What Happens During This Procedure
A heart transplant is a complicated surgery that usually involves the following steps.
General anesthesia
Heart transplant always involves general anesthesia, which puts you into a deep sleep. While youre asleep, providers will insert a tube down your throat, attaching the end of the tube outside your body to a machine called a ventilator. The ventilator will keep you breathing even though youre under anesthesia.
After youre under anesthesia, providers will lower your body temperature to around 82 degrees F . Lowering your body temperature means the activity of your cells slows down. That prevents damage to your cells when blood flow stops during various steps of the surgery.
Removing your heart
At some point, providers will also add blood thinners like heparin to your blood to keep it from clotting at the wrong time. Theyll then reroute all the blood in your body through a device called a heart-lung bypass machine. That device adds oxygen and removes carbon dioxide from your blood, and also keeps your blood circulating.
To make room for the donor heart you’ll receive, doctors have to perform a procedure called cardiectomy to remove your heart. This procedure involves clamping off all the major blood vessels that connect to your heart and disconnecting your heart from them.
Implanting the donor’s heart
What About Acute Liver Failure
Acute liver failure is often treated in the intensive care unit of a hospital. Supportive care is given to help stabilize the condition and control any complications during treatment and recovery.
If a medication overdose or reaction is suspected, drugs may be given to reverse the effects. A liver transplant may also be recommended for some people with acute liver failure.
You can help to prevent liver failure by making lifestyle changes that keep your liver happy and healthy. Here are some tips for improving liver health:
- Drink alcohol in moderation, and never mix medications with alcohol.
- Take medications only when needed, and carefully follow any dosing instructions.
- Dont mix medications without first consulting your doctor.
- Maintain a healthy weight theres a connection between obesity and fatty liver disease.
- Get vaccinated against hepatitis A and B.
- Be sure to have regular physicals with your doctor during which they perform liver blood tests.
Also Check: What Is A Typical Resting Heart Rate For A Healthy Individual
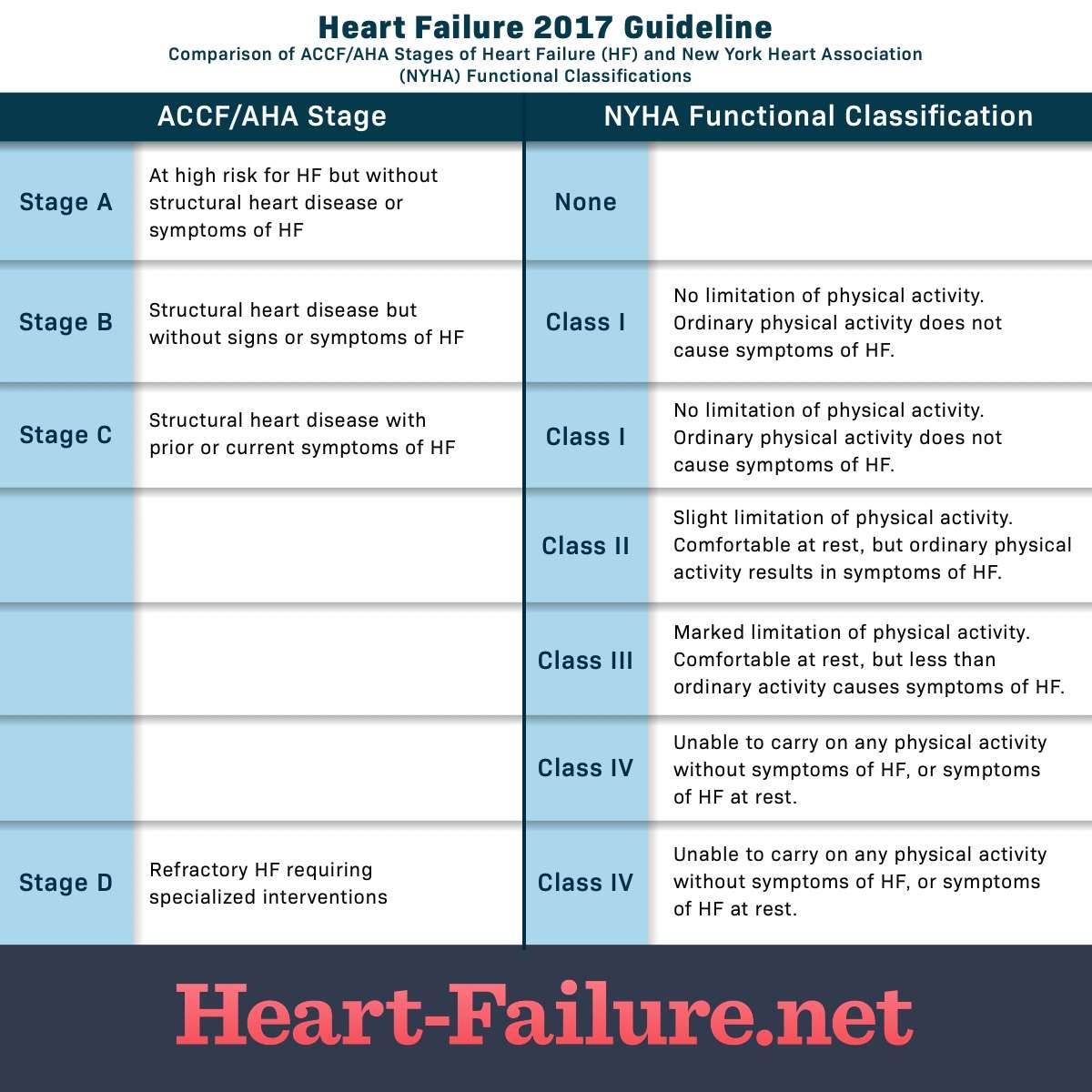
New York Heart Association
