Atrial Natriuretic Peptide And B
ANP and BNP are endogenously generated peptides activated in response to atrial and ventricular volume/pressure expansion. ANP and BNP are released from the atria and ventricles, respectively, and both promote vasodilation and natriuresis. Their hemodynamic effects are mediated by decreases in ventricular filling pressures, owing to reductions in cardiac preload and afterload. BNP, in particular, produces selective afferent arteriolar vasodilation and inhibits sodium reabsorption in the proximal convoluted tubule. It also inhibits renin and aldosterone release and, therefore, adrenergic activation. ANP and BNP are elevated in chronic heart failure. BNP especially has potentially important diagnostic, therapeutic, and prognostic implications.
For more information, see the Medscape Drugs & Diseases article Natriuretic Peptides in Congestive Heart Failure.
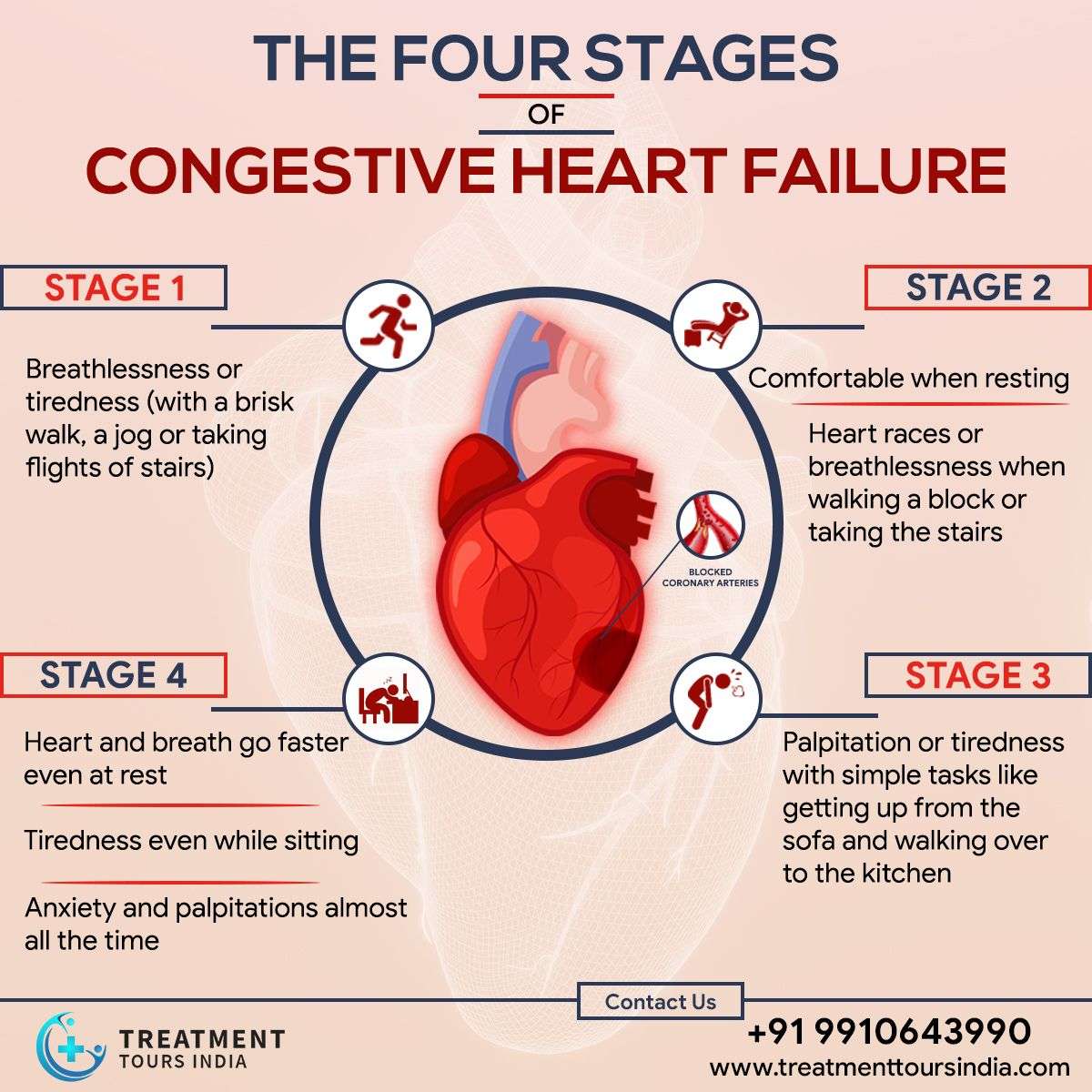
What Are The 4 Stages Of Heart Failure
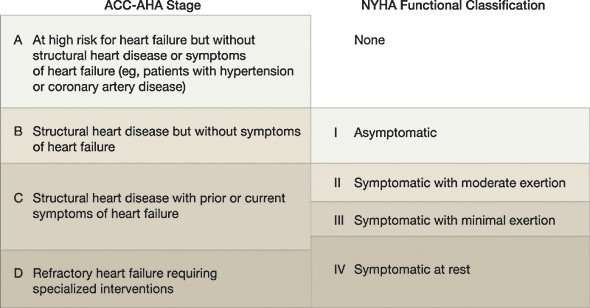
There are four stages of heart failure – stage A, B, C and D – which range from high risk of developing heart failure to advanced heart failure.
