What Is A Heart Attack
A heart attack occurs when a blocked artery prevents oxygen-rich blood from reaching a section of the heart. If the blocked artery is not reopened quickly, the part of the heart normally nourished by that artery begins to die. The longer a person goes without treatment, the greater the damage.
Symptoms of a heart attack may be immediate and intense. More often, though, symptoms start slowly and persist for hours, days or weeks before a heart attack. Unlike with sudden cardiac arrest, the heart usually does not stop beating during a heart attack. The heart attack symptoms in women can be different than men.
What Are The Risk Factors Of Sudden Cardiac Arrest
Many factors can increase your risk of sudden cardiac arrest and sudden cardiac death.
The two leading risk factors include:
- Previous heart attack: Your risk of sudden cardiac death is higher during the first six months after a heart attack. Healthcare providers link 75% of sudden cardiac deaths to a previous heart attack.
- Coronary artery disease: Risk factors for coronary artery disease include smoking, family history of cardiovascular disease, high cholesterol or an enlarged heart. Theres a link between 80% of sudden cardiac deaths and coronary artery disease.
Other risk factors include:
What Is The Difference Between Sudden Arrhythmic Death Syndrome And Sudden Cardiac Death
When reading about sudden cardiac death, you might also come across the term sudden arrhythmic death . The difference between the two is that sudden arrhythmic death is diagnosed when the cause of the cardiac arrest can’t be explained in a post-mortem examination because the structure of the heart appears normal. Sudden arrhythmic death syndrome affects around 500 people in the UK every year. It is classified as a form of sudden cardiac death.
