Who Is The Stage B Pre
Stage B is composed of patients who have structural heart disease associated with risk of subsequent heart failure. By definition, the advancement from Stage A to Stage B heart failure can occur without recognition by patients especially if noncardiac factors limit physical activity. Thus, the clinical definition of the Stage B patient is often somewhat difficult to pinpoint. For example, the Mayo Clinic criteria include an assessment of physical activity .
STAGE B CLINICAL DEFINITIONS
STAGE B SYSTOLIC DYSFUNCTION
Stage B outcomes depend on the population studied and the criteria used to define structural heart disease. In patients with left ventricular systolic dysfunction , it is estimated that there are four times as many asymptomatic as symptomatic Stage C and D patients combined.4
The Framingham Study assessed 4257 asymptomatic participants and found an ejection fraction < 50% to be present in 6.0% of men and in 0.8% of women. As systolic function worsened, prognosis approached that of symptomatic systolic dysfunction .5
STAGE B SYSTOLIC AND DIASTOLIC DYSFUNCTION
The Mayo Clinic sampled a cross-section of 2029 Olmsted County, Minnesota residents aged 45 years. When using clinical criteria including post-MI, systolic dysfunction, valvular heart disease, and left ventricular hypertrophy either by ECG or on echocardiogram, they found a Stage B prevalence of 23%. When Doppler diastolic dysfunction was included, the prevalence increased to 34% .3
Congestive Heart Failure Treatment Options
Middle Georgia Heart is experienced in treating patients with CHF.
Our compassionate medical team takes a comprehensive approach to treating our patients, starting with performing numerous tests to make an accurate diagnosis. These diagnostic tests can include an electrocardiogram , echocardiogram, stress tests, and heart monitors.
Once our team diagnoses your heart condition, well create a treatment plan for you. These plans can vary based on your needs, ranging from small lifestyle changes to procedures performed by our doctors.
What Is Heart Failure
Heart failure, or congestive heart failure, is a long-term condition that gets worse over time. Although the name sounds like your heart has stopped working, heart failure means your heart isnt able to pump blood as well as it should. When your heart has less pumping power, that can damage your organs and fluid can collect in your lungs.
Also Check: How Long Can A Heart Attack Last Before Death
C History Part : Competing Diagnoses That Can Mimic Stage B Heart Failure
Stage B HF can be readily distinguished from other stages along the HF spectrum by history, physical exam, and imaging.
Stage A HF, which represents risk factors for HF in the absence of cardiac structural or functional changes, can be differentiated by history and imaging .
Stage C HF is differentiated from stage B HF if symptoms or signs of HF are present, or if the patient has a prior history of symptomatic HF.
Figure 1 Heart Failure Stages And Classes
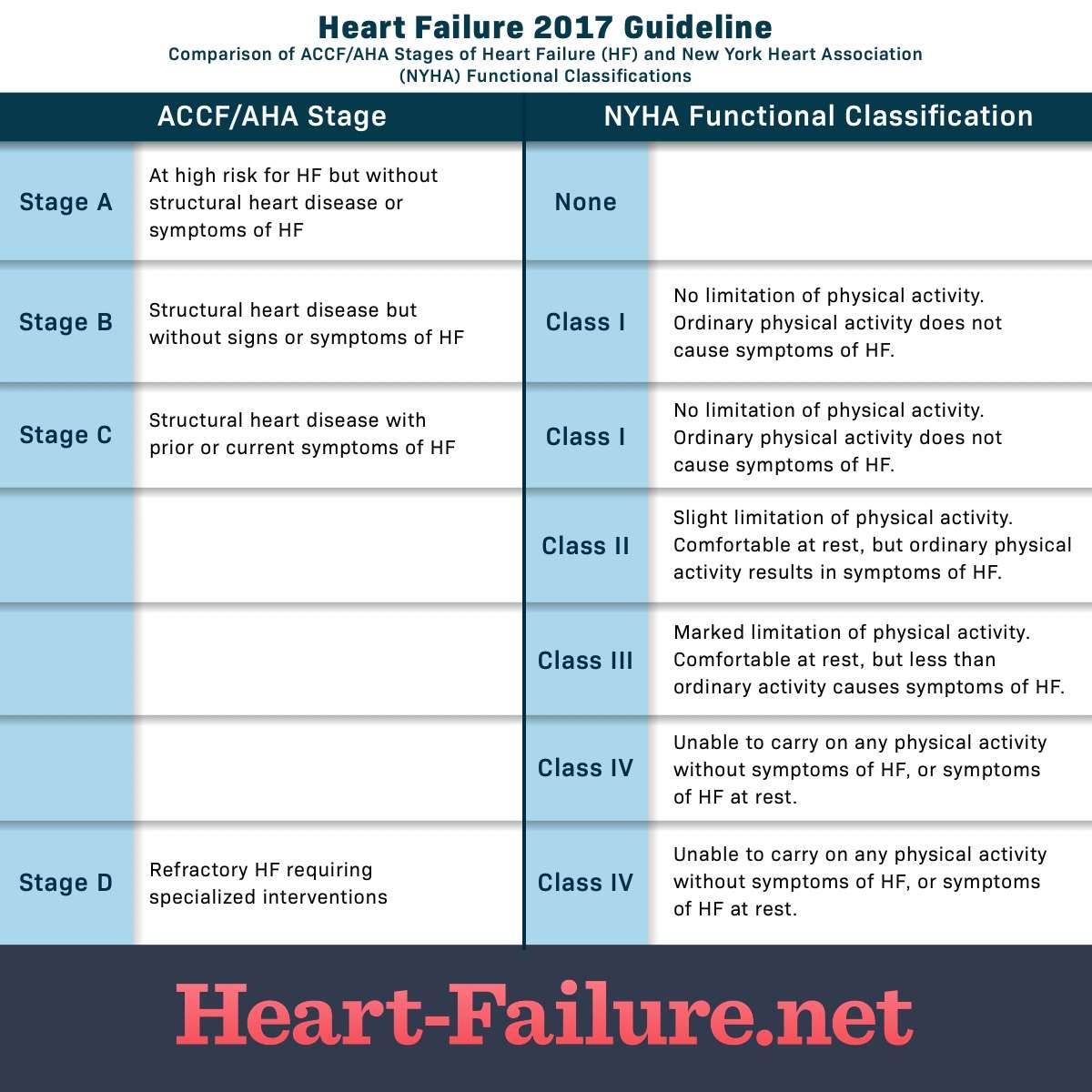
The stages above describe the range from a high risk of developing heart failure on through advanced heart failure. The stages are correlated to treatment plans. The stages are also progressive, as HF worsens, you advance to the next stage of heart failure. There is no reversal through the stages. The objective is that with treatment, progression through the stages may be delayed.4