This association will state the various ways of heart failure and the things which will cause heart failure and related heart disease. This association classifies the stages of heart failure into four classes. These are class I, class II, class III, and class IV. These are classified on the basis of symptoms.
Read Also: What Drugs Should Be Avoided In Heart Failure
Types Of Heart Failure
The main types of heart failure are named for where they occur in the heart:
- Left-sided heart failure
- Biventricular heart failure
Clinicians also may classify heart failure as:
- Acute: You have active symptoms of heart failure, with either a new diagnosis or with long-term heart failure.
- Chronic: You have a history of heart failure, but your condition is relatively stable with no symptoms or with manageable symptoms.
What Are The Types Of Heart Failure
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure
Heart failure with reduced left ventricular function The lower left chamber of your heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of your body.
Heart failure with preserved left ventricular function Your heart contracts and pumps normally, but the bottom chambers of your heart are thicker and stiffer than normal. Because of this, your ventricles can’t relax properly and fill up all the way. Because there’s less blood in your ventricles, your heart pumps out less blood to the rest of your body when it contracts.
Right-sided heart failure
Heart failure can also affect the right side of your heart. Left-sided heart failure is the most common cause of this. Other causes include certain lung problems and issues in other organs.
Also Check: Can Omeprazole Cause Heart Palpitations
When To Seek Hospice Care
Even physicians have difficulty determining life expectancy for people with end-stage heart-failure. The condition can be unpredictable, and symptoms can change. However, certain signs can indicate that hospice care would be beneficial, including:
- frequent chest pain
- significant fatigue or shortness of breath
- substantial decline in ability to do daily activities, such as self-care
- The patient has already received the best possible treatment, which are no longer working well, and the patient is not a candidate for other interventions.
- The patient has received the best possible treatment and has decided to decline further specialized interventions.
People can be reluctant to start hospice, as they may worry it means theyre giving up or that it will hasten death. But such concerns are unfounded. In fact, patients and families often wish they had started hospice sooner, because it makes such a positive difference in their lives. And research shows that early admission to hospice results in greater satisfaction with care among patients and family caregivers.