In the majority of cases, in sudden cardiac death the cause of cardiac arrest can be found in a post-mortem because something is wrong with the structure of the heart. The most common causes are damage to the heart muscle or abnormal heart rhythms due to heart attack or other coronary artery disease.
One of the reasons why the cause of death might not be found is down to the way the heart beats. The British Heart Foundation explains that the rhythm of your heart is controlled by electrical impulses. However, if the electrical impulses go wrong, it can cause an abnormal heart rhythm. This is known as an arrhythmia and can mean the heart is beating too quickly, too slowly, or irregularly.
If left untreated, an arrhythmia can cause a cardiac arrest. Your heart’s rhythm and electrical impulses are no longer there once you die therefore, an abnormal heart rhythm can’t be found and the heart’s structure will appear normal.
In about one in every 25 cases of sudden cardiac death, no definite cause of death can be found.
Also Check: How Does Heart Attack Affect The Organ System
Stages Of Dying From Congestive Heart Failure
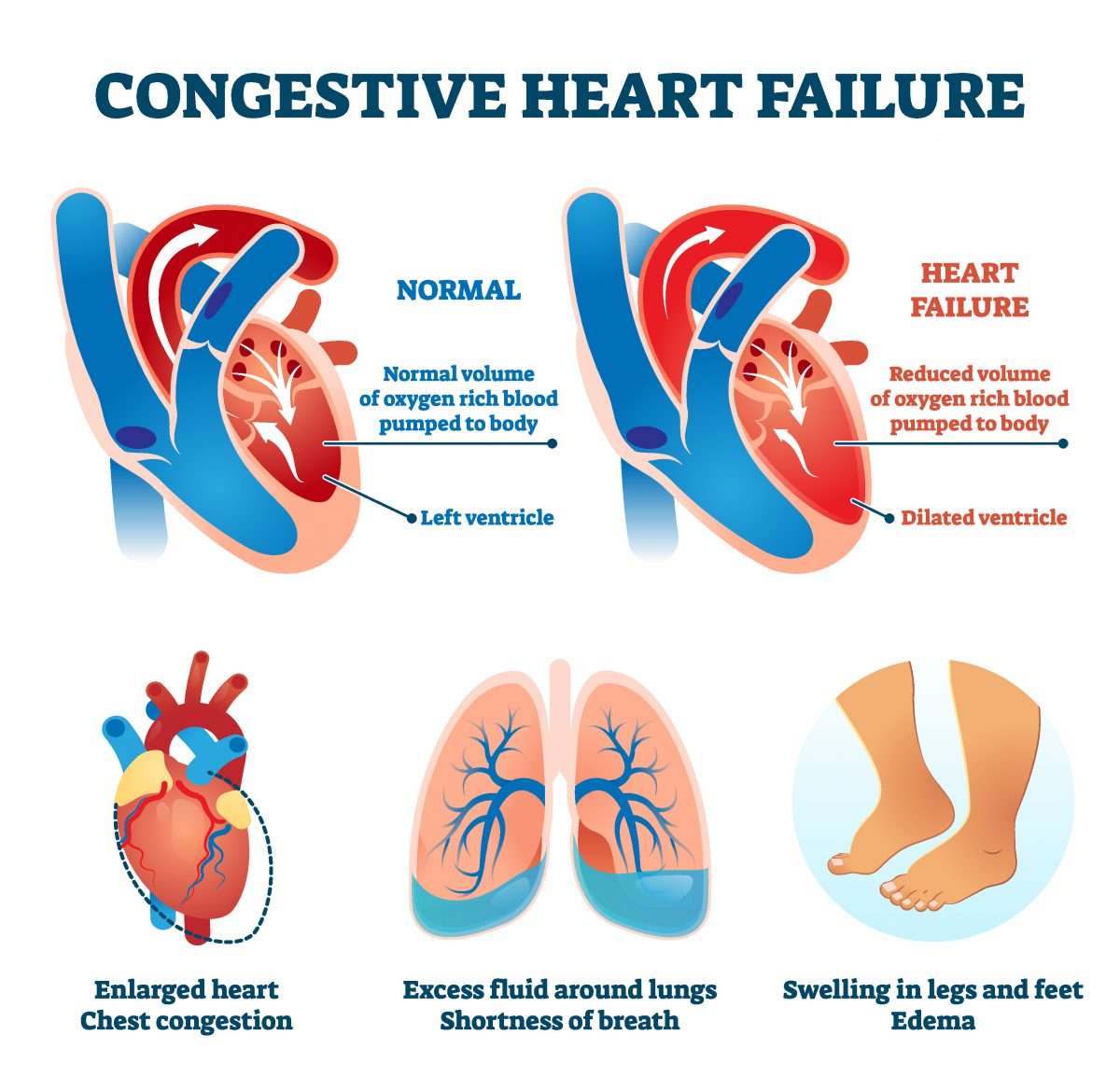
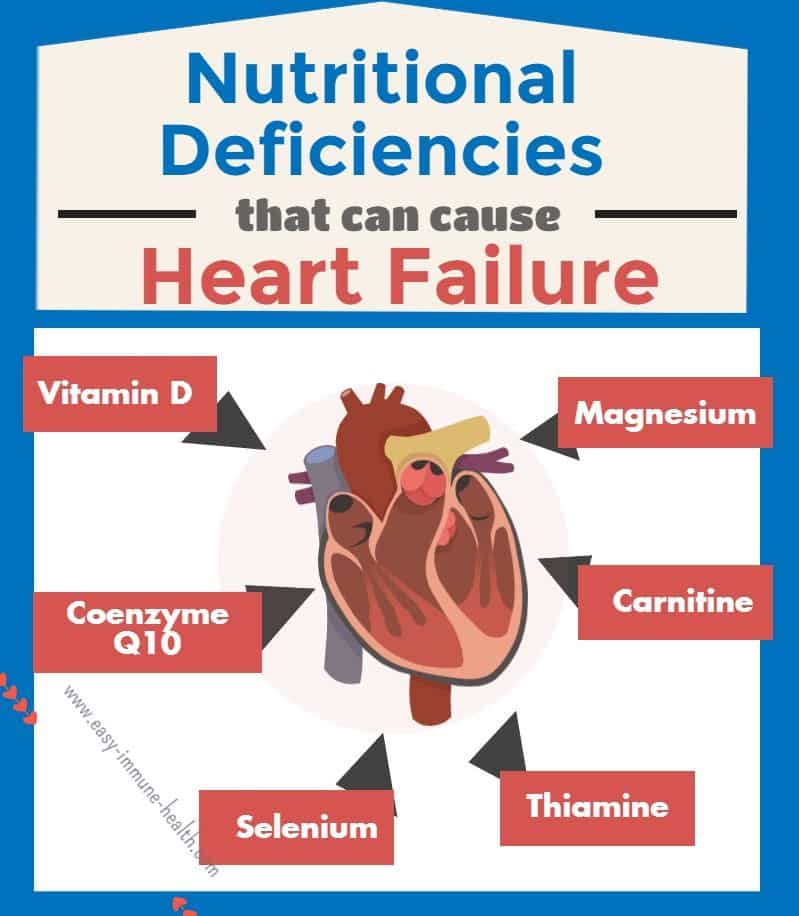
It is estimated that there around 5 million Americans suffering from congestive heart failure and every year another half a million people are diagnosed. This condition occurs when the heart is unable to pump sufficient oxygen-rich blood to meet the demands of the body. It can occur due to various reasons, like elevated blood pressure, malformed valves of the heart, weakening or stiffening of the heart muscle or diseases that demand more oxygen than the heart can supply, like anemia or hyperthyroidism.
