Palliative Care For Patients With Heart Failure
- A
- A
Palliative care, sometimes now referred to as supportive care, is specialized care that focuses on improving quality of life through relief of stress and symptoms for patients with serious illness.1 While most often associated with oncology, palliative care is appropriate for any patient in the advanced stages of illness, including patients with heart failure . HF patients not only suffer from dyspnea and fatigue as a result of their disease process, but also have a high burden of somatic complaints, including pain, nausea, anxiety, and depression, leading to significant psychosocial distress for both patients and their caregivers.2,3 Advance care planning and complex shared decision making become increasingly important as HF progresses, particularly when patients are faced with options such as transplant and mechanical circulatory support, which may not align well with their overall goals or preferences. Because of the unique role palliative care has in the management of all of these domains, several recent consensus statements and care guidelines have recommended the incorporation of palliative care into the care of patients with advanced HF.4-8
Table 1: Differences Between the Traditional Model of Palliative Care That Was Developed for Oncology Patients vs. the Optimal Model of Palliative Care for Patients With Advanced Heart Failure
Table 2: Indication for Referral to Palliative Care for Patients With Heart Failure
|
Symptoms
Caregiver distress |
What Are The Symptoms
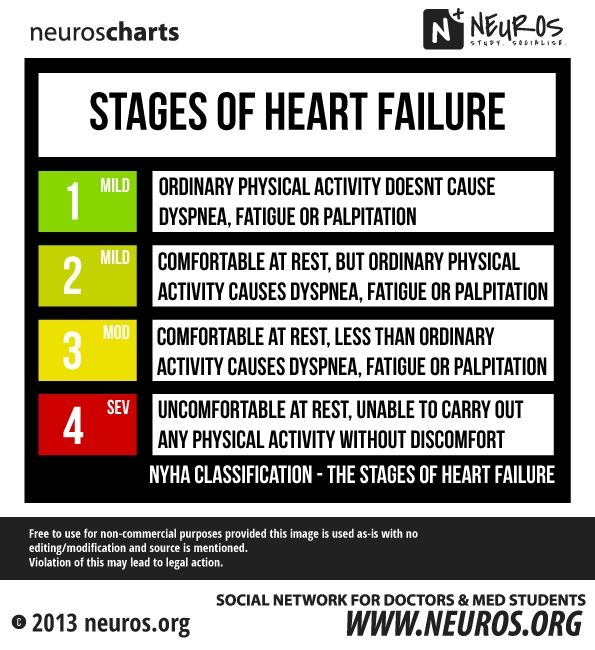
Some are easy to confuse with normal aging or other diseases. The more advanced your heart failure, the more likely you are to have many symptoms, or the changes that youâve noticed in yourself will worsen.
These are common ways that heart failure can affect you:
Shortness of breath. Heart failure can make it hard to breathe when you walk up a flight of stairs. With advanced heart failure, you may get winded in a shorter period of time, or you may have trouble even when youâre sitting still.
Sleep problems. Heart failure can make it hard to breathe or catch your breath when you lie in bed. You may have trouble nodding off to sleep, or you might wake up in the middle of the night gasping for air. Try sleeping while propped up on two or more pillows instead of lying flat. Advanced heart failure makes it even more likely youâll have trouble breathing when youâre at rest. That means your bedtime problems will probably get worse, too.
Coughing. You may already have a dry cough that acts up when youâre lying in bed. You might cough often during the day, and your phlegm could have a slight pink tint to it. That means thereâs a bit of blood in the gunk youâre coughing up. Advanced heart failure can make that cough worse, especially when youâre lying down.
Fatigue. Heart failure can make you feel worn out. Things that wouldnât have tired you out in the past suddenly do. Youâre more likely to feel tired all of the time with advanced heart failure.