How Chf Is Diagnosed
There are several ways a doctor can diagnose heart failure, aside from considering your own medical history and your family history, as well as administering a physical exam. You might be asked to take a stress test to see how your heart responds to physical demands, for example.
The doctor can also turn to an electrocardiogram to monitor your hearts electrical activity, as well as a chest X-ray to pinpoint an enlarged heart or damaged lungs. It can also use a blood test for B-type natriuretic peptide to determine how severe the heart failure is.
You May Like: Can Low Potassium Cause Heart Palpitations
How Can Heart Failure Affect People Towards The End Of Life
At any stage of someones illness, heart failure can have a significant psychological impact on a person. People experience different emotions, including anger, sadness and worry. Life may feel very up and down, with good days and bad days. People can feel low about their symptoms and limitations, or they may feel that they lack control over their life. It can be particularly shocking for someone if they have been told their outlook is poor.
Symptoms can fluctuate at the advanced stage of heart failure, making it hard to estimate prognosis . This can make it difficult to know how and when to discuss the future and find out how someone would like to be cared for at the end of their life.
People with heart failure are more likely to have renal failure. Renal failure can make prescribing certain medications difficult which can, lead to more symptoms and discomfort.
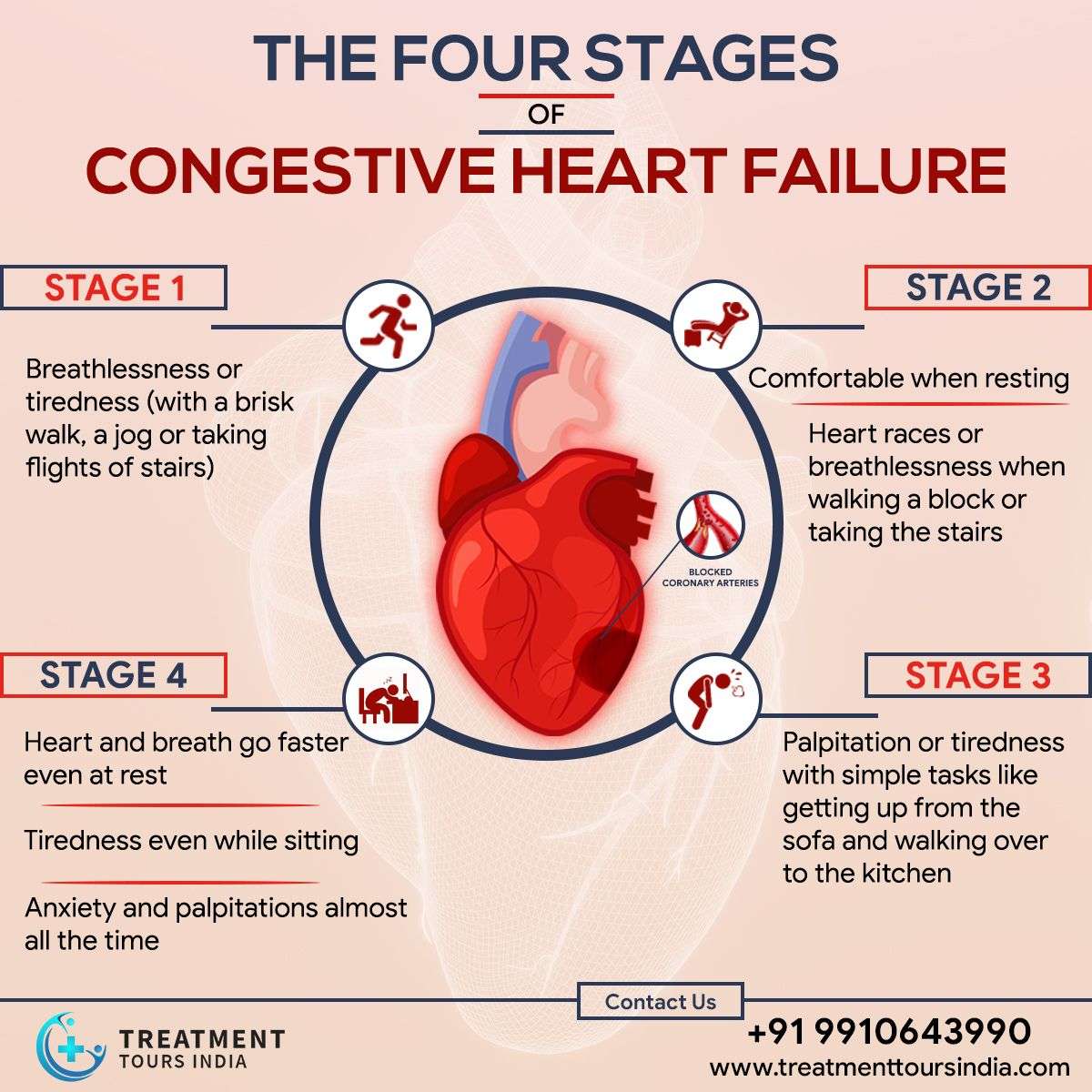
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the Stages of Heart Failure. These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
Recommended Reading: How To Record Heart Rate
Stage 2 Of Congestive Heart Failure
Stage two of congestive heart failure will produce symptoms such as fatigue, shortness of breath, or heart palpitations after you participate in physical activity. As with stage one, lifestyle changes and certain medication can help improve your quality of life. Your doctor will discuss treatment with you and help you on your healthcare journey while living with CHF.
