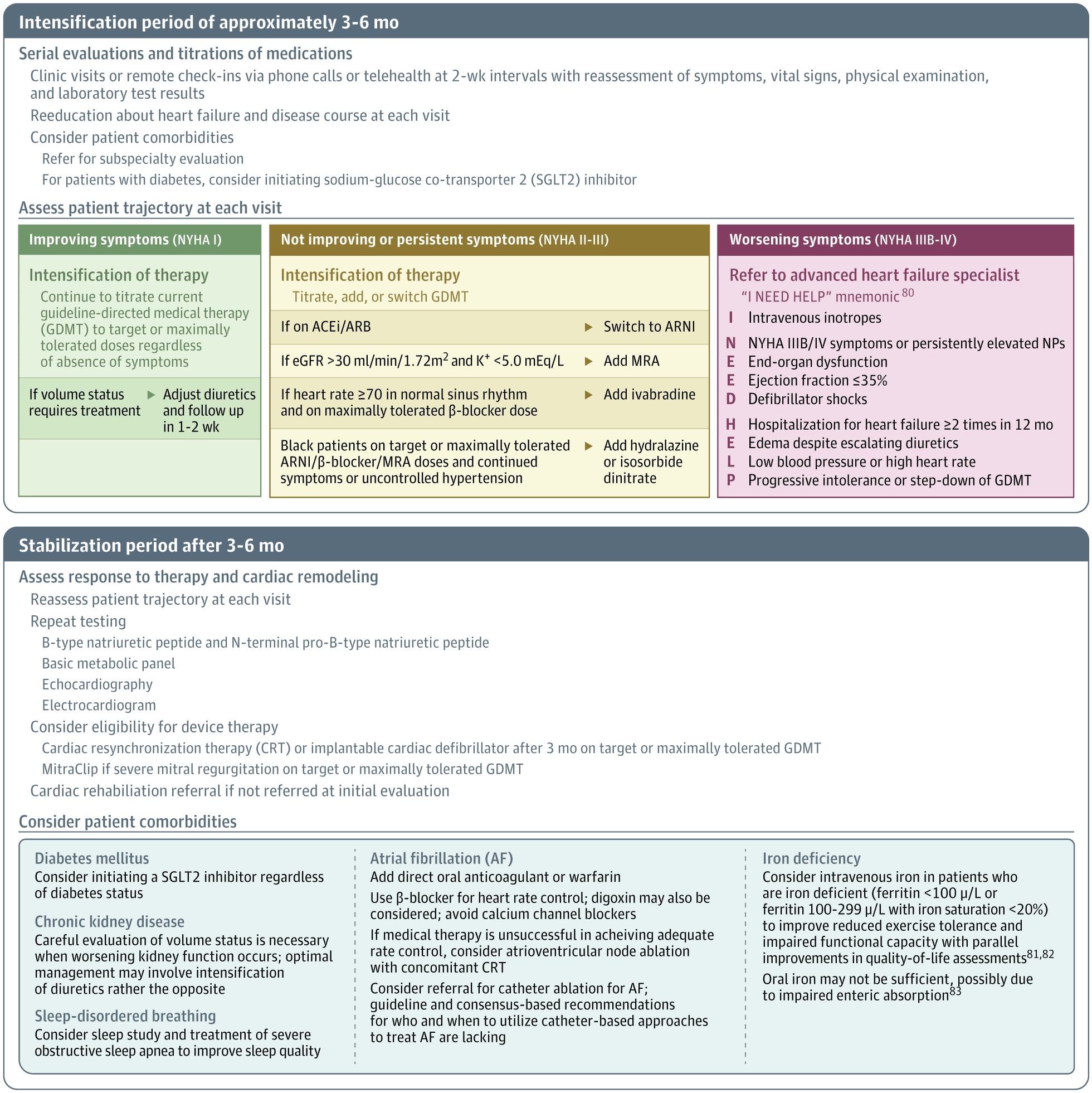
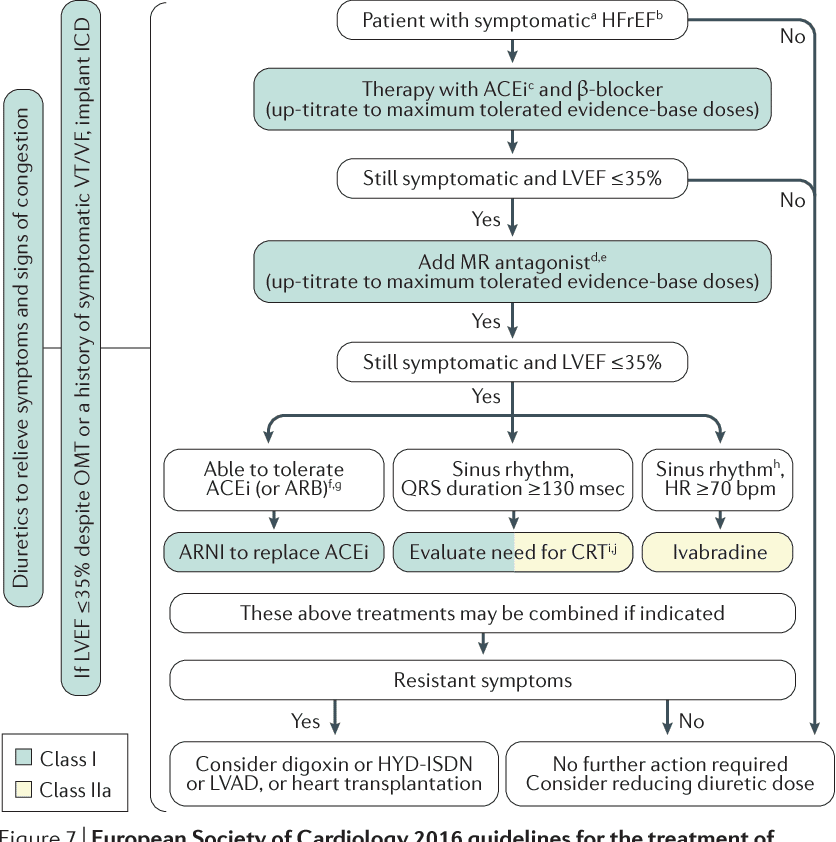
Titration Schedules And Drug Sequences Examined
shows the conventional sequence of treatments using, in order a RASi, a beta-blocker, an MRA, an ARNI , and an SGLT2i. also shows an accelerated approach to up-titration of the conventional sequence , drug sequencing starting with an ARNI , rather than a RASi, and up-titrating all drugs rapidly, as in Sequence 1a , and the four new treatment sequences found to be most advantageous over the accelerated conventional sequence . In Sequences 25, the order in which the treatments of interest were used was varied from Sequence 1b. The principal scenario reported here assumes that each treatment exerted its full effect from halfway through the up-titration period .
Medication sequences and duration of up-titration periods: Sequences 1, 1a, 1b, 25, and duos 16. The colour boxes indicate different medications, i.e. pink for renin-angiotensin system inhibitor, orange for beta-blocker, green for mineralocorticoid receptor antagonist, red for angiotensin receptorneprilysin inhibitor, and blue for sodiumglucose cotransporter-2 inhibitor. ARNI, angiotensin receptorneprilysin inhibitor BB, beta-blocker MRA, mineralocorticoid receptor antagonist RASi, reninangiotensin system inhibitor SGLT2i, sodiumglucose cotransporter-2 inhibitor.
The results of applying each of the different treatment sequences on the two endpoints of interest are shown in and and the difference in numbers of events and event-free survival after 12 months in .
What Is The Ejection Fraction Formula
The ejection fraction formula equals the amount of blood pumped out of the ventricle with each contraction divided by the end-diastolic volume , the total amount of blood in the ventricle. To express as a percentage, you would multiply by 100. So, EF = x 100.
In other words, the ejection fraction is the percentage of blood pumped out of the ventricle after a contraction.
Recommended Reading: Aha Heart Failure Classification
How Does Ejection Fraction Affect Heart Failure Treatment
A variety of treatment options available have been scientifically shown to benefit people who have heart failure with reduced ejection fraction. These therapies including medications, lifestyle changes, and surgery can relieve symptoms, prevent complications, slow the worsening of heart failure, decrease hospitalizations, and perhaps prolong life.
Medications used in heart failure with reduced EF have not demonstrated the same benefits in heart failure with preserved EF. In clinical trials, its not clear which of the medications used for HFpEF are the most beneficial.
In practice, people with HFpEF are often prescribed the same medications as those used by people with HFrEF, although the scientific evidence for doing so is neutral. There are different options in HFpEF, depending on the reason for the heart failure. Be sure to discuss these treatments with your doctor.
