What Are The Symptoms Of Advanced Heart Failure
Symptoms of advanced heart failure may include that you:
- are very short of breath despite not exerting yourself or even at rest, while you are already on quite a few medicines
- need more help with day-to-day chores, such as getting dressed, preparing meals or personal care
- lose your appetite
- feel weak, with no energy and feel very tired
- have repeated hospital admissions due to heart failure or needed to see your doctor multiple times
- are losing weight
- stay in bed most of the time and move around less.
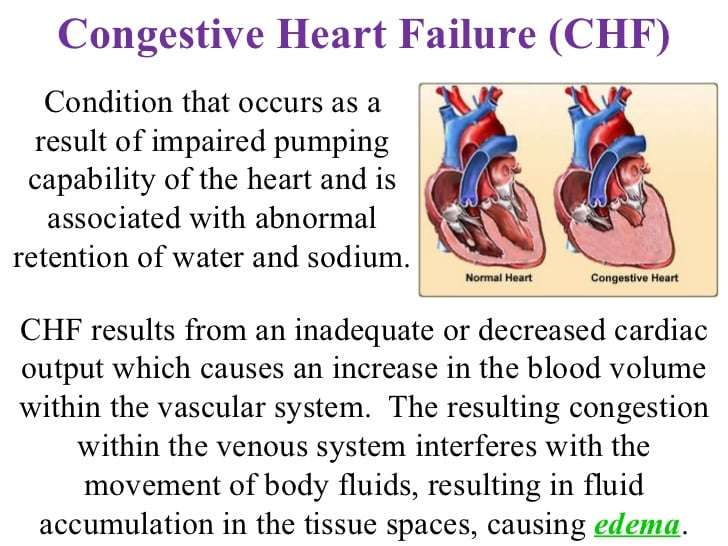
What Is Congestive Heart Failure
The term heart failure might sound like the heart has stopped working entirely but this is actually not the case. Rather, this is a common problem that affects around 6 million Americans with 670,000 new cases diagnosed each year.
What CHF actually describes is a weakening of the heart. This means that the power it has to pump blood around the body has been reduced and therefore the blood and oxygen move around the body at a slower rate. This can result in the chambers of the heart enlarging in order to hold more blood to pump or it might cause them to become stiffer and thickened to keep the blood moving. The danger is that the muscle walls in the heart might eventually grow even weaker and therefore be unable to maintain circulation. At this point, the kidneys can respond by causing the body to retain fluid and salt which might build up in the arms, legs, ankles and feet. The body thus becomes congested and hence the term congestive heart failure is used to describe this condition.
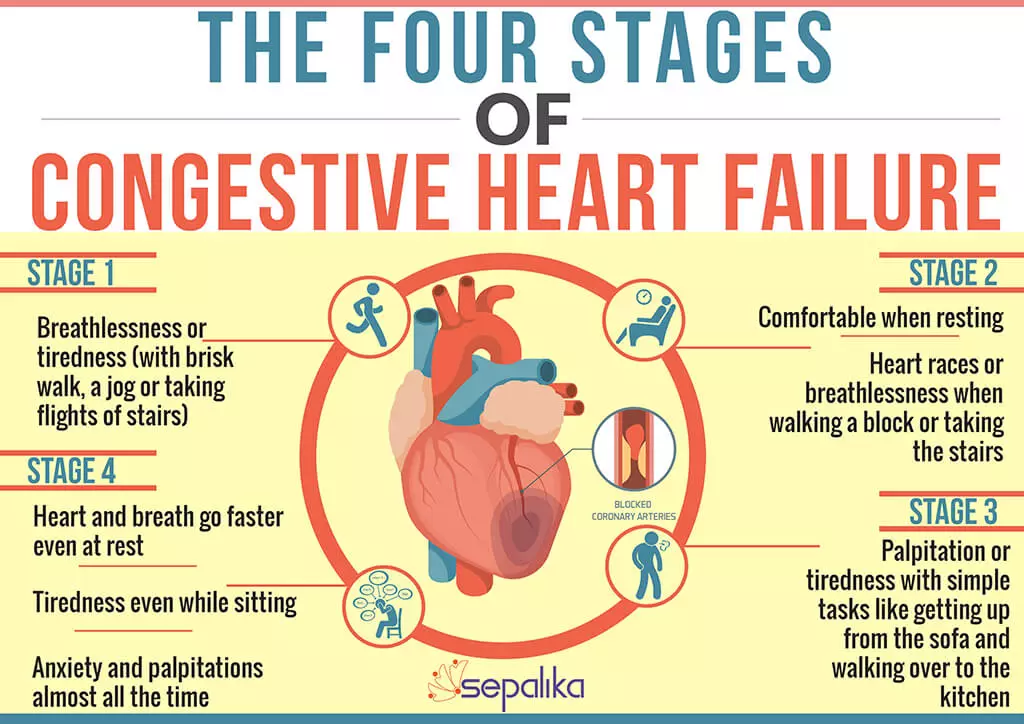
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the “Stages of Heart Failure.” These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
Recommended Reading: What Does Increased Heart Rate Mean
What To Look Out For
Ideally, you’ll want to seek help long before symptoms get severe. Your body will show early signs of acute heart failure, such as worsening edema of your lower legs, ankles or feet and weight gain. Seek help if you experience worsening fatigue, irregular heart beat, rapid heart beat, chest pain, dizziness, or confusion. You should also seek help when you experience worsening shortness of breath, or any of the signs and symptoms noted above for acute left heart failure.
Not everyone with COPD will develop heart failure. There is no cure, but it can be treated. It’s important to know that people are living longer than ever before thanks to modern wisdom and medicine. So, if you experience any of the above symptoms, tell your doctor, and call 911 if you need to. The sooner you seek help the easier it is to fix you and get you back to your home.