As the disease progresses, the symptoms of condition tend to worsen until the eventual death of the person. Some of the common symptoms of congestive heart failure include shortness of breath when doing minor physical activity, fatigue, weakness, edema of the ankles, feet and legs, arrhythmia, constant coughing and wheezing, edema of the abdomen, nausea, lack of appetite, and problems in concentration. These symptoms tend to worsen as the congestive heart failure worsens or becomes more acute.
There are mainly 4 stages of dying from CHF, or congestive heart failure. These stages are described below.
Stage 2: In the second stage of dying, the tiredness becomes worse and the person may also suffer from palpitations of the heart while doing light exercises. However, the symptoms tend to disappear once the person rests for a while.
More Articles :
What Causes Arrhythmic Death
Sudden arrhythmic death syndrome is usually caused by a heart condition that affects the heart’s electrical system. Sometimes, this condition can be inherited, having fatal consequences if undetected and untreated. These conditions include:
- Long QT syndrome .
- Catecholaminergic polymorphic ventricular tachycardia .
- Progressive cardiac conduction defect .
While SADS is diagnosed because the heart appears normal in a post-mortem, there are a few conditions that can cause SADS that make very subtle structural changes to the heart. In these cases, SADS may still be diagnosed because the changes are too small to be seen in an examination.
These conditions include:
Also Check: How To Get Heart Rate
What Is Stage D Heart Failure
We propose that stage D advanced heart failure be defined as the presence of progressive and/or persistent severe signs and symptoms of heart failure despite optimized medical, surgical, and device therapy. Importantly, the progressive decline should be primarily driven by the heart failure syndrome.
What’s The Difference Between Sudden Cardiac Death And Sads
Sudden arrhythmic death syndrome is diagnosed when the cause of death cant be explained in a post-mortem examination because the structure of the heart appears normal.
Sudden cardiac death is when the cause of death can be found in a post-mortem examination because something is wrong with the structure of the heart. Such as, partially or fully blocked arteries after a heart attack.
Don’t Miss: How Do You Measure Heart Rate
Emotional Symptoms Towards The End Of Life
People with heart failure may experience different emotions and feelings. They may feel:
- up and down, with good days and bad days
- like they lack control over their life
- like it’s hard to cope with the reactions of others.
People may not think heart failure is as serious as other illnesses, such as cancer. Patients with heart failure can look well even when they feel very ill.
If a patient has anxiety or depression, their healthcare team will assess how it affects them and whether they need treatment, such as cognitive behavioural therapy or medication.
You can support the patient by providing emotional care and helping them with activities to make them feel better, such as reading, going outside and listening to music or audio books. Find out more about providing emotional care.
What Is The Life Expectancy Of A Person With Congestive Heart Failure
Although there have been recent improvements in congestive heart failure treatment, researchers say the prognosis for people with the disease is still bleak, with about 50% having an average life expectancy of less than five years. For those with advanced forms of heart failure, nearly 90% die within one year.
Recommended Reading: How Dangerous Is Open Heart Surgery
Stages Or Classes Of Heart Failure
Your patient may have been told what stage or class their heart failure is at this explains how severe it is.
NYHA classification divides heart failure into four classes:
- Class 1: no limitation of physical activity. Ordinary physical activity does not cause undue fatigue, breathlessness, or palpitations.
- Class 2: slight limitation of physical activity. Comfortable at rest but ordinary physical activity results in undue breathlessness, fatigue, or palpitations.
- Class 3: marked limitation of physical activity. Comfortable at rest but less than ordinary physical activity results in undue breathlessness, fatigue, or palpitations.
- Class 4: unable to carry out any physical activity without discomfort. Symptoms at rest can be present. If any physical activity is undertaken discomfort is increased.