Citation Doi & Article Data
Citation:DOI:Kelly TrinhRevisions:see full revision historySystem:
- Heart failure with reduced ejection fraction
- Heart failure due to systolic dysfunction
- Systolic heart failure
Heart failure with reduced ejection fraction is a type of heart failure due to left ventricular dysfunction classified by a left ventricular ejection fraction of 40% or less. Heart failure with reduced ejection fraction occurs when the left ventricle is unable to contract and effectively pump blood , thus decreasing cardiac output.
Recommended Reading: How To Tell If You’re Having A Heart Attack Female
Clinical Characteristics Of Hfmref
Proper characterization and phenotyping of HFmrEF is important because it might support treatment recommendations based on available data and inform the design of future interventional trials in HFmrEF by facilitating appropriate trial selection criteria. HFmrEF is often defined as intermediate because this classification makes intuitive sense, or as a milder form of HFrEF because of some distinct clinical and treatment response similarities to HFrEF. Both of these approaches are overly simplistic and ignore the extensive emerging research that characterizes HFmrEF in detail in relation to HFrEF and HFpEF. Figure provides a conceptual representation of HFmrEF in relation to HFrEF and HFpEF, and Figs , provide detailed characteristics from specific data sets.
Fig. 1: Phenotype, risk of cause-specific outcomes and effect of therapies in HFrEF, HFmrEF and HFpEF.
Previous research has also assessed the degree of neurohormonal activation across the EF spectrum, showing higher circulating neurohormone levels in patients with HFrEF than in those with HFmrEF or HFpEF,,. The higher neurohormonal activation in HFrEF might reflect the greater HF severity and be a marker of higher rates of cardiovascular events in patients with HFrEF than in patients with HFmrEF or HFpEF, as well as the observed efficacy of neurohormonal inhibition in patients with HFrEF, and potentially in those with HFmrEF, but not in patients with HFpEF ,,.
How Is Ejection Fraction Measured
Generally, your left ventricle is the one measured for ejection fraction. It does the heavy lifting in your body, pumping blood to almost all your major organs.
However, current research suggests that the right ventricle shouldnt be ignored when determining ejection fraction of the right heart.
An accurate left ventricle ejection fraction reading can be measured through a variety of imaging techniques. The most common ejection fraction testing measures include:
- Echocardiogram. An echocardiogram uses sound waves to take images of your heart. A 2012 research article suggests that 3-D images provide the best and most accurate readings.
- Cardiac MRI . A C-MRI is an image-based test that uses a magnetic field, radio waves, and a computer to create detailed images of the inside of your heart.
- Cardiac catheterization. In this procedure, your doctor inserts a hollow tube into a large blood vessel to monitor your heart function. During the catheterization, a coronary angiography is also performed. A dye is injected into the catheter. Then, an X-ray monitors the blood flowing throughout your heart.
- Cardiac nuclear medicine scan. Trace amounts of radioactive materials are injected into your bloodstream. Theyre then detected by cameras that produce images of your heart and its mechanisms.
- Cardiac CT scan. This X-ray procedure can give a representation of heart size and, with gated images, heart function.
- swelling in your ankles, legs, or abdomen
- exercise intolerance
Don’t Miss: Is 105 Heart Rate High
Impact Of Initiating Two Therapies Simultaneously
Lastly, we examined the impact of starting two therapies simultaneously, keeping the more rapid up-titration timeline for each drug , as shown in and .
Compared with Sequence 1b, the greatest incremental reduction in the composite of heart failure hospitalization or cardiovascular death was with the sequence starting with the combination of SGLT2i plus MRA, followed by an ARNI and then beta-blocker . These sequences were estimated to prevent 2122 events per 1000 patients treated over 12 months compared with Sequence 1b and 45 more events compared with the best accelerated-sequence described above, i.e. Sequence 2 .
For all-cause mortality, an MRA plus beta-blocker, followed by SGLT2i and then an ARNI was most effective . These sequences were estimated to prevent 7 deaths per 1000 patients treated over 12 months compared with Sequence 1b and prevent 2 more deaths compared with the best accelerated-sequence described above, i.e. Sequence 3 .
Of note, the sequence starting simultaneously with a beta-blocker plus ARNI, followed by SGLT2i and then an MRA, substantially shortened the theoretical total time to full titration of all treatments but was not particularly effective in further reducing the risk of either outcome.
The cumulative risk reduction with each sequence of therapies is shown graphically for the composite of heart failure hospitalization or cardiovascular death and all-cause mortality in .