Read Also: Treatments Of Congestive Heart Failure
Definition Of Hf Stages
HF stages were defined according to the American College of Cardiology/American Heart Association definition:
-
HF stage A: patients with risk factors of HF, with normal echocardiography and without signs or symptoms of HF.
-
HF stage B: patients with risk factors of HF, with an abnormal echocardiography but without past or current symptoms of HF.
-
HF stage C: patients with an abnormal echocardiography and past or current symptoms of HF.
To ensure the HF diagnoses in patients categorised as HF stage C, we used the European Society of Cardiology definition of HF. Signs of HF may be absent, for which reason a biochemical confirmation of HF was included. Patients in HF stage C needed to fulfil three criteria: symptoms of HF abnormal echocardiography according to study definition and clinical signs and/or abnormal plasma concentrations of NT-proBNP .
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Don’t Miss: How To Decrease Resting Heart Rate
New Treatments And Future Perspectives
While the effects of sodiumglucose cotransporter 2 inhibitors on atrial function have not been assessed, to date,104, 129, 130, 131 new drugs acting directly on cardiac function may have an impact also on the LA. Compared with placebo, the myosin activator omecamtiv mecarbil improved LA function, as shown by a reduced LA minimal volume and a larger emptying fraction, in the Chronic Oral Study of Myosin Activation to Increase Contractility in HF trial and reduced the risk of newonset AF and stroke, likely through an improvement in LA function, in the larger Global Approach to Lowering Adverse Cardiac outcomes Through Improving Contractility in HF trial.132, 133, 134, 135
Rhythm control for AF may improve LA function and this may improve patients’ outcomes.130 These effects, shown also after pulmonary vein isolation, may be particularly effective in patients with HFpEF such as 79% of the patients analysed in the Catheter Ablation versus Antiarrhythmic Drug Therapy for Atrial Fibrillation trial.136 Improvement in LA function, as well as in outcomes, has been shown also in the Catheter Ablation versus Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation trial, enrolling patients with reduced LVEF.137
Prognosis By Ejection Fraction
Ejection fraction is a measure of how much blood is pumped out of your heart each time it contracts. A healthy heart has an EF of between about 55 percent to 75 percent.
Some people with CHF have a reduced EF. This means their heart is pumping less blood out to the rest of their body than a healthy heart. Studies have shown that people who have CHF and a reduced EF have a more challenging outlook than people with CHF who do not have a reduced EF.
The exact survival rates varied among studies, but have shown that EF has an impact on prognosis. Your doctor will have the best information about how your ejection fraction can affect your prognosis.
Also Check: Heart Shaped Lips Surgery
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
E Common Pitfalls And Side
In patients who are intolerant of ACE-inhibitors , angiotensin receptor blockers should be used.
In patients with normal or low blood pressure, carvedilol may not be tolerated. In these patients, we typically use long-acting metoprolol .