Patients with advanced heart failure will usually fit into class 3 and 4, despite the best specialist treatment. Read more about the definition of heart failure from NICE .
How Do They Test For Inherited Heart Conditions
An inherited heart condition is usually tested for with a genetic test. A genetic test is usually done with a simple blood test. It can also be carried out on a sample of hair, skin or bodily tissue.
Genetic tests can find genetic faults. A fault could mean you are at risk of developing the same inherited heart condition that your family member has.
If someone has a heart condition or has died from SADS, the immediate family might be referred for genetic tests. The tests are normally done in an inherited heart condition clinic at a hospital or genetics centre.
During your appointment, you might also be asked about your health, family history and if you have any symptoms. Its helpful to bring information about any family members who have passed away unexpectedly or have been diagnosed with heart and circulatory diseases.
Also Check: Where Do You Feel Heart Palpitations
What Is The Most Common Cause Of Sudden Cardiac Death
Coronary artery disease causes most cases of sudden cardiac death. In people who are younger, congenital heart defects or genetic abnormalities in their hearts electrical system are often the cause. In people age 35 and older, the cause is more often related to coronary artery disease.
Other sudden cardiac death causes include cardiomyopathy from:
- Genetic disorders of your heart muscle, including hypertrophic cardiomyopathy and arrhythmogenic cardiomyopathy.
Sudden cardiac death in athletes is rare . Most professional athletic programs will screen their prospective athletes for the most common causes of sudden cardiac death in that population, which in the United States is hypertrophic cardiomyopathy. It also happens more often in people AMAB.
In people who are younger, most sudden cardiac death occurs while playing team sports. In athletes age 35 and older, it happens more often while running or jogging. About 1 in 15,000 joggers and 1 in 50,000 marathon runners have sudden cardiac death.
What Causes Sudden Cardiac Death
Most sudden cardiac deaths are caused by abnormal heart rhythms called arrhythmias. The most common life-threatening arrhythmia is ventricular fibrillation, which is an erratic, disorganized firing of impulses from the ventricles . When this occurs, the heart is unable to pump blood and death will occur within minutes, if left untreated.
Also Check: Open Heart Surgery Risk
How Is Sudden Cardiac Arrest Treated
You can treat and reverse sudden cardiac arrest. However, emergency action has to start immediately. Survival can be as high as 90% if treatment starts within the first minutes after sudden cardiac arrest. The rate drops by about 10% each minute longer.
If you see someone experiencing sudden cardiac arrest, do this:
Once emergency personnel arrive, defibrillation can restart the persons heart if they havent received a shock from an AED yet. Defibrillators shock your heart through paddles placed on your chest. Emergency personnel will also give intravenous medications called antiarrhythmics that work to restore the hearts electrical rhythm.
After successful defibrillation, most people need hospital care to recover from the effects of their sudden cardiac arrest and to treat and prevent future cardiac problems.
Reversal Of Remodelling To Prevent Acute Cascading Mechanical Failure
Fortunately, recent experiences with cardiac resynchronization and neprilysin inhibition in large-scale trials in HFrEF have provided unique opportunities to clarify this confusion. These observations have supported the premise that ventricular remodelling is a direct cause of cascading collapse and sudden death.
First, cardiac resynchronization exerts striking benefits on ventricular remodelling without interfering with neurohormonal systems as a result, trials of cardiac resynchronization are poised to identify a unique role for ventricular geometry in the genesis of sudden death. It is therefore noteworthy that, when cardiac resynchronization induces significant reverse remodelling, the substrate for acute electrical cascade is reduced , the risk of sudden death is decreased by 50% in patients without an ICD, primarily related to a decrease in lethal ventricular tachyarrhythmias in those who experience a marked decrease in ventricular volumes ., In contrast, in patients with severe symptoms and persistently dilated and fibrotic hearts, a significant risk for sudden death remains following cardiac resynchronization, and it is not reduced by an ICD.,
You May Like: What Causes High Blood Pressure And Low Heart Rate
Scd In Patients With Hfpef
Although patients with HFpEF were less prone to SCD compared to patients with HFrEF, patients with HFpEF did account for a significant proportion of all HF patients who encountered SCD. An observational study in Netherland showed that the incidence of SCD in patients with a LVEF> 50% and a previous HF history was 19%, while the incidence of SCD was 61% in patients with a LVEF> 50% but without HF history . Another study by Stecker et al. assessed 121 SCD patients who had LVEF data before SCD. They found that 48% of these SCD patients have a normal LVEF, while 30% and 22% of these SCD patients have a severely reduced and mildly to moderately reduced LVEF, respectively . The incidence of SCD in patients with HFpEF remains unknown in these two studies. In the TOPCAT, I-PRESERVE, and CHARM-Preserved trials, SCD consistently accounted for around one fourth of total death in HFpEF patients in these trials . In the I-PRESERVE trial, the annual SCD rate was 1.35% in patients with HFpEF .
Mechanisms Of Scd In Hfref
HF was associated with increased action potential duration and transmural heterogeneity of repolarization, leading to increased arrhythmic events and SCD . This electrical remodeling is the consequence of dysregulation of different ion channels, especially the potassium channels , and the transient outward potassium current has been shown to result in electrical dispersion and triggered activity in the failing hearts. Sodium channels are also responsible for the maintenance of AP plateau and repolarization so that alterations of INa in HF patients may lead to pro-arrhythmic states . Intracellular calcium not only mediates myocardial contraction but also influences electrophysiological balance . Dysregulation of calcium channels is also responsible for excitationcontraction uncoupling and arrhythmogenesis .
You May Like: Does Caffeine Increase Heart Rate
What Is Sudden Cardiac Death In Patients With Heart Failure
The original definition of sudden cardiac deathi.e. demise within 1 h of the onset of new cardiac symptomswas developed to identify the event in the general population with no known heart disease. However, this approach could not be applied to patients with HFrEF, who had ongoing symptoms and an established cardiovascular disorder. Initially, patients with HFrEF were deemed to have died suddenly if their symptoms had not recently worsened, and if another cause for cardiac arrest could not be identified. Yet, this approach was difficult to apply in practice. Technically, all deaths were sudden, since the patient was alive at one moment and dead at the next observation point. Therefore, the feature that distinguished instantaneous demise was not its suddenness, but its unexpectedness. If an event had not been foreseen, physicians believed that a new mechanism had emerged and had triggered the abrupt circulatory collapse.
What Are The Symptoms Of End
Heart Failure: Quick Facts
1. More than 6 million U.S. adults have heart failure.
2. About half of people who develop heart failure die within 5 years of diagnosis.
3. Most people with end-stage heart failure have a life expectancy of less than 1 year.
4. The leading causes of heart failure are diseases that damage the heart, such as heart disease, high blood pressure, and diabetes.
Heart failure worsens over time, so symptoms are most severe during the final stages. It causes fluid to build up in the body, which produces many of these symptoms:
- Shortness of breath . In the final stages of heart failure, people feel breathless both during activity and at rest.
- Persistent coughing or wheezing. This may produce white or pink mucus. The cough may be worse at night or when lying down.
- Weight gain or swelling of the feet, ankles, legs, abdomen, or neck veins.
- Tiredness, weakness.
In addition, people in the final stages of heart failure may suffer from:
- depression, fear, insomnia, and isolation
- anxiety about their future
- trouble navigating the health care system
Also Check: Does Menopause Cause Heart Palpitations
Who Is At Risk For Sudden Cardiac Arrest
You are at higher risk for SCA if you:
- Have coronary artery disease . Most people with SCA have CAD. But CAD usually doesn’t cause symptoms, so they may not know that they have it.
- Are older your risk increases with age
- Are a man it is more common in men than women
- Are Black or African American, especially if you have other conditions such as diabetes, high blood pressure, heart failure, or chronic kidney disease
- Have a personal history of heartbeats that aren’t regular
- Have a personal or family history of SCA or inherited disorders that can cause arrhythmia
- Have a problem with drug or alcohol use
- Have had a heart attack
- Have heart failure
Moderate Stage Of Chf
At Stage C, as the heart continues to fail, the person develops weakness and significant fatigue, shortness of breath or palpitations with the slightest physical exertion. She begins to limit activity because of these symptoms as she is only comfortable when resting. A doctor’s evaluation and testing shows moderate signs of heart dysfunction,
Other possible symptoms might include more visible edema of the lower extremities and the hands might also swell as the fluid congestion in body tissues increases. Shoes and rings might be tighter. The pulse might become weaker because of the struggling heart.
Recommended Reading: How To Reduce Heart Palpitations During Pregnancy