Show Sources
Critical Points For The Practising Cardiologist To Consider In Their Patients With End
Prof. Michael Weis
Average survival for end-stage chronic heart failure patients is less than one year. Timely referral of eligible patients to an advanced heart failure centre providing structural support, to extend quality of life, and to improve functional status, is recommended. Advances in transplantation, improved mechanical assist devices, and novel, multidisciplinary and palliative approaches contribute substantially to better care. Palliative care in ESHF includes focusing on symptom relief, emotional support and communication between the patient and her/his family. Recent technological advances have led to increased complexity of care and decision making at the end of life. As a result, advanced care planning for patients with ESHF must be addressed earlier in the course of the disease.
Recommended Reading: What Is A Heart Attack Definition
Stage C Treatment Options
Treatment at this stage focuses on managing your symptoms, optimizing your heart function, and preventing worsening of your condition.
Medications to treat stage C heart failure include:
- Diuretics to reduce fluid retention
- Digoxin to help the heart beat stronger and more regularly
- Beta blockers to help your heart beat stronger
- Entresto , which reduces the risk of death and hospitalization among patients with chronic heart failure
- SGLT2 inhibitors to help lower blood sugar
- Vasodilators, which are medications that help improve the flow of blood through your vessels
- Angiotensin-converting enzyme inhibitors
- Possible cardiac resynchronization therapy
- Possible implantable cardiac defibrillator therapy
In addition to the lifestyle changes for stages A and B, you may need to make the following changes:
- Reduce your sodium intake
- Restrict fluid intake
- Keep track of your weight daily
Remember that even if the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression of your condition to stage D.
When To Seek Hospice Care
Even physicians have difficulty determining life expectancy for people with end-stage heart-failure. The condition can be unpredictable, and symptoms can change. However, certain signs can indicate that hospice care would be beneficial, including:
- frequent chest pain
- significant fatigue or shortness of breath
- substantial decline in ability to do daily activities, such as self-care
- The patient has already received the best possible treatment, which are no longer working well, and the patient is not a candidate for other interventions.
- The patient has received the best possible treatment and has decided to decline further specialized interventions.
People can be reluctant to start hospice, as they may worry it means theyre giving up or that it will hasten death. But such concerns are unfounded. In fact, patients and families often wish they had started hospice sooner, because it makes such a positive difference in their lives. And research shows that early admission to hospice results in greater satisfaction with care among patients and family caregivers.
Don’t Miss: Can Dehydration Cause Increased Heart Rate
Support Them To Make Decisions About Treatments
As well as having an advance care plan, patients should be given the chance to discuss the following issues:
- Whether to deactivate an implantable cardioverter defibrillator , if they have one. This can prevent the ICD activating at the end of life, which can be distressing.
- What the patient would want to happen if they had a cardiac arrest. They may decide they do not want to have cardiopulmonary resuscitation .
- When to stop medication that no longer reduces symptoms or improves their quality of life. This can be a difficult conversation and it’s best carried out sooner rather than later. Make sure the patient and the people important to them understand what changes are being made to their medication and why.
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Recommended Reading: What Are Some Signs Of A Heart Attack
What Can Hospice Do For The Family Of A Person With Heart Disease
Family members may have to make difficult healthcare and financial decisions, act as caregivers and provide emotional support to others. If the decision is made to stop medical support, some families experience strong emotions and feel overwhelmed.
Hospice offers comprehensive services for families of patients with heart disease:
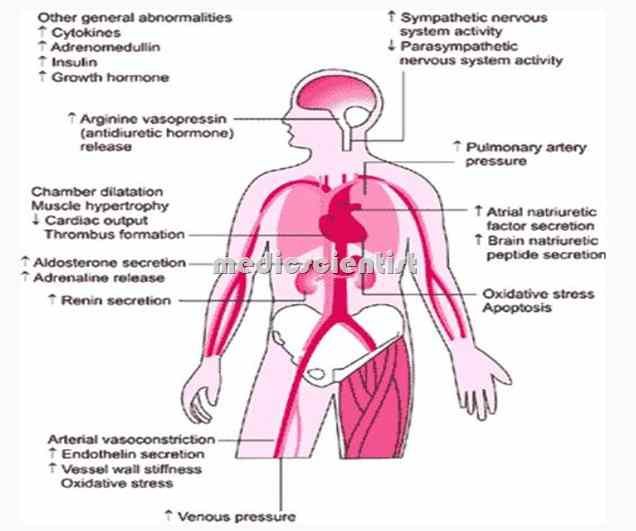
What Is Heart Failure
Heart failure, or congestive heart failure, is a long-term condition that gets worse over time. Although the name sounds like your heart has stopped working, heart failure means your heart isnt able to pump blood as well as it should. When your heart has less pumping power, that can damage your organs and fluid can collect in your lungs.
Recommended Reading: Can You Cure Congestive Heart Failure
Caring For Someone With Heart Failure Towards The End Of Life
Please be aware – this information is for healthcare professionals.
You can use our My Learning form to reflect on how this page has helped with your continuing professional development.
If you’re a patient, or a family member or friend, you can find more information on heart failure from the British Heart Foundation .
Heart failure means the heart is not pumping blood around the body as well as it should. People with heart failure may have symptoms such as fatigue, breathlessness and oedema . Here, we’ll talk about knowing when a patient with heart failure is near the end of life, and how to support them.
This information is about supporting adults with advanced heart failure.
On this page:
Pharmacological Management Of End Stage Heart Failure
Table 1Pharmacological management of end stage heart failure1,2,3,4,5
| Goal 1: Improvement of morbidity and mortality |
| ACE inhibitors |
| ARBs |
| Selected blockers |
| Goal 2: Control of symptoms |
| Diuretics |
| Digitalis |
ACE, angiotensinconverting enzyme ARBs, angiotensin II type I receptor blockers.
Table 2Overview of the drugs used for the pharmacological management of end stage heart failure1,2,3,4,5
| Drug class | |
|---|---|
| Cough, hyperkalaemia, renal insufficiency, angioedema | |
| Enalapril | |
| Blockade of theangiotensin II type Ireceptor | Losartan |
| Blockade of the 1adrenergic receptor | Metoprolol succinate |
| Blockade of the aldosterone receptor | Spironolactone |
| Blockade of the Na+/Cl cotransporter | Hydrochlorothiazide |
| Blockade of the Na+/2Cl/K+ cotransporter | Furosemide |
| Blockade of theNa+/K+ ATPase | Digoxin |
As patients with end stage heart failure frequently show signs of fluid retention or have a history of such, inhibitors of the reninangiotensin system should be coadministered with diuretics, which usually leads to rapid symptomatic improvement of dyspnoea and exercise tolerance while lacking significant effects on survival. End stage heart failure usually requires the use of loop diuretics, which may be effectively used in combination with thiazides in case of treatment refractory fluid overload due to a synergistic mechanism of action .
Also Check: How Do They Do Open Heart Surgery
Supporting Those Around The Patient
Those close to the patient may also need emotional and practical support. They may need:
- information about heart failure to help them understand the symptoms and treatment options
- support if they’re caring for the patient
- time to relax or look after their own health.
If the patient’s heart failure is due to an inherited heart condition, their family may have concerns about their own health. Talk to them about their worries. It might be appropriate to refer immediate family members to a clinic which specialises in inherited heart conditions. This may have been done when the patient was first diagnosed.
Inherited heart conditions services offer specialist assessment and investigations, genetic counselling and testing. GPs can refer to this service.
What Are The Symptoms Of End
Heart Failure: Quick Facts
1. More than 6 million U.S. adults have heart failure.
2. About half of people who develop heart failure die within 5 years of diagnosis.
3. Most people with end-stage heart failure have a life expectancy of less than 1 year.
4. The leading causes of heart failure are diseases that damage the heart, such as heart disease, high blood pressure, and diabetes.
Heart failure worsens over time, so symptoms are most severe during the final stages. It causes fluid to build up in the body, which produces many of these symptoms:
- Shortness of breath . In the final stages of heart failure, people feel breathless both during activity and at rest.
