Heart Disease Can Have Long
Patients who receive a diagnosis of coronary heart disease are at higherrisk for cognitive decline later on, a new study shows.
The study, published Monday in the Journal of the American College of Cardiology, found that scores on cognitive tests including verbal memory and orientation of time dropped faster after patients received such a diagnosis than they did leading up to it.
This study adds to the increasing body of literature that showcases how the heart and brain work together, said Dr. Neelum T. Aggarwal, director of research for the Rush Heart Center for Women and a cognitive neurologist at its Cardiology Cognitive Clinic. She was not involved in the study.
We are now seeing more issues related to cognitive function from heart disease as more people are living longer, and also undergoing more heart procedures, and placed on medications, Aggarwal wrote in an email.
The authors of the study say previous research on the issuehas been a mixed bag, often focused on the role of conditions like strokes and sometimes showing a more rapid cognitive decline thereafter. But the new study found a longer-term impact on the brain, following up with stroke-free adults for a median of 12 years and looking at a subset who had been diagnosed with a heart attack or angina, a kind of chest pain resulting from decreased flow of blood to the heart.
Physical Activity And Diet
Lifestyle modifications play a crucial role in management of cardiovascular and neurological diseases. Physical activity and a well-balanced diet favor cardiovascular conditioning and improves performance and capacity. Exercise has a positive effect on the metabolism, which controls glucose levels, especially for stress-related pathology and brain disorders such as depression, which impose a heavy burden on the cardiovascular system. Many studies are currently being done for more information and knowledge regarding the common mediators for cardiovascular disease and the central nervous system. The brain-heart interaction is considered bidirectional, however the majority of times the central nervous system is regulated more over the heart and blood vessels.
Smoking And Cardiovascular Disease Risk
As well as causing cancer, smoking affects the arteries that supply blood to your heart and other parts of your body. It reduces the amount of oxygen in your blood and damages your artery walls.
Smoking increases your risk of heart attack, stroke and peripheral vascular disease â which can lead to gangrene and limb amputation).
Smoking makes your blood âstickierâ, causing blood cells to clump together. This slows blood flow through your arteries and makes blockages more common. Blockages may cause heart attack and stroke.
Smoking also makes your artery walls sticky, causing them to become clogged with fatty material called plaque or atheroma. Smokers often have cold hands or feet as a result of clogged arteries, which may also lead to serious problems such as gangrene.
If your coronary artery becomes clogged, it can cause angina. If a blood clot forms in the narrowed coronary artery and completely blocks the blood supply to a part of your heart, it can cause a heart attack.
Don’t Miss: Can Acid Reflux Cause Palpitations
Heart Disease And Stroke Risk Factors
There is no single cause for CVD, but there are risk factors that increase your chance of a heart attack or stroke. There are modifiable factors and non-modifiable factors .
Heart disease and stroke risk factors that you can change include:
- Management of depression.
Social isolation and lack of social support are risk factors for CVD that can be changed, although it can seem challenging. One way to help with loneliness is to learn how to improve your social connections.
Risk factors you canât change include increasing age, being male, being post-menopausal and having a family history of CVD. Aboriginal and Torres Strait Islander people are also at increased risk of CVD.
The good news is that you can reduce your overall risk of developing CVD by leading a healthy lifestyle and taking medicines as prescribed by your doctor.
How Can Vasculitis Affect The Nervous System
Vasculitis can cause problems in the central and peripheral nervous systems, where it affects the blood vessels that nourish the brain, spinal cord, and peripheral nerves. A vasculitis syndrome may begin suddenly or develop over time.
Vasculitis in the brain can lead to stroke:
- Cerebral aneurysms can burst and spill blood into surrounding tissue
- Blood in the inflamed blood vessel can clot , blocking blood flow and causing ischemic stroke
Additional nervous system symptoms include:
- Transient ischemic attack
- Headaches, especially a headache that doesnt go away
- Swelling of the brain
Recommended Reading: Reflux And Palpitations
Being Overweight And Cardiovascular Disease Risk
Being overweight or obese increases your risk of a number of health problems, including:
- CVD.
- Sleep problems, such as sleep apnoea.
- Certain types of cancer.
Carrying extra weight around your middle is more of a health risk, so it is especially important for you to lose weight if this is the case.
To achieve a healthy body weight, balance the energy coming into your body through food and drinks, with the energy being used up by your body through regular physical activity.
Family History And Cardiovascular Disease Risk
A personâs family history of disease can increase their tendency to develop:
- Diabetes.