How Do Doctors Diagnose Congestive Heart Failure
Heart failure is diagnosed with a physical exam and tests that may include:
- Electrocardiogram to measure the electrical activity in the heart
- Brain natriuretic peptide or N-terminal pro-BNP blood tests
- BNP or NT-proBNP level is high in people with heart failure
Recommended Reading: Does Magnesium Help With Heart Palpitations
Symptoms Of Heart Failure
The main symptoms of heart failure are:
- breathlessness after activity or at rest
- feeling tired most of the time and finding exercise exhausting
- feeling lightheaded or fainting
- swollen ankles and legs
Some people also experience other symptoms, such as a persistent cough, a fast heart rate and dizziness.
Symptoms can develop quickly or gradually over weeks or months .
How Do I Manage My Heart Failure
Its important to follow the advice from your doctor and take the medicines youre prescribed. Making changes to your lifestyle is another way to improve your health. Changes you could try are:
- keeping active which has been proven to boost energy and improve sleep and quality of life
- keeping to a healthy weight and diet this will help your overall health and prevent extra strain on your heart
- limiting how much alcohol you drink – lowering your chance of getting abnormal heart rhythms, high blood pressure and diseases such as stroke, liver problems and some cancers
- stopping smoking and using other tobacco products – reducing your risk of developing heart and circulatory diseases
- watching the amount of fluid you have each day if advised by your medical team
- weighing yourself regularly sudden weight gain may mean too much fluid is building up in your body and will need treated.
Living a healthier lifestyle can be hard at first, but its important for your overall quality of life. Visit our healthy living hub to start eating healthier and manage things like smoking and stress today.
