Enhancing Healthcare Team Outcomes
The treatment of heart failure and acute decompensated heart failure is challenging despite the use of maximal evidence-based therapy based on the stage of heart failure. Given the limited effect that current treatment strategies have on the progression of heart failure, it is important to identify ways to maximize patient outcomes and quality of care by the interprofessional team.
Patients at potential risk for heart failure based on comorbidities or other identified risk factors should receive appropriate evidence-based preventative counseling and treatments. When appropriate, the primary care providers who may be the most involved in the management of the patients’ risk factors should consult other specialists, including cardiologists, endocrinologists, pharmacists, cardiology nurses, and nutritionists, to ensure that they are providing the best advice and treatment for their patients. Nurses monitor patients, provide education, and collaborate with the physicians and the rest of the team to improve outcomes. Pharmacists review medications, inform patients and their families about side effects and monitor compliance.
Given the propensity of heart failure patients to require re-current admissions, often because of non-heart failure related conditions, the collaboration between inpatient and outpatient services can be of benefit in the continuity of care and helping promote improved outcomes.
How Can I Reduce My Risk
Since cardiogenic pulmonary edema happens when you already have a problem with your heart, the best way to reduce your risk is by keeping your heart strong and healthy.
Ways to do that include:
- Eating foods that are low in saturated fats and trans fats.
- Exercising every day.
- Limiting how much alcohol you drink.
Cpap In Cardiogenic Pulmonary Oedema
- CPAP can be considered in patients who have not responded to medical treatment. However, discuss this option with a senior.
- CPAP increases intrathoracic pressure, which reduces preload by decreasing venous return.
- CPAP lowers afterload by increasing the pressure gradient between the left ventricle and the extrathoracic arteries, which may contribute to the associated increase in stroke volume.
- Intubation should be considered in patients with persistent hypoxaemia on CPAP or persistent hypercapnia despite the administration of oxygen, morphine, diuretics, and vasodilators. In addition, intubation is required in the setting of apnoea or profound respiratory depression .
Recommended Reading: How Does Dehydration Affect Heart Rate
What Are The Causes Of Congestive Heart Failure
Many medical conditions could weaken or damage the heart. They are as mentioned below:
-
Coronary Artery Disease: The arteries supplying the heart may become obstructed entirely or partially, resulting in depletion of oxygen-rich blood to the heart, causing extensive damage to the heart muscles.
-
Heart Attack: When the blood flow to the heart is completely obliterated, it results in a heart attack. A heart attack could also result in scar tissue, thus compromising its function.
-
Cardiomyopathy: It is an acquired or hereditary disorder affecting the heart muscles. It could be due to drug abuse, alcohol consumption, or certain infections.
-
Valvular Disease: The heart has few valves that check the inflow and outflow of blood. Damage to these valves could strain the heart and weaken it.
-
Myocarditis: Inflammation of the muscles of the heart is myocarditis. It is usually caused by a viral infection such as the COVID-19 virus.
-
Congenital Heart Defects: Congenital heart defects refers to heart diseases that are present from birth. If not treated early, they could also result in congestive heart failure.
-
Arrhythmias: Abnormal heartbeat could result in the irregular working of the heart, thus weakening it over time.
-
Risk Factors: Certain risk factors associated with heart failure are diabetes, hypertension, high cholesterol, smoking, alcohol abuse, obesity, and certain medications.
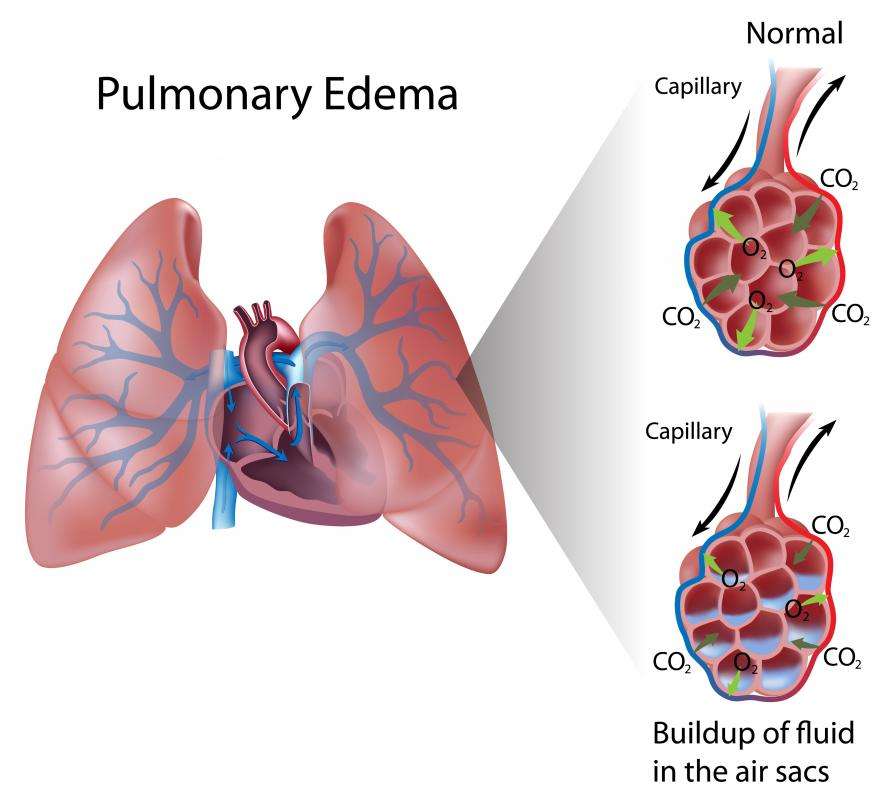
Why Pulmonary Edema Is A Problem
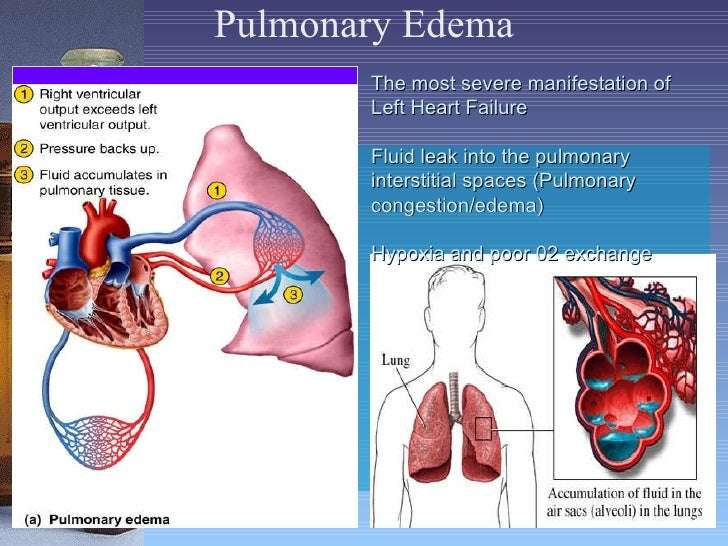
Pulmonary edema is a serious medical condition that happens when excess fluid begins to fill the lungs’ air sacs . When the alveoli are filled with fluid, they cannot adequately add oxygen to, or remove carbon dioxide from, the blood. So pulmonary edema produces significant breathing difficulties, and may often become a life-threatening problem.
Don’t Miss: How To Reduce Your Heart Rate
Definitions In Pulmonary Oedema
- Acute pulmonary oedema: Accumulation of fluid in the lung parenchyma leading to impaired gas exchange between the air in the alveoli and pulmonary capillaries.
- Cardiac failure: clinical syndrome where the heart is unable to function adequately as a pump to meet the demands of the body characterised by:
- Typical symptoms, including dyspnoea, orthopnoea, ankle swelling
- Typical signs, including bibasal crepitations, raised jugular venous pressure
- Objective evidence of a structural or functional abnormality including cardiomegaly, third heart sound, abnormality on echocardiogram
Pulmonary Edema Or Plural Effusion
Pulmonary edema happens when fluid collects inside the lungs, in the alveoli, making it hard to breathe. Plural effusion also involves fluid in the lung area, and it is sometimes called water on the lungs.
However, in pleural effusion, water fluid collects in the layers of the pleura that are ouside the lungs. It can result from heart failure, cirrhosis, or a pulmonary embolism. It can also occur after heart surgery.
Recommended Reading: Fitbit Heart Rate Monitor How Does It Work
Deterrence And Patient Education
Effective treatment of comorbidities and risk factor reduction can decrease the chance of developing heart failure. Patient education should be focused on ensuring compliance with prescribed evidence-based treatments.
- Hypertension – effective treatment of systolic and diastolic hypertension can reduce the risk of heart failure by approximately 50%
- Diabetes – is directly associated with the development of heart failure, independent of other associated clinical conditions
- Alcohol – heavy alcohol use is associated with heart failure
- Metabolic syndromes – important to keep up treatment based on evidence-based guidelines to decrease the risk of heart failure
- Patient education regarding dietary salt restriction and fluid restriction is imperative
What Is Cardiogenic Pulmonary Edema
Cardiogenic pulmonary edema is an accumulation of extra fluid in your lungs that can be life-threatening. This comes from pressure going up and blood collecting on the left side of your heart, usually because of heart failure. In addition to difficulty breathing, cardiac edema can lead to organ damage from a lack of enough oxygen.
Cardiac edema vs. pulmonary edema
Both of these mean you have too much fluid in your lungs, which makes it hard for you to breathe. Cardiogenic pulmonary edema is a type of pulmonary edema with a heart problem as its cause. An injury to your lungs causes the non-cardiogenic type of pulmonary edema.
Cardiac edema vs. renal edema
These are both names for excess fluid in your organs. With cardiac edema, theres too much fluid in your lungs. With renal edema, theres too much fluid in your kidneys. Heart failure can cause both of these. Also, your kidneys cant get enough fluid out of your blood and into your pee.
Read Also: How To Stop Heart Palpitations From Anxiety
Cardiac Disorders Manifesting As Cpe
Atrial outflow obstruction
This can be due to mitral stenosis or, in rare cases, atrial myxoma, thrombosis of a prosthetic valve, or a congenital membrane in the left atrium . Mitral stenosis is usually a result of rheumatic fever, after which it may gradually cause pulmonary edema. Other causes of CPE often accompany mitral stenosis in acute CPE an example is decreased LV filling because of tachycardia in arrhythmia or fever.
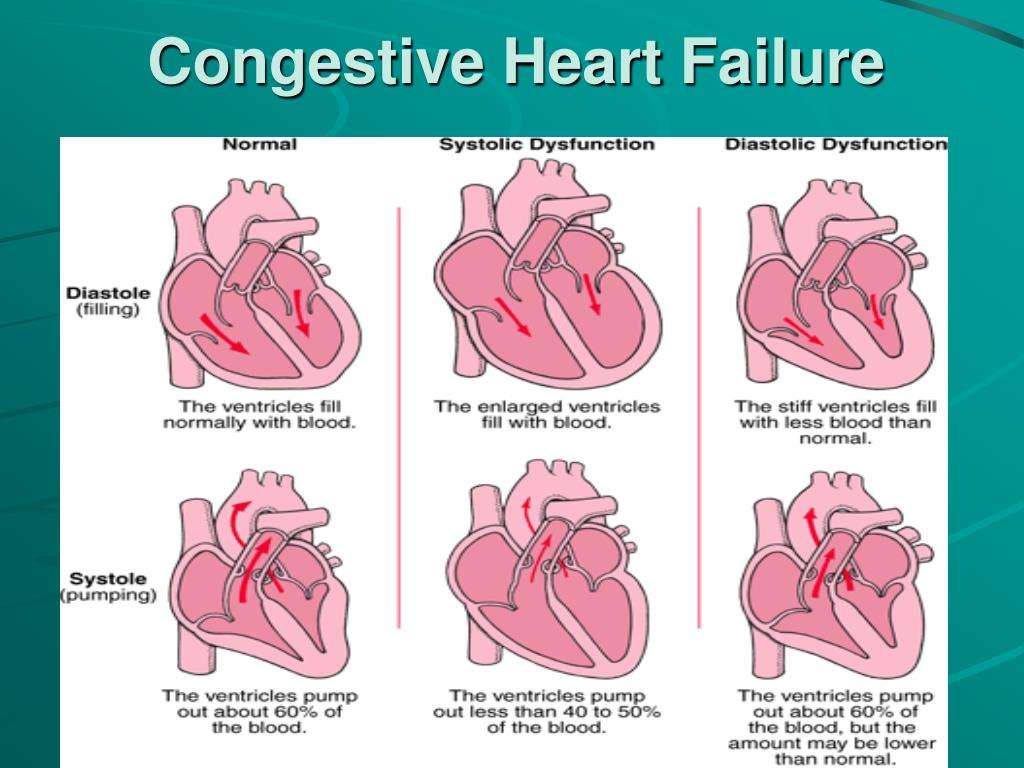
LV systolic dysfunction
Systolic dysfunction, a common cause of CPE, is defined as decreased myocardial contractility that reduces cardiac output. The fall in cardiac output stimulates sympathetic activity and blood volume expansion by activating the renin-angiotensin-aldosterone system, which causes deterioration by decreasing LV filling time and increasing capillary hydrostatic pressure.
Chronic LV failure is usually the result of congestive heart failure or cardiomyopathy. Causes of acute exacerbations include the following:
-
Acute myocardial infarction or ischemia
-
Patient noncompliance with dietary restrictions
-
Patient noncompliance with medications
-
Severe anemia
-
Myocardial toxins
-
Chronic valvular disease, aortic stenosis, aortic regurgitation, and mitral regurgitation
LV diastolic dysfunction
Ischemia and infarction may cause LV diastolic dysfunction in addition to systolic dysfunction. With a similar mechanism, myocardial contusion induces systolic or diastolic dysfunction.
How Is Pulmonary Oedema Treated
People with sudden onset of pulmonary oedema usually need urgent admission to hospital. They require treatment with oxygen , medicines to remove the excess fluid from the lungs and other medicines to help the heart work more effectively. These medicines are usually given through the veins .
Further treatment will depend on the cause of the pulmonary oedema. See also the separate leaflet called Congestive Heart Failure.
Urgent treatment is also needed for the cause of the pulmonary oedema, such as treatment for a heart attack, high-altitude sickness or acute kidney injury.
If oxygen and medicines do not successfully treat the pulmonary oedema, it may be necessary to use a ventilator or other methods to help with breathing until the pulmonary oedema is improving.
Recommended Reading: Increased Resting Heart Rate
What Are The Ways To Diagnose Congestive Heart Failure
Various tests can be used to diagnose the health of the heart. They are described below:
-
Physical Examination and History of the Patient: A detailed physical examination, medical history, family history, and personal history could help ascertain the risk factors and the predisposition for heart failure.
-
Blood Test: Blood tests can determine any risk factors that adversely affect the heart. High serum cholesterol levels could result in blocked coronary arteries. Another blood marker for heart failure is B-type natriuretic peptide . When heart failure occurs, there is a change in blood pressure which prompts the heart to release BNP.
-
Radiological Imaging: Various radiological imaging tests such as X-rays, electrocardiograms, computed tomography , and magnetic resonance imaging are also used to diagnose heart failure.
Pulmonary Edema Or Pneumonia
Pulmonary edema can overlap with pneumonia, but it is a different condition. Pneumonia is an infection that often occurs as a complication of a respiratory infection, such as the flu.
It can be difficult to distinguish between the two. If the individual or a family member can provide a detailed medical history, this will make it easier for a physician to make the correct diagnosis and provide the right treatment.
The patient will undergo a physical exam first. The doctor will use a stethoscope to listen to the lungs for crackles and rapid breathing, and the heart for abnormal rhythms.
Blood tests will be carried out to determine blood oxygen levels the doctor will often order other blood tests, including:
- electrolyte levels
- liver function
- blood counts and blood markers of heart failure
An ultrasound of the heart, an echocardiogram, and an electrocardiogram can help determine the condition of the heart.
A chest X-ray may be used to see whether there is any fluid in or around the lungs and to check the size of the heart. A CT scan of the chest may also be ordered.
Read Also: With Respect To Heart Rate, Which Of The Following Worked In Opposition To Each Other
Dilatation Of Azygos Vein
Dilation of the azygos vein is a sign of increased right atrial pressure and is usually seen when there is also an increase in the width of the vascular pedicle.The diameter of the azygos vein varies according to the positioning.In the standing position a diameter > 7 mm is most likely abnormal and a diameter > 10 mm is definitely abnormal.In a supine patient > 15 mm is abnormal. An increase of 3 mm in comparison to previous films is suggestive of fluid overload. The difference of the azygos diameter on an inspiration film compared to an expiration film is only 1mm. This means that the diameter of the azygos is a valuable tool whether or not there is good inspiration.
Pathophysiology Of Acute Pulmonary Oedema
- Blood pressure = cardiac output x systemic vascular resistance
- CO = heart rate x stroke volume
- SV depends on preload, myocardial contractility and afterload
- As the heart begins to fail, compensatory mechanisms maintain CO & BP
- Increased sympathetic tone increases SVR and stimulates renin secretion
- The renin-angiotensin-aldosterone system increases salt and fluid retention, which initially increases preload, end diastolic volume , SV and therefore CO via the Frank-Starling mechanism, but over time leads to cardiac dilatation and a reduction in contractility and CO, together with congestion of the pulmonary and systemic veins with associated tissue oedema
- As alveolar oedema increases, diffusion of oxygen into the pulmonary capillaries is impaired, which manifests as dyspnoea venous return to the already congested heart and lungs increases when the patient lies flat, which manifests as orthopnoea and paroxysmal nocturnal dyspnoea
- Acute pulmonary oedema can be precipitated by sudden increases in preload , decreases in contractility , increases in afterload or direct damage to the lungs themselves
Recommended Reading: What Happens If Your Heart Rate Is Too Low
Pulmonary Edema Vs Pleural Effusion
Sometimes pulmonary edema is confused with pleural effusion, another condition that involves fluid buildup in the lungs. However, pleural effusion specifically causes a buildup of fluids in the pleural tissues. These cover the outside of each of your lungs as well as the inside of the chest wall.
Pleural effusion can be caused by CHF, poor nutrition, and pneumonia. Its also sometimes cancerous .
With pleural effusion, you may experience:
- breathing difficulties
- shortness of breath
- chest pain and discomfort
A chest x-ray can help diagnose pleural effusion. Your doctor may take a biopsy from pleural tissues if cancer is suspected. Depending on the cause, pleural effusion may be treated with a combination of fluid removal techniques and surgery.
What Are The Radiological Findings Of Congestive Heart Failure
The radiological tests conducted and their findings are as mentioned below:
Chest X-Ray
A chest X-ray can be used to view both the heart and lungs. The chest X-ray can assess the size of the heart and the fluid accumulation in the lungs.
Based on the progression of CHF, 3 phases have been described, which are as follows:
– Phase 1: Vascular Phase
-
This represents the first phase of CHF and signifies pulmonary venous hypertension.
-
Cardiomegaly is evident.
-
Prominent upper pulmonary vessels, in contrast to lower blood vessels, are evident in healthy individuals.
-
Hilar level sees an increase in the artery to bronchus ratio, which appears as white round densities.
-
The pulmonary artery is more prominent in diameter than the bronchi .
-
Hilar haziness and fullness: Pulmonary veins are enlarged, and fluid is seen collecting around the vessels.
-
Vascular redistribution is not seen in supine X-rays .
– Phase 2: Interstitial Phase
-
Kerley lines .
-
They occur due to interstitial edema and amplified lymphatic drainage.
-
The bronchial wall thickening appears as a white rim around the bronchioles, which appear dark.
-
Thickening of the fissures between the lobes of the lungs.
– Phase 3: Alveolar Phase
Computed Tomography
-
CT is not generally recommended to diagnose heart failure. However, it can reveal any congenital or valvular diseases if present.
-
Thickening of the septal lines will be evident.
-
Ground-glass opacity appearance .
Magnetic Resonance Imaging
Stress Test
Coronary Angiogram
Don’t Miss: How To Calculate Your Maximum Heart Rate
Articles On Heart Failure Types & Stages
Congestive heart failure doesn’t mean your heart has stopped. It means it’s not pumping blood the way it should. When that happens, blood and fluid can back up in your body and make it harder for your kidneys to flush out sodium and water. That can make you hold on to too much fluid, which causes swelling.
There’s no cure. But your doctor may give you medication to do things like lower your blood pressure, relax your blood vessels, make your heart beat stronger, or ease swelling. And diet and lifestyle changes — like not smoking — can help, too.
What Can I Expect If I Have Cardiogenic Pulmonary Edema
Pulmonary edema is life-threatening, but your prognosis depends on what caused it. One year after discharge from a hospital, about 50% survive cardiac edema.
Heart failure, a common cause of cardiogenic pulmonary edema, is a chronic disease that can get better with treatment. Out of every three people whove been in the hospital because of heart failure, one person lives five or more years after their stay.
You May Like: Types Of Heart Surgeries
Pulmonary Edema Vs Pneumonia
Pneumonia is another serious condition of the lungs. Unlike edema, pneumonia is caused by either a viral, fungal, or bacterial infection. As your lungs become infected, fluid builds up in the air sacs .
While both pulmonary edema and pneumonia cause a form of buildup in the lungs, the former is primarily caused by CHF. Pneumonia, on the other hand, is caused by an infection. A weakened immune system can increase your chances of getting pneumonia from a common cold or flu.
Symptoms of pneumonia may include:
- high fever with chills
- cough with mucus that continues to worsen
- chest pain and discomfort
Treatment Of Pulmonary Edema
Pulmonary edema is a serious condition that requires quick treatment. Oxygen is always the first line of treatment for this condition. Your healthcare team may prop you up and deliver 100 percent oxygen through an oxygen mask, nasal cannula, or positive pressure mask.
Your doctor will also diagnose the cause of pulmonary edema and prescribe the appropriate treatment for the underlying cause.
Depending on your condition and the cause of your pulmonary edema, your doctor may also give:
- Preload reducers. These help decrease pressures from the fluid going into your heart and lungs. Diuretics also help reduce this pressure by making you urinate, which eliminates fluid.
- Afterload reducers. These medications dilate your blood vessels and take pressure off your heart.
- Heart medications. These will control your pulse, reduce high blood pressure, and relieve pressure in arteries and veins.
- Morphine. This narcotic is used to relieve anxiety and shortness of breath. But fewer doctors today use morphine due to the risks.
In severe cases, people with pulmonary edema may need intensive or critical care.
In other cases of pulmonary edema, you may need treatment to help you breathe. A machine will deliver oxygen under pressure to help get more air into your lungs. Sometimes this can be done with a mask or cannula, also called Continuous Positive Airway Pressure .
Your doctor may need to insert an endotracheal tube, or breathing tube, down your throat and use mechanical ventilation.
Read Also: How Do You Calculate Your Heart Rate