- A particular body shape.
Although having a family history of CVD is a risk factor you canât change, it does not mean that you will develop it. However, if you do have a family history of CVD, it is important to reduce or remove other risk factors. For example, adopting healthy eating patterns, do not smoke, and lead an active, healthy lifestyle.
Don’t Miss: Does Tylenol Increase Heart Rate
When Your Heart Loses Its Rhythm
If those electrical bursts really get knocked off course, you feel it — your heart may start to race or beat slower than normal. That means your organs and muscles may not get enough oxygen — you could have chest pain and feel lightheaded, and you might even faint. If the rhythm gets totally out of whack, your heart gets like gelatin: It quivers and canât pump at all. This is called fibrillation, and it can be life-threatening.
What Research Is Being Done To Better Understand These Syndromes
The National Institute of Neurological Disorders and Stroke is the main funder of research on the brain and nervous system and a component of the National Institutes of Health , the leading biomedical research organization in the world. Other NIH institutes that support research on vasculitis include the National Heart, Lung, and Blood Institute and the National Institute of Arthritis and Musculoskeletal and Skin Diseases .
Several NINDS-funded investigators are studying blood vessel damage and cerebral blood flow as it relates to stroke. A better understanding of the mechanisms involved in injury and repair of blood vessels in the brain may lead to improvements in the treatment and prevention of other vascular disorders.
The Vasculitis Translational Research Program at NIAMS is dedicated to performing clinical and translational research in all types of vasculitis. Objectives of the program are to follow people with the disorder over time to see how it affects them and to discover new aspects of vasculitis that will help doctors learn how to better care for individuals with the disease.
More information about NIH-funded research on vasculitis and other disorders can be found using NIH RePORTER, a searchable database of current and past research projects supported by NIH and other federal agencies. RePORTER also includes links to publications and resources from these projects.
Also Check: Does Tylenol Increase Heart Rate
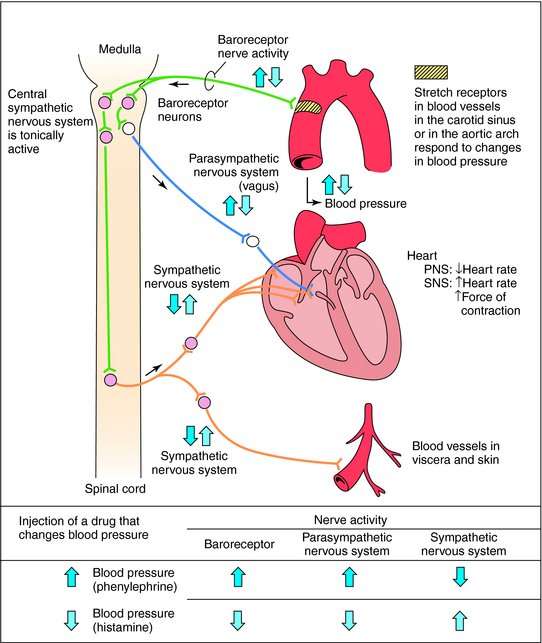
Baroreceptor Anatomy And Function
The baroreceptors are mechanoreceptors located in the carotid sinus and aortic arch that respond to beat-to-beat changes in SBP or pulse pressure. When activated by stretch, they transmit sensory signals to the vasomotor centre in the brain stem via the vagal nerve , the nerve of Hering and the glossopharyngeal nerve . This initiates an efferent reflex response, resulting in both sympathetic inhibition and parasympathetic activation . In hypertension the baroreceptor response to blood pressure resets, whereas in HF it is diminished. It is hypothesized that electrical stimulation of the carotid sinus nerve distal to the mechanoreceptor will circumvent such attenuation and intensify afferent input to the brain stem, thereby reflexively inducing augmented parasympathetic tone and attenuated sympathetic nerve firing.
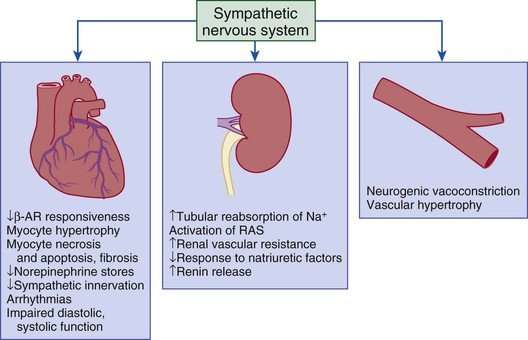
Renal Nerve Anatomy And Function
The kidneys are innervated by both efferent and afferent sympathetic nerves. Stimulation of the efferent nerves has been shown to increase renin secretion through the direct action of norepinephrine on β-adrenoreceptors on juxtaglomerular cells, to promote sodium and water reabsorption at the tubular level via activation of α-adrenoreceptors, and to reduce renal blood flow and glomerular filtration through vasoconstriction, all of which are important mechanisms in the pathophysiology of HF.
There are two main types of afferent nerves, both predominately found in the renal pelvis one is chemosensitive and responds to nociception and the other is mechanosensitive and responds to stretch. Activation of the afferent system stimulates CNS centres known to be involved in cardiovascular regulation. Conversely, interrupting the afferent nerves in diseased states reduces central sympathetic outflow, particularly to the heart, kidneys and peripheral vasculature.
The proximity of the nerves to the renal artery lumen make them amenable to destruction using transcatheter ablative techniques with radiofrequency or ultrasound energy or alcohol injection.
Also Check: How Much Can Marijuana Increase A Person’s Heart Rate
Overview Of Structural And Functional Organization Of The Cardiovascular Neuraxis
Autonomic control of the cardiovascular system is mediated through afferent and efferent pathways and neural networks involving the brain stem, spinal cord, peripheral ganglia, and ICNS . Feedback systems between each of these components exist and mediate transduction of beat-to-beat information, allowing for maintenance of hemostasis and adaptation to stressors . The cardiovascular neuraxis can be considered in three different levels: Level 1 is considered the heart with its own ICNS, which is comprised of cardiac ganglia that reside at the origin of the great vessels, and posteriorly along the atria and atrioventricular junction . Level 2 consists of intrathoracic components that regulate cardiac function including the middle cervical ganglia, cervicothoracic ganglia, and the T2-T4 portions of the sympathetic chain . Level 3 can be considered as the dorsal root and nodose ganglia, which mediates the majority of afferent neurotransmission, as well as spinal cord, brainstem, and higher centers . Importantly, information is processed at multiple levels by interneurons, resulting in the interdependent network interactions between brainstem, spinal, intrathoracic, and cardio-cardiac reflexes . While initially thought to exert opposing effects on cardiac electrophysiologic and mechanical properties, interactions between the sympathetic and parasympathetic nervous systems mediate cooperative control and regulation of function .
How Does Congestive Heart Failure Affect The Cardiovascular System
In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch to the point that the heart cant pump blood efficiently throughout your body. Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
Recommended Reading: Does Tylenol Increase Heart Rate
Cholesterol And Cardiovascular Disease Risk
Cholesterol is a fatty substance produced naturally by your body . It is used for many different things in your body but is a problem when thereâs too much of it in your blood.
High total cholesterol causes fatty material to gradually build up in your bodyâs arteries, making it harder for blood to flow through. It is mainly caused by eating foods high in saturated fats and trans fats.
Your total cholesterol includes two types of cholesterol, which are:
- Low-density lipoprotein â also known as âbadâ cholesterol because it can add to the build-up of plaque in your arteries and increase your risk of heart attack and stroke.
- High-density lipoprotein is also known as âgoodâ cholesterol because it helps to protect you against heart attack and stroke.
Most of the total cholesterol in your blood is made up of âbadâ LDL cholesterol. Only a small part is made up of âgoodâ HDL cholesterol.
You should aim for low LDL cholesterol and higher HDL cholesterol on advice from your doctor. If you are having trouble with your cholesterol levels, a dietitian can help you to eat healthily for your specific needs.
Perception Of Breathlessness In Heart Failure
Breathlessness is a normal experience after excessive physical exertion and is more pronounced in the physically deconditioned. It is also a cardinal symptom of CHF, in which several mechanisms probably contribute to its generation. Although counter-intuitive, there is little or no relationship between symptoms of CHF and objective indices of function The issue is of obvious clinical importance, with a spectrum of symptoms ranging from excessive, causing debility in patients with well-preserved organ function on the one hand, to lack of an important `early warning system’ in patients with significant pathology on the other. However, to date, the role of the CNS in generating such variability of symptom perception has not been studied directly. One of the motives to perform the present study was to address this. We attempted to identify if rCBF, in a particular cerebral area, co-varied with the subjective sensation of breathlessness in the CHF patients. No such area was identified. In fact there was less cerebral activation in the patients than in the controls, although both groups had similar subjective sensations of breathlessness. This subjective similarity may itself be considered rather surprising.
Also Check: How Accurate Is Fitbit Charge 2 Heart Rate
Analysis Of Pet Images
PET images were transformed into a standard stereotactic space. Regional blood flow measurements were corrected for global changes in blood flow and comparisons of rCBF across conditions were performed with the t statistic on a voxel by voxel basis by statistical parametric mapping software . rCBF changes related to the post-exercise breathlessness runs were compared with isocapnic hyperventilation runs as well as with baseline conditions. These analyses permitted the construction of statistical parametric maps for the description of significant changes in rCBF between the different test conditions. Significant changes were identified by applying a statistical threshold of 0.05, corrected for multiple comparisons.
For the computation of global cerebral blood flow , arterial blood was sampled throughout the scanning procedure from the radial arterial line. gCBF measurements were obtained by means of least squares fits of total tissue radioactivity using the Kety model.
Pharmacological Restoration Of Autonomic Nervous System Imbalance
In addition to devices and ablation strategies, a number of new pharmacological approaches targeting ANS dysfunction are being developed. The attenuation of the effects of neurally released and circulating norepinephrine on β-1 and β-2 adrenoreceptors is the most obvious established example in chronic HF and beta-blockers have had a class 1 indication for HFrEF for over 10âyears, which has been reinforced in the current 2016 ESC guidelines for chronic HF.
Stimulation of the parasympathetic branch of the ANS is more difficult to achieve pharmacologically. Parasympathetic innervation of the heart is mediated primarily by ACh binding to the M2 muscarinic ACh receptor . Although parasympathetic fibres are also found throughout the ventricles, the majority are located in the sinoatrial node, the atrial myocardium, the atrioventricular node, and the ventricular conducting system.
Pyridostigmine, a ChEI that does not cross the bloodâbrain barrier and thus only acts peripherally, increased HRV in healthy humans. Pyridostigmine increased HRV and reduced ventricular arrhythmias in HF patients.
Collectively, these findings indicate that ChEIs ameliorate the sympathoâvagal balance and improve haemodynamics in HF. An important caveat is that ChEI will also stimulate sympathetic cervical, splanchnic and lumbar ganglionic neurotransmission. Indeed, an increase in MSNA was reported after application of edrophonium, a short-acting ChEI.
Recommended Reading: Does Acid Reflux Cause Heart Palpitations
How Is Vasculitis Diagnosed In The Nervous System
Diagnosing vasculitis that affects the nervous system can be difficult, as some diseases have similar symptoms. Diagnosis depends on the number of blood vessels involved, their size, and their location as well as the types of other organs involved.
A doctor will review the persons medical history, perform a physical exam to confirm signs and symptoms, and order diagnostic tests and procedures, including:
- Blood and urine tests to look for signs of inflammation
- Analysis of the fluid that surrounds the brain and spinal cord to check for infection and signs of inflammation
- Biopsy of brain or nerve tissue
- Diagnostic imaging using computed tomography and magnetic resonance imaging to provide images of the brain, nerves and other organs, and tissues, and detect weakened or blocked vessels.
- Angiogram to detect the degree of narrowing of blood vessels in the brain, head, or neck
- Ultrasound to produce high-resolution images of the blood vessel walls and organs to look for inflammation
Blood Pressure And Cardiovascular Disease Risk
Blood pressure is the pressure of the blood in your arteries as it is pumped around your body by your heart. Blood pressure depends on two main things: the amount of blood pumped by your heart and how easily the blood can flow through your arteries.
Your blood pressure will go up and down throughout the day, depending on the time of day and what you are doing. However, high blood pressure is a condition where your blood pressure is consistently high.
Your family history, eating patterns, alcohol intake, weight and level of physical activity have a strong influence on blood pressure. In some people, medicines, including the oral contraceptive pill, contraceptive âdepotâ injections, steroids and arthritis medicines, can also raise blood pressure.
High blood pressure can overload your heart and arteries and speed up the artery-clogging process. This can lead to problems such as heart attack and stroke.
High blood pressure can also affect arteries to other parts of your body, such as the eyes, kidneys and legs.
If high blood pressure is not treated, your heart may weaken because of the constant extra demand. This may cause âheart failureâ, a serious condition with symptoms such as tiredness, shortness of breath and swelling of the feet and ankles.
Read Also: Why Do Av Nodal Cells Not Determine The Heart Rate