- Persistent coughing or wheezing. This may produce white or pink mucus. The cough may be worse at night or when lying down.
- Weight gain or swelling of the feet, ankles, legs, abdomen, or neck veins.
- Tiredness, weakness.
In addition, people in the final stages of heart failure may suffer from:
- depression, fear, insomnia, and isolation
- anxiety about their future
- trouble navigating the health care system
Recommended Reading: Dos And Don’ts After Heart Surgery
Hospice For Heart Disease & End
If you are reading this, it is likely you or someone you love has been waging a difficult physical and emotional battle against heart failure or some form of heart disease. Your search for comfort, support and answers does not stop when you accept that you must learn to live with heart disease. Thats when VITAS can help.
Hospice helps patients and their families deal with the significant impact of heart disease after curative treatment has stopped. On this page, we’ve provided answers to these questions:
- When is the right time to ask about hospice?
- What can hospice do for a person with heart disease?
- What can hospice do for the family of a person with heart disease?
- What are the overall benefits of hospice care?
- How can I approach my hospice discussion with family members and loved ones?
What Is An Ejection Fraction
An ejection fraction is a measurement of the blood pumped out of your heart with each beat, expressed in a percentage. It can be measured using an echocardiogram , multigated acquisition scan, nuclear stress test, magnetic resonance imaging , or during a cardiac catheterization. A normal ejection fraction is between 55% and 70%.
People at this stage may have some slight symptoms like:
- Slight physical limitations
- Shortness of breath with physical activity
Also Check: Congestive Heart Failure Chf
What You Can Do For Your Loved One
In addition to symptom management, its important for the family caregiver to learn how to recognize the end-of-life signs for CHF, and when they should contact hospice. Hospice care will be able to address the specific needs of CHF patients in their final days, and help them to get the most out of what time they have left.
Spell Out Your Choices
Itâs smart to let it be known ahead of time what you want to do if your symptoms worsen. Should the doctor try to extend your life at all costs, even if the treatment is painful? Or is your comfort level more important? You probably wonât be able to speak when you need a treatment like CPR, so making formal choices ahead of time can be worthwhile.
The doctor can help you decide if you want to have any of these things done to extend your life:
- CPR if your heart stops
- A breathing tube if you canât breathe on your own
- A feeding tube if you canât eat on your own
You may want the doctor to do everything in their power to keep you alive. Or you might have certain standards for quality of life youâd rather meet. You can write those choices down in a formal document called an âadvance directive.â Make sure your doctor and family members know your wishes.
Show Sources
American Heart Association: âAdvanced Heart Failure,â âPlanning Ahead: Advanced Heart Failure,â âRecognizing Advanced Heart Failure and Knowing Your Options.â
Circulation: âPalliative Care in the Treatment of Advanced Heart Failure.â
Heart: âManagement of end stage heart failure.â
American Family Physician: âDiuretics for Treatment of Patients with Heart Failure?â
Also Check: What Causes Heart Attack In Women
What Is The Outlook With Heart Failure
With the right care, congestive heart failure wont stop you from doing the things you enjoy. Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with heart failure have a life span 10 years shorter than those who dont have heart failure. Another study showed that the survival rates of people with chronic heart failure were 80% to 90% for one year, but that dropped to 50% to 60% for year five and down to 30% for 10 years.
A different study found that people who had heart failure and were discharged from the hospital had expected life spans ranging from three to 20 years, depending on various factors like age and gender. Its important to look at your specific situation when considering your prognosis.
Symptoms Of Heart Failure
Common symptoms of heart failure include:
- breathlessness either when resting or being active
- swelling of legs, ankles, feet, abdomen or around the lower back area
Patients with heart failure may find it difficult to move around, do daily activities, work and do hobbies. This can affect how they feel, and lead to worries about money or losing their independence.
If someone has symptoms of heart failure and they have not been diagnosed with heart failure, it’s important that they speak to their GP or another healthcare professional.
Don’t Miss: Atrial Fibrillation Heart Failure