Digoxin should not be used in patients with stage B HF unless there is a separate indication for its use .
In patients on spironolactone who develop gynecomastia or breast tenderness, eplerenone can be used.
In patients with LV systolic dysfunction, calcium channel blockers, particularly non-dihydropyridine calcium channel blockers should be avoided. We typically avoid dihydropyridine calcium channel blockers in these patients as well unless there is a specific indication for their use.
ACE-inhibitors:
-
Ramipril 1.25 to 2.5mg orally every day, up to 10mg orally every day
-
Lisinopril 2.5mg orally every day, up to 20 to 40mg orally every day
-
Enalapril 2.5mg orally twice a day, up to 20mg orally twice a day
-
Captopril 6.25mg orally three times a day, up to 50mg orally three times a day
Angiotensin receptor blockers:
-
Losartan 25 to 50mg orally every day, up to 100mg orally every day
-
Candesartan 4 to 8mg orally every day, up to 32mg orally every day
-
Valsartan 20 to 40mg orally twice a day, up to 160mg orally twice a day
Aldosterone antagonists:
-
Spironolactone 12.5 to 25mg orally every day, up to 25mg orally twice a day
-
Eplerenone 25mg orally every day, up to 50mg orally every day
Beta-blockers
Recommended Reading: What Should Your Heart Rate Be When Sleeping
Stages Of Heart Failure
In line with the 2021 HF Society of America, HF Association of the ESC and Japanese HF Society universal definition of HF,52 a fourstage classification has been proposed for atrial disease. We discuss below the potential benefits of prevention and treatment on LA reverse remodelling, across the four HF stages.
Echocardiographic Characteristics Of Hf Stages
Echocardiographic parameters were used to identify patients in both HF stages B and C. In this study comparable prevalence of structural and functional abnormalities of the myocardium was found in HF stages B and C, and only LV mass index and e septal differed between HF stages B and C. Other studies have observed a more pronounced difference in echocardiographic variables, increasingly so with higher stages of HF.
Also Check: How Long Can You Have Angina Before A Heart Attack
What You Can Do
Some risk factors of heart failure, like age, cant be modified. Still, people with CHF can take steps to improve the long-term prognosis. The first thing to do is to be familiar with any family history of heart disease. You’ll also want to learn about all the possible symptoms. Don’t ignore any symptom that you think is cause for concern. Tell your healthcare provider about them right away.
Regular exercise, along with managing any other health issues you may have, can also help to keep CHF under control.
Heart Failure Symptoms By Class And Stage
- Bookmark for later
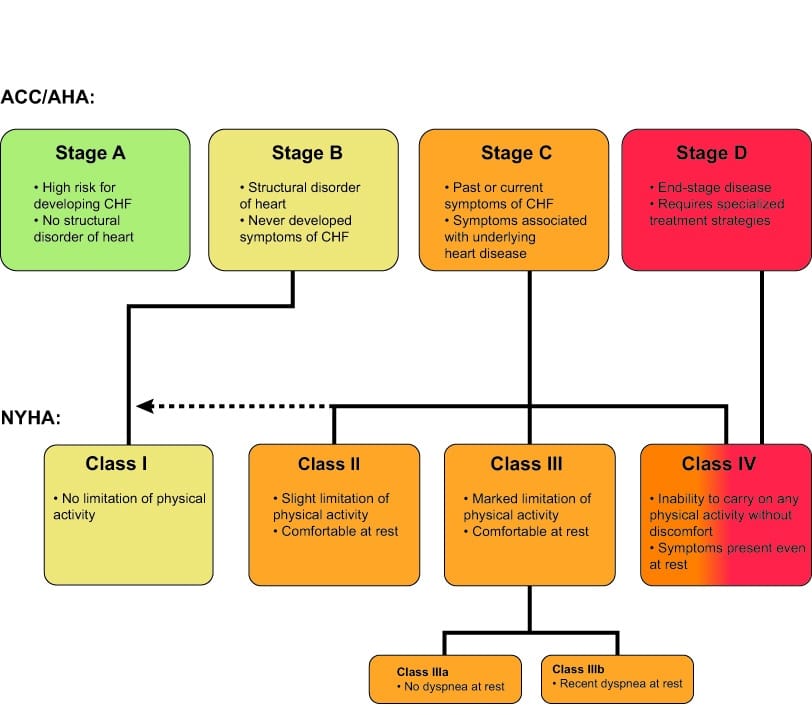
Heart failure is a complex, chronic syndrome that gets worse over time. During the diagnostic process, physicians classify each case of heart failure. The American College of Cardiology/American Heart Association and the New York Heart Association have complementary classification systems.1-4
The ACC/AHA stages reflect the range from a high risk of developing heart failure to advanced heart failure and are associated with an approach to treatment plans.1-4 The New York Heart Association clinical classifications of heart failure reflect the severity of symptoms or functional limits due to heart failure.1-2 A diagnosis can have an assignment of a stage and a class.