Also Check: Can Lisinopril Cause Heart Palpitations
What Are The Stages Of Chf
Congestive heart failure is a progressive condition that can worsen over time. Depending on the severity of CHF and its associated symptoms, cases are classified into one of four potential categories:
|
Stage |
||
|
Stage I CHF can typically be managed through lifestyle modifications and medicaiton. |
||
|
Physical activity may lead to symptoms such as palpitations, shortness of breath, and fatigue. |
Management of Stage II CHF is very similar to Stage I but may require more careful monitoring. |
|
|
Any physical activity is likely to result in notable symptoms, more severe than Stage II. |
Treatment of Stage III CHF is far more complicated than lower stages. Consult with a cardiologist to learn more. |
|
|
Symptoms are always present, even while at rest. Physical activity is likely not possible. |
Stage IV CHF has no cure, but there are options available to increase patient comfort. Speak with a cardiologist to learn more. |
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Also Check: How Long To Recover From Heart Attack
Treatment Options For Stages C And D
In stage C, there can be ACE inhibitors and beta-blockers, as well as several other medications, such as hydralazine or diuretics. An ICD or biventricular pacemaker may also be an option. Lifestyle adjustments, including reducing salt and losing weight, can be other approaches to managing CHF.
In stage D youll likely need a ventricular assistance device or a heart transplant. Continuous infusion of intravenous inotropic drugs may also be an approach at this advanced stage, explains WebMD.
The Four Stages Of Heart Failure
- Reactions 0 reactions
There are four stages of heart failure. The stages range from being at risk of heart failure to having advanced heart failure. These stages were created by the American Heart Association and the American College of Cardiology and were given letter titles A, B, C, and D. Each stage has different recommended treatments depending on a multitude of factors.1
Don’t Miss: How Long Can You Live With Stage 4 Heart Failure
When And What To Discuss With Doctor About Stage 4 Ckd
Having a close relationship with your doctor is vital for optimal kidney disease treatment. You should disclose any problems and concerns that you may be having as well as symptoms that develop. This is important as your doctor will be able to pick out and investigate potential problems before they become any more serious.
For the sake of convenience, you may discuss with your doctor your dialysis options and whether you can perform dialysis from the comfort of your own home. Speaking directly to a nephrologist will also provide more insight into your condition.
Those with stage 4 kidney disease are expected to visit their doctor at least every three months, getting a full workup and making sure the treatment plan is working well.
Read Also: Claritin Heart Racing
How Are Obesity And Heart Disease Related
Obesity affects more than 40% of the U.S. population. The excess fat in obesity was originally thought to be harmless . However, we now know that excess fat causes chemical changes in your blood that increase your heart disease risk. When your fat cells become enlarged, they give off hormones that produce chronic inflammation.
Inflammation can lead to your body no longer using insulin efficiently . This means your body has trouble regulating your blood sugar levels, which can result in metabolic syndrome. Having this condition means you have risk factors that increase your chance of developing heart disease, such as:
How does body shape affect your heart disease risk?
Your risk of heart disease varies based on where your body stores excess fat. People with an apple shape have a higher risk of heart disease than people with a pear shape. Your healthcare provider may measure your waist circumference to understand the degree of abdominal obesity you have as this correlates well with a higher risk of heart disease.
How else can obesity affect your heart?
Increased body fat may also directly contribute to changes in your heart, including:
Obesity also increases your risk of irregular heartbeat . Research shows it may cause one-fifth of all cases of atrial fibrillation . Afib can lead to blood clots that cause stroke.
You May Like: Most Common Heart Surgeries
Living With Congestive Heart Failure: What To Expect
Yes, there are several lifestyle changes you should take into account if youve been diagnosed with congestive heart failure. But remember your diagnosis doesnt mean you should necessarily stop doing things you love.
You are supposed to be exercising walking, biking, swimming, or doing light weight exercises, says Mountis. The American Heart Association recommends at least 30 minutes of moderate intensity aerobic activity at least five days a week for optimal heart health. Avoid exercises that make you feel breathless, and make sure to talk to your doctor before starting a new exercise routine.
Your healthcare provider will also likely suggest dietary changes that can help reduce the swelling associated with congestive heart failure and slow the progression of the condition. Those changes may include following a low- or reduced-salt diet, or reducing how much fluid you drink to lessen the bodys water content.
Other lifestyle changes that can slow the progression of heart failure include:
