What Causes Atrial Fibrillation
Sometimes the cause of AFib is unknown. Other times, it is the result of damage to the heart’s electrical system from other conditions, such as longstanding, uncontrolled high blood pressure or coronary artery disease. AFib is also the most common complication after heart surgery.
Learn about the important connection between atrial fibrillation, high blood pressure and stroke.
Can Taking Too Many Medications Impact Older Adults With Heart Failure
Yes. As we age, the body doesnt handle the medicine in the same way. It metabolizes medicines differently, which is why taking too many medications can be a problem for older patients with heart failure. As we age, the liver and kidneys dont work as well, so drugs can sometimes build up in the system. Older people on medicines for their heart might be on five, six or 10 other drugs. So theyre taking a whole cocktail of medicines that might not work well together and could have side effects. Its helpful to re-prioritize medications with your doctor. Over-the-counter pain medications can sometimes be very dangerous in older people because they can raise blood pressure and harm the kidneys. They can also have a sedative effect on people and cause delirium.
Things That Raise Your Odds Of Heart Failure And Afib
AFib and heart failure are both common on their own. But many people have both, and doctors aren’t totally clear why. One reason may be that many of the same things raise your chances of having both conditions.
Risks you can’t control. Some things you just can’t change, such as:
- Age. The older you are, the greater the chances you’ll get AFib or heart failure. Most people who have both conditions are older adults.
- Genes. There’s still a lot of research to be done here, but certain differences in your genes may affect how likely it is that you end up with heart failure or AFib.
- Gender. Men are more likely to have these conditions than women.
Heart disease. Your odds for heart failure and AFib go up if you have other heart conditions, such as:
- Coronary artery disease, where plaque builds up in your heart’s arteries and leads to less blood flow
- Cardiomyopathy, which is damage to your heart muscle
- Heart valve problems, such as a leaky valve or a valve that doesn’t fully open
- Myocarditis, where the muscles of your heart get swollen and irritated
Other health conditions. Other health issues can also raise your risk, such as:
Smoking and drinking alcohol. Just on its own, smoking raises your odds for all kinds of heart disease, including AFib and heart failure. But it’s even more dangerous if you have risks in play.
Over time, heavy drinking weakens your heart’s muscles. And for some people, alcohol acts as a trigger for AFib.
Show Sources
Recommended Reading: What To Do When Someone Having Heart Attack
Interventional Management: Rhythm Control With Catheter Ablation
There has been increasing evidence in catheter ablation for patients with AF and HFrEF. So far, there have been 8 published randomized trials assessing the efficacy of AF ablation in patients with HFrEF . There were variabilities in the ejection fraction inclusion, ranging from 35% to < 50%. Most of the studies included only persistent AF. There were also variabilities in trial design with the control group ranging from medical rate control, amiodarone, AV node ablation and biventricular pacing, or best medical therapy with either rate or rhythm control.
What Causes Atrial Fibrillation To Start
Changes or damage to your hearts tissue and electrical system cause atrial fibrillation. Usually, coronary artery disease or high blood pressure causes those changes. Often a trigger heartbeat causes atrial fibrillation to begin. But sometimes its hard to know the cause of that triggered heartbeat. For some people, there is no identifiable cause. Research is constantly providing new information to help us learn more about the
Afib often runs in families. So, if a close family member has Afib, you have a family history and therefore a higher chance of developing it, too.
Can atrial fibrillation be caused by anxiety?
We dont fully know the connections between atrial fibrillation and anxiety. Research has identified Afib as a cause of anxiety . But few studies have explored anxiety as a cause of Afib. We do know that anxiety can raise your risk of cardiovascular disease and causes a 48% higher risk of cardiac death. However, we need more research to find out if anxiety disorders can cause Afib.
Read Also: Types Of Open-heart Surgery
Symptoms Of Heart Failure
The main symptoms of heart failure are:
- breathlessness after activity or at rest
- feeling tired most of the time and finding exercise exhausting
- feeling lightheaded or fainting
- swollen ankles and legs
Some people also experience other symptoms, such as a persistent cough, a fast heart rate and dizziness.
Symptoms can develop quickly or gradually over weeks or months .
Also Check: When Does A Heart Attack Occur
Af Treatment In The Setting Of Hf
Pharmacological rhythm control is especially difficult in patients with HFrEF. Most AADs cannot be instituted because of their negative inotropic effects. Amiodarone is the only AAD approved for HFrEF but is unfortunately associated with many adverse effects. Therefore, rate versus rhythm strategies were performed to assess whether there was any benefit for rhythm control. Noteworthy, these trials were performed before the era of ablation . The largest trial that studied rate versus rhythm control trial in patients with HF, the AF and congestive heart failure trial, included 1376 patients with LVEF of 35% or lower and randomised to a rate or pharmacological rhythm control strategy. No differences were observed in all-cause mortality or secondary outcomes . In the recent Routine vs Aggressive risk factor driven upstream rhythm Control for prevention of Early atrial fibrillation in heart failure trial included stable patients with HFpEF and HFrEF with early persistent AF who were randomised either to targeted therapy of underlying conditions plus rhythm control or routine rhythm control therapy . AAD treatment was instituted after recurrent AF and was effective in half of the patients at 1 year. Amiodarone was the most effective drug, but unfortunately, again limited by adverse effects. Ablation was performed only in a limited number of patients.
Overview of recent studies for the treatment of atrial fibrillation in the setting of heart failure
Recommended Reading: Congestive Heart Failure And Erectile Dysfunction
Ablate And Pace Strategy
There are a few small randomised clinical trials comparing pharmacological rate control and permanent pacing with complete AV node catheter ablation in patients with HF. These trials showed a benefit of an ablate and pace strategy in terms of symptom relief, HF hospitalisations and mortality . AV node ablation solves the problem of rapid ventricular response in AF, which aggravates symptoms and HF.
Catheter ablation of the AV node and permanent pacing should be considered if pharmacological rate control fails . The optimal choice of pacemaker type or pacing mode is still unclear.
Right ventricular or biventricular pacing is the next question which should be answered in the future. There are limited data suggesting an advantage of biventricular pacing versus right ventricular pacing in HF patients.
You May Like: How To Stop Worrying About Heart Attack
Atrioventricular Nodal Ablation And Pacemaker Placement
While the ablate and pace approach achieves rate control, it does not restore sinus rhythm and necessitates permanent implantation of a mechanical pacemaker. AV nodal ablation with biventricular pacing was compared to AF ablation in a pilot study of 35 subjects with CHF and systolic left ventricular dysfunction . In the Pulmonary Vein Isolation Versus AV Nodal Ablation With Biventricular Pacing for Patients With Atrial Fibrillation With Congestive Heart Failure study, pulmonary vein isolation was associated with greater improvement in symptoms and ejection fraction as compared with the ablate and biventricular pacing group.
Definitive trials assessing the effectiveness of AF ablation as compared with an ablate and ventricular pacing strategy are warranted. In the meantime, atrioventricular node ablation and ventricular pacing remains a reasonable option for the management of patients in whom the achievement of adequate rate control with pharmacologic therapy is inadequate .
Read Also: Is It Safe To Have Open Heart Surgery
What Causes Heart Failure
Although the risk of heart failure doesnt change as you get older, youre more likely to have heart failure when youre older.
Many medical conditions that damage the heart muscle can cause heart failure. Common conditions include:
- Tobacco and recreational drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
Treatments For Heart Failure
Treatment for heart failure usually aims to control the symptoms for as long as possible and slow down the progression of the condition.
How you’re treated will depend on what is causing your heart failure.
Common treatments include:
- lifestyle changes including eating a healthy diet, exercising regularly and stopping smoking
- medicine a range of medicines can help many people need to take 2 or 3 different types
- devices implanted in your chest these can help control your heart rhythm
- surgery such as a or a heart transplant
Treatment will usually be needed for life.
A cure may be possible when heart failure has a treatable cause. For example, if your heart valves are damaged, replacing or repairing them may cure the condition.
Recommended Reading: What Are The Types Of Heart Attacks
How Heart Failure Leads To Afib
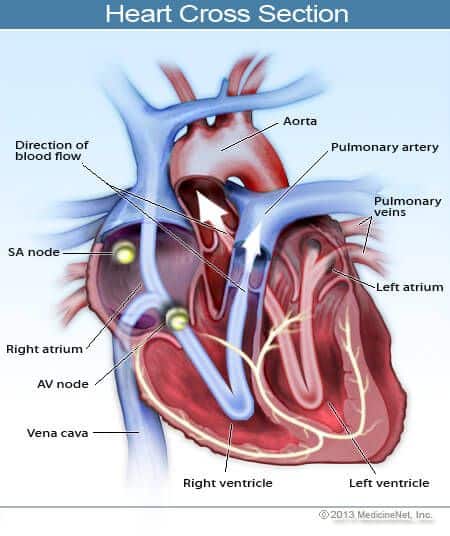
It works in the other direction, too. Your heart’s rhythm is controlled by electrical signals. For those signals to work well, they need healthy heart tissue.
But heart failure can actually stretch your atria and cause tissue in your heart to thicken and scar. Those changes throw off the electrical signals, and that messes up the heart’s rhythm and can cause AFib.
Mechanisms And Pathophysiology Of Atrial Fibrillation In Heart Failure
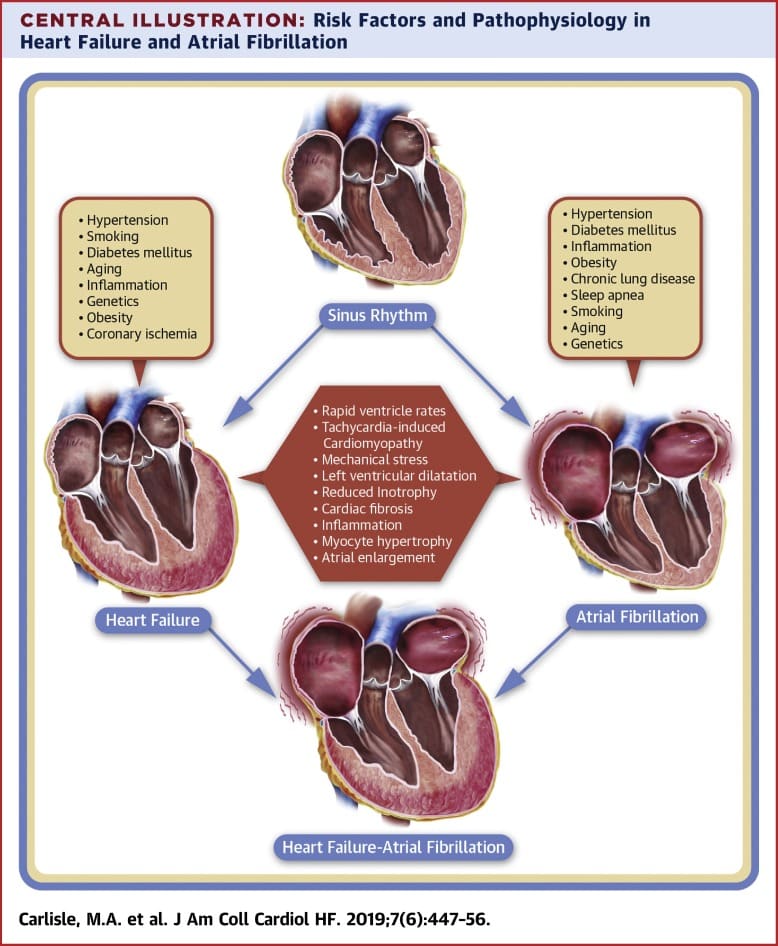
Heart failure and AF share risk factors and common pathophysiologic processes . Hypertension, smoking, obesity, diabetes, renal impairment, sleep apnoea, and coronary artery disease are all associated with an increased risk of developing both HF and AF.16 In HF, neurohormonal imbalance and activation of the reninangiotensinaldosterone system leads to maladaptive physiological changes including increased filling pressures and afterload. These can lead to increased left atrial stretch and fibrosis, contributing to the development of conduction abnormalities and facilitating the initiation and maintenance of AF.1721 The reninangiotensinaldosterone system also directly contributes to proarrhythmic remodelling, with angiotensin II causing atrial fibrosis and anisotropic conduction.22 Patients with HF also demonstrate altered calcium handling and calcium overload, which can lead to after-depolarizations and arrhythmia.23
You May Like: Does Eating Raise Heart Rate
You May Like: Recovery After Heart Surgery
Outlook For Heart Failure
Heart failure is a serious long-term condition that will usually continue to get slowly worse over time.
It can severely limit the activities youre able to do and is often eventually fatal.
But its very difficult to tell how the condition will progress on an individual basis.
Its very unpredictable. Lots of people remain stable for many years, while in some cases it may get worse quickly.
Pathophysiology Of Af In Chf
The pathophysiologic basis of AF is complex and incompletely understood . Initial mechanistic explanations for AF cited reentry as a principal factor . The multiple wavelet hypothesis, proposed by Moe and Abildskov, stated that the development of AF depended on the perpetuation of a sufficient number of randomly wandering wavelets created as a normal occurrence due to heterogeneous repolarization. The hypothesis maintained that adequate atrial mass, short refractory periods, and conduction velocities slow enough to permit temporal disparities in depolarization and repolarization in the atria favored the development of these reentrant wavelets.
This argument is predicated on the concept that the wavelength of an electrical signal also represents the minimal pathway length that must be present to sustain a reentrant circuit. If a pathway is shorter, then a reentrant electrical stimulus will encounter refractory tissue upon completing the circuit and terminate. In contrast, if the pathway is longer then the electrical signal may encounter excitable tissue upon completing the circuit, thereby perpetuating the previous cycle. The wavelength, and thus the pathway length, is proportional to both the refractory period of the tissue, as well as the conduction velocity. This model explains precipitants of AF that shorten the atrial effective refractory period or decrease conduction velocity.
Mechanisms promoting atrial fibrillation in congestive heart failure.
You May Like: How To Reduce Your Heart Rate
Rationale For Rhythm Control In Atrial Fibrillation And Heart Failure
What is the optimal management of this subset of patients who have concomitant heart failure and atrial fibrillation, and what is the rationale? The loss of atrial transport and an irregular ventricular rhythm both make important contributions to the worsening of cardiac output and other hemodynamic parameters. The subsequent hemodynamic changes may then explain the clinical alterations that are observed in this population.
The clinical and hemodynamic consequences of developing atrial
Af And Chf: Therapeutic Approaches
Rate or rhythm control
In a substudy of Danish Investigations of dysrhythmia and mortality on Dofetilide trial and in CHF-STAT the subgroup of heart failure patients who maintained sinus rhythm demonstrated reduced mortality., The Atrial Fibrillation in Congestive Heart Failure trial, a large multicenter prospective randomized trial, involving 1,376 patients which assessed cardiovascular mortality among patients with concomitant AF and CHF treated with a rate or rhythm control strategy, did not describe any morbidity or mortality benefit or any improvement in secondary outcome of rhythm over rate control. SWORD , a trial of d-sotalol in patients with LVEF â¤40% post myocardial infarction demonstrated increased mortality with d-sotalol use compared with placebo. SWORD was not a trial looking specifically at AF patients, but does raise concern about the use of this class of antiarrhythmic drugs in patients with CHF post myocardial infarction.
Antiarrhythmic therapy
Class I agents: sodium channel blockers
These are commonly used for patients with structurally normal hearts and AF but avoided in patients with CHF and ischemic heart disease as they may increase mortality.
Class III agents: potassium channel blockers
Rate control
Other drug therapies
Anticoagulation
Don’t Miss: How To Measure Heart Rate Variability
Specific Implications In Chf
Thus it is clear that electrical triggers, susceptible substrate, and modulating factors are important for the promotion of AF. Genetic factors may promote AF by increasing susceptibility to reentry, triggered activity, disrupting cell-to-cell communication, and through other currently as yet undefined mechanisms. Several of the discussed pathophysiological mechanisms are of particular importance in patients with CHF .
Elevations in left atrial and pulmonary venous pressure present in CHF promote AF as well. Myocyte stretch increases firing from ectopic foci such as the pulmonary veins through mechanoelectrical feedback . Additionally, increased fibrosis results from myocyte stretch. Gross evidence of structural remodeling includes left atrial enlargement, which predisposes to AF . Although increased atrial refractoriness has been observed clinically in patients with CHF, shortening of the atrial refractory period has been reported in experimental models of left atrial stretch, suggesting that many competing processes may be occurring simultaneously in these patients .
Atrial Fibrillation And Congestive Heart Failure
DOI: 10.19102/icrm.2011.020404
1Department of Internal Medicine, Charlton Memorial Hospital, Fall River, MA2Cardiac Arrhythmia Service, Massachusetts General Hospital, Boston, MA
ABSTRACT.Atrial fibrillation and congestive heart failure are common conditions which predispose each other, share risk factors, and are associated with morbidity and mortality. They share common pathophysiology, including structural and electrical remodeling, intracellular calcium dysregulation, and neuroendocrine mechanisms, and also have genetic basis. Despite better survival in patients with sinus rhythm than those with AF, rhythm control has not been found to be superior to rate control. The role of non-antiarrhythimc therapy is also being explored. Catheter ablation and device-based therapy with pacemaker and cardiac resynchronization therapy may also benefit patients with AF and CHF.
KEYWORDS.ablation, antiarrythmic drugs, atrial fibrillation, genetics, heart failure.
The authors report no conflicts of interest for the published content. Manuscript received February 13, 2011, final version accepted March 3, 2011.
Address correspondence to: E. Kevin Heist, MD, PhD, Cardiac Arrhythmia Service, 55 Fruit Street, Massachusetts General Hospital, Boston, MA. E-mail:
Also Check: Does Dopamine Increase Heart Rate
Prevention Of Atrial Fibrillation In Heart Failure
In the Framingham study, 41% of patients with AF and HF developed HF first, 38% developed AF first, and in the remaining 21% AF and HF occurred at the same time. While there are no therapies proven to prevent the risk of incident HF in patients with established AF, the treatment of modifiable CV risk factors , effective rate control and the diagnosis and treatment of associated comorbidities would seem to be sensible interventions.
What about preventing AF in patients with known HF? Meta-analysis of RCTs suggests that angiotensin converting enzyme inhibitors and angiotensin receptor blockers reduce the risk of incident AF, with RR of 0.79 and 0.78 , respectively. Data from the Candesartan in Heart failure-Assessment of Reduction in Mortality and morbidity program show that ARBs can decrease the risk of new-onset AF in patients with HFrEF and HFpEF. In the -blocker vs. placebo trials in HFrEF with baseline sinus rhythm, allocation to -blockers was associated with a significant reduction in the adjusted odds of incident AF . In a small analysis pointing towards the potential benefits of personalized therapy in patients with HF and AF, HF patients who were homozygotes for 1 adrenergic receptor 389 Arginine had a 74% reduction in new-onset AF when treated with bucindolol vs. placebo.
Will Atrial Fibrillation Make My Life Harder
You might find it harder when getting used to a new routine. AF is a manageable condition and with the right treatment you can carry on as you were before you were diagnosed.
Talking to people about your condition can be hard. Dealing with stress and anxiety is also common after being told you have a heart condition. Visit our emotional support hub for advice and support if youre struggling with the change of pace.
You might have to think about practical matters, like driving, going on holiday or travel insurance after being diagnosed with AF. Again, your GP can help with any queries you might have.
Read Also: Which Arm Hurts With Heart Attack