Recommended Reading: What Are The Early Signs Of Congestive Heart Failure
American College Of Cardiology/american Heart Association Classification
The American College of Cardiology/American Heart Association classification of heart failure stages focus more on the condition’s structural impact on the heart, such as the measurement of ejection fraction:
- Stage A: You do not have any structural disorder of the heart, but are at high risk for developing congestive heart failure due to a family history of heart failure or a personal history of hypertension, diabetes, coronary artery disease, alcohol abuse, viral infections, or use of drugs that are toxic to the heart.
- Stage B: You have a structural disorder of the heart, but no symptoms of heart failure .
- Stage C: You have a structural disorder of the heart and you have currently or previously displayed symptoms of heart failure.
- Stage D: People in this final stage of heart failure do not get better with treatment.
Diagnosis Congestive Heart Failure
The diagnosis of congestive heart failure is predominantly by history and physical, though echocardiography and cardiac catheterization can be beneficial.
Physical examination during systolic congestive HF will reveal a S3 heart sound if significant left ventricular dilation is present. A S4 heart sound can be present in diastolic HF. The point of maximal impulse, or PMI, will be laterally displaced and, at times, the S3 can even be palpable. Cardiac murmurs will be present if valvular heart disease is present, contributing to the HF such as aortic stenosis or mitral regurgitation.
Physical examination in states of right heart failure may reveal elevated jugular venous pressure including hepatojugular reflux, lower extremity pitting edema and ascites. Pleural effusions may be present and more prominent on the right compared to the left.
Echocardiography is indicated in all patients with a new diagnosis of congestive HF to help determine the etiology. The LV systolic function can be measured, including ejection fraction. Diastolic function assessment can help determine the left heart pressures. The cardiac valves can be interrogated for significant regurgitant or stenotic lesions.
Recommended Reading: What Causes Afib After Heart Surgery
B History Part : Prevalence:
The earlier the stage of HF, the higher the prevalence. Thus, stage B HF is more common than stage C, but not nearly as common as stage A which is defined as the presence of risk factors for heart failure in the absence of cardiac structural or functional abnormalities.
In a community study of approximately 2,000 participants, nearly 5% of individuals had evidence of LV systolic dysfunction and 21% had any grade of diastolic dysfunction without evidence of HF . During a follow-up period of 6 years, the risk for developing HF was nearly 25% in those with at least moderate diastolic dysfunction.
The burden of systolic dysfunction is also high. The total number of patients with asymptomatic LV systolic dysfunction is estimated to be three to four times as prevalent as the sum of all patients in stages C and D systolic HF. Figure 1 displays the increased risk of developing HF in patients with LV systolic dysfunction and in those with LV diastolic dysfunction.
Figure 1:
A) Kaplan-Meier curves for survival free of heart failure according to ejection fraction. B) Incidence of heart failure according to diastolic function.
In the Framingham Heart Study, the prevalence of LV hypertrophy was 17.5%. Several studies, including the Multi-Ethnic Study of Atherosclerosis, have found a strong association between increased LV mass and the development of symptomatic HF.
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Also Check: What Do Beta Blockers Do To Heart Rate
Take Care Of Your Mental Health Too
While stress is never pleasant, it can be especially hard on your heart. Anger management is also an important aspect of heart health.
Talking with a therapist or joining a support group can help with keeping your stress levels down and giving you accountability for the lifestyle changes youre making.
Iv Management With Comorbidities
Hypertension: in patients with stage B HF who have concomitant hypertension, we typically use ACE-inhibitors , carvedilol, chlorthalidone, spironolactone, and amlodipine as agents which are efficacious in controlling blood pressure, improve outcomes, and/or are associated with improvements in cardiac structure and function.
Diabetes: ACE-inhibitors and angiotensin receptor blockers are beneficial in patients with diabetes because of their renal protective effects. These agents can also decrease the incidence of diabetes and proteinuria in patients with LV dysfunction and impaired glucose tolerance. Carvedilol has less of a detrimental effect on glucose control in diabetics compared to short-acting metoprolol. Spironolactone can cause an increase in hemoglobin A1c levels, whereas eplerenone does not.
Chronic kidney disease: electrolytes and renal function should be monitored frequently since many patients with stage B HF will be on ACE-inhibitors or angiotensin receptor blockers.
ACE-inhibitors, angiotensin receptor blockers, and aldosterone antagonists should not be prescribed to patients with hyperkalemia. In addition, potassium and renal function should be checked 7 to 10 days after starting or uptitrating any of these drugs.
Pregnant patients should not be prescribed ACE-inhibitors or angiotensin receptor blockers.
You May Like: Why Does Alcohol Increase Heart Rate