European Society Of Cardiology’s Guidelines For Diagnosis Of Heart Failure
Essential features
- ArrhythmiasAtrial fibrillation ventricular arrhythmias bradyarrhythmias
- ThromboembolismStroke peripheral embolism deep venous thrombosis pulmonary embolism
- GastrointestinalHepatic congestion and hepatic dysfunction malabsorption
- MusculoskeletalMuscle wasting
- RespiratoryPulmonary congestion respiratory muscle weakness pulmonary hypertension
Recent observational data from the studies of left ventricular dysfunction and vasodilator heart failure trials indicate that mild to moderate heart failure is associated with an annual risk of stroke of about 1.5% , rising to 4% in patients with severe heart failure. In addition, the survival and ventricular enlargement study recently reported an inverse relation between risk of stroke and left ventricular ejection fraction, with an 18% increase in risk for every 5% reduction in left ventricular ejection fraction this clearly relates thromboembolism to severe cardiac impairment and the severity of heart failure. As thromboembolic risk seems to be related to left atrial and left ventricular dilatation, echocardiography may have some role in the risk stratification of thromboembolism in patients with chronic heart failure.
Read Also: Is Congestive Heart Failure Curable
Diagnosis Of Heart Failure Of Acute Onset
|
Data from Ponikowski P, Voors AA, Anker SD, et al: 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology Developed with the special contribution of the Heart Failure Association of the ESC. European Heart Journal 37:2129-2200, 2016. doi: 10.1093/eurheartj/ehw128 |
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
You May Like: When To Go To The Hospital For Rapid Heart Rate
Acute Episodes Of Left Heart Failure
You may experience weight gain. Blood may get backed up into your lungs, causing fluid in your lungs . This may cause you to feel like you have to sit up to breathe . You may have a cough, which may be productive of pink, frothy secretions . Your oxygen levels may be low. Your breathing and heart rate may increase. Blood will be shunted to your vital organs, so you may feel cold and clammy to the touch, and the skin around your lips and fingertips may appear blue . You may feel fatigue, weakness, and anxiety. These are all severe signs and symptoms, meaning that you need to seek immediate medical attention. Call 911.2, 5
What Tests Will I Need
Healthcare providers use a variety of tests to assess your symptoms, such as:
- Electrocardiogram to record and assess the hearts electrical activity.
- Chest X-ray to check for fluid build-up in the heart or lungs.
- Echocardiogram to show heart movement and blood flow.
- Angiography or heart catheterization to examine the hearts blood vessels.
You may also need lab tests that include:
- BNP blood test to check for hormones that occur when pressures change inside the heart.
- Basic metabolic panel which shows signs of kidney or thyroid issues.
Recommended Reading: How Do You Find Your Maximum Heart Rate
Palliative And Hospice Care
Someone living with a serious condition like heart failure can access palliative care at any stage of their condition. Palliative care is intended to support overall wellness and quality of life and can happen alongside other treatments.
With very severe heart failure, people may choose to access hospice care to receive supportive care at the end of life.
How Is Heart Failure Diagnosed
Your doctor will ask you many questions about your symptoms and medical history. Youâll be asked about any conditions you have that may cause heart failure . Youâll be asked if you smoke, take drugs, drink alcohol , and about what drugs you take.
Youâll also get a complete physical exam. Your doctor will listen to your heart and look for signs of heart failure as well as other illnesses that may have caused your heart muscle to weaken or stiffen.
Your doctor may also order other tests to determine the cause and severity of your heart failure. These include:
Other tests may be ordered, depending on your condition.
Don’t Miss: How To Reverse Heart Failure
What Are The Symptoms Of Heart Failure Exacerbation
When heart failuresymptoms suddenly or slowly get worse, this may be a sign of heart failureexacerbation. Symptoms of heart failure include:
- Breathing problems or shortness of breath.
- Chronic coughing or wheezing.
- Nausea or lack of appetite.
- Feeling light-headed.
- Increased heart rate or irregular heartbeat.
- Buildup of fluid in the legs, ankles, feet, or abdomen.
- Difficulty breathing when lying down.
Receive The Best Care For Your Heart And Stay Safe With Dispatchhealth
Anyone with a history of heart disease knows the stress associated with this condition. What seems like minor symptoms for others, such as fatigue, can be especially scary when youre constantly on the lookout for symptoms related to your illness. When it comes to your heart, you should be assessed if you think something is wrong. DispatchHealth offers a better solution than travelling to an urgent care facility for non-life-threating situations. When heart failure exacerbations occur, DispatchHealth will come to you and evaluate the situation. Our experienced medical staff has the ability to use an EKG to assess heart rhythms and develop a treatment plan. To schedule an appointment, you can call, click here, or download our app.
If this is an emergency, please call 911 or go to the nearest emergency department.
Recommended Reading: End Stage Heart Failure How Long To Live
Recognizing Symptoms Of Heart Failure Exacerbation
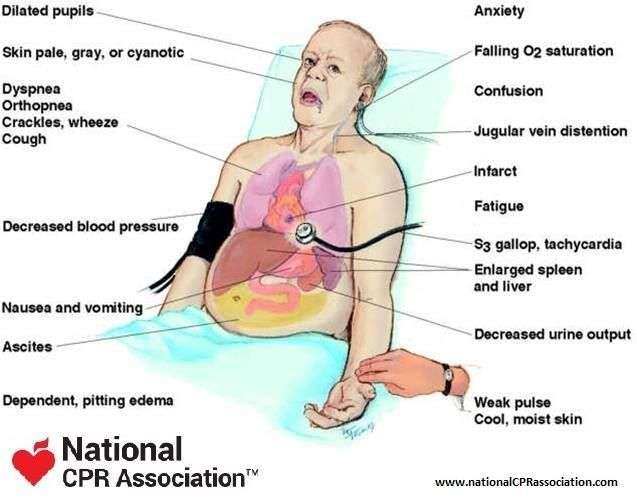
What Are The Most Common Symptoms Of Congestive Heart Failure
Swelling is the most common symptom of congestive heart failure. Often, swelling is most apparent in the extremities, especially in the legs and ankles, but it can occur in other parts of the body as well. Fluid collection in and around the lungs can cause shortness of breath , especially during physical activity or when lying down. Other common symptoms of heart failure include fatigue, loss of appetite, and weight gain.
Recommended Reading: Recovery After Heart Surgery
What Is A Chf Exacerbation & How You Can Manage It
In this article, you can know about chf exacerbation here are the details below
Individuals with this condition can often experience CHF exacerbations, which are characterized by getting worse symptoms. Symptoms of CHF can involve shortness of breath and coughing or wheezing, inflamed ankles or legs, weight gain, tiredness, and heart palpitations.1 A CHF exacerbation can be triggered by many aspects, such as high salt intake and lung infections.
Individuals with CHF can successfully handle their condition with medications and lifestyle changes. In the United States, around six million individuals have CHF, and it is the leading reason for hospitalizations.2. Also check white nails.
Is There A Treatment For Heart Failure
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are to try to keep it from getting worse , to ease symptoms, and to improve quality of life.
Some common types of medicines used to treat it are:
- ACE inhibitors
- Aldosterone antagonists
- Selective sinus node inhibitors
- Soluble guanylate cyclase stimulator
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. It usually includes workouts that are designed just for you, education, and tips to lower your chance of heart trouble, like quitting smoking or changing your diet.
Cardiac rehab also offers emotional support. You can meet people like you who can help you stay on track.
You May Like: What Heart Chamber Pushes Blood Through The Aortic Semilunar Valve
Other Possible Treatment Choices Include:
Ultrafiltration treatment: This procedure resembles dialysis and by hand eliminates fluid from the body. This is used if diuretics dont get rid of enough fluid.9.
Vasodilators: These medications open your blood vessels so the blood can flow more easily. This can assist resolve the symptoms of lung edema and high blood pressure.
Inotropic drugs: Two typically used inotropic substance abuse to deal with CHF exacerbation are dobutamine and milrinone. They help make your heartbeats more powerful.8.
Although beta-blockers can trigger CHF exacerbation, your healthcare provider may resume beta-blocker therapy or include a low dosage to your treatment plan if your fluid volume remains typical.8.
Once your fluid volume, blood pressure, and heart function are stable, your doctor will release you. They might advise modifications to your diet or CHF therapy.
What Is The Prognosis For People With Heart Failure
The prognosis for heart failure varies widely and depends on the underlying cause and whether it can be treated.
Your outlook depends on a variety of factors, including:
- Heart failure cause and severity.
- How quickly you receive care.
- Your overall health and response to treatment.
- Commitment to heart-healthy living.
Recommended Reading: What Is A Dangerous Heart Rate For A Woman
Look After Your Mental Health
You also need to look after your mental health. You might have lots of different feelings while coping with your symptoms, such as anxiety, stress or depression.
Try to avoid stressful situations. If you get stressed, use relaxation techniques such as taking 6 slow, deep breaths. Doing something where you feel useful and gain a sense of achievement can help you regain balance in your life. It also helps to have plenty of rest and get a good night’s sleep, as this allows your body and mind to restore. Talking to family/whnau members can also help. If you need more support, ask your healthcare team for a referral to a psychologist or counsellor.
When To Get Medical Advice
See your GP if you experience persistent or gradually worsening symptoms of heart failure.
The symptoms can be caused by other, less serious conditions, so it’s a good idea to get them checked out.
Call 999 for an ambulance or go to your nearest accident and emergency department as soon as possible if you have sudden or very severe symptoms.
This is a medical emergency that may require immediate treatment in hospital.
Page last reviewed: 19 May 2022 Next review due: 19 May 2025
Also Check: Heart Failure Guidelines Acc/aha
Heart Failure Symptoms By Class And Stage
- print page
- Bookmark for later
Heart failure is a complex, chronic syndrome that gets worse over time. During the diagnostic process, physicians classify each case of heart failure. The American College of Cardiology/American Heart Association and the New York Heart Association have complementary classification systems.1-4
The ACC/AHA stages reflect the range from a high risk of developing heart failure to advanced heart failure and are associated with an approach to treatment plans.1-4 The New York Heart Association clinical classifications of heart failure reflect the severity of symptoms or functional limits due to heart failure.1-2 A diagnosis can have an assignment of a stage and a class.