The four stages of heart failure are different to the four classes of heart failure symptoms also described in New York Heart Association , which illustrates the severity of symptoms, ranging from class one to the most severe, which is class four .
What Are The Signs And Symptoms Of Congestive Heart Failure
Difficulty breathing or shortness of breath are the most common and distinctive symptoms of congestive heart failure.
- Difficulty breathing may occur when a patient is at rest, during an activity, while lying flat, or even while waking up.
- Chest pain is another common symptom seen in patients with congestive heart failure.
- Due to water retention in the kidneys, patients will have a fluid overload in ankles, feet, stomach, and lungs, which is another key symptom seen in heart failure patients.
You May Like: Is 85 Heart Rate Normal
What Happens Before This Procedure
Because there are far more people who need hearts than donors, there’s a strict selection process that you have to undergo to receive a heart transplant. The goal of this process is to select recipients who have the best chance of long-term survival based on their overall health.
After a healthcare provider refers you to a transplant program, youll undergo the following.
Medical evaluation
To ensure that donor hearts go to people with the best chance of survival, healthcare providers will evaluate your overall health by running several different tests. Some, but not all, of the possible tests are listed below.
Lab tests will include tests on your blood, urine and other screenings. These tests will look for the following:
- Blood composition. This analyzes your bloods levels of red blood cells, platelets, and more. These tests will also analyze your blood chemistry, looking for signs of other conditions that might affect your ability to undergo a heart transplant.
- Immune system analysis. These tests help providers anticipate how well your immune system can tolerate a donor organ.
- Kidney function. These tests analyze your urine to see how well your kidneys are working.
- Tests for alcohol, tobacco and drugs. These are often important tests if you have a history of using recreational drugs or drinking too much alcohol. Most transplant centers require that youre sober and avoid using tobacco products and recreational drugs for an extended time before your transplant.
End Stages Of Heart Failure: What To Expect
Congestive heart failure is one of the most common reasons for hospital admissions for senior citizens. In fact, over 5 million adults in the United States experience heart failure.
Heart failure occurs when the heart muscle becomes damaged and can no longer pump blood effectively. Although symptoms can be managed, this is a chronic condition with no cure. In time, patients will reach the final stages of congestive heart failure.
Patients in the end stages of heart failure want to know what to expect. The symptoms of end-stage congestive heart failure include dyspnea, chronic cough or wheezing, edema, nausea or lack of appetite, a high heart rate, and confusion or impaired thinking.
Read Also: How Long Do Heart Attack Enzymes Stay In Blood
What Happens After This Procedure
After your heart transplant, the following will need to happen.
Immune system suppression
After the procedure, providers will start you on medications that will suppress your immune system. They do that because your immune systems normal reaction to a foreign object is to treat it like an infection or other harmful invader and attack it. That suppression protects the new heart from attack by your own immune system.
Providers will continue to monitor your condition and vital signs closely. They do that to watch for any signs that your body is rejecting the new heart . Youll also need to take those medications for the rest of your life.
Nervous system reconnection
Providers will also monitor the new heart’s electrical function. That’s necessary because the donor’s heart doesn’t connect to your nervous system. Fortunately, your heart can still manage how fast it beats in other ways. Your resting heart rate will usually stay at the high end of normal or slightly higher .
In many people, the heart recipient’s nervous system can form new connections with the donor’s heart. The sympathetic nervous system connections, which control your fight-or-flight response and speed up your heart, form after about six months. The parasympathetic nervous system connections, which help your heart slow down and relax, form after about 18 months to two years. In some cases, this reconnection doesnt happen, but this isnt usually the case.
Follow-up care
Congestive Heart Failure Symptoms
Signs of heart failure can appear in anyone at any age, even in young children that may be born with heart defects. But it usually affects older people with weakened hearts from other diseases.
There may be no symptoms in the early stages, but people start having symptoms in stage II and they get progressively worse, especially without treatment.
Symptoms include:
- Feelings of anxiety, suffocation and restlessness
- Hacking, dry cough that happens more often when lying down
- Having to urinate more often at night
- Lung congestion and difficulty breathing from blood backing up into the lungs
- Nausea, abdominal swelling, tenderness or pain
- Swelling from fluid buildup, especially in the feet, ankles and legs
- Weight gain from fluid buildup or weight loss from poor nutrient absorption and decreased appetite
Also Check: Does Alcohol Increase Your Heart Rate
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the “Stages of Heart Failure.” These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
Read Also: Why Is My Resting Heart Rate Going Up
How Is Congestive Heart Failure Diagnosed
Heart failure is diagnosed with a physical exam and tests that may include:
- Electrocardiogram to measure the electrical activity in the heart
- Brain natriuretic peptide or N-terminal pro-BNP blood tests
- BNP or NT-proBNP level is high in people with heart failure
What Is The Prognosis For Children With Congenital Heart Defects
The prognosis depends on the defect. In many cases, children with congenital heart defects go on to live normal lives. In most cases, people with heart defects are at greater risk for developing infection of the heart and valves. They may need to take antibiotics when having certain dental or surgical procedures in order to prevent endocarditis, an infection of the hearts lining.
Recommended Reading: Chest Pain Low Heart Rate
What Are The Advantages And Disadvantages Of This Procedure
The biggest advantage of heart transplantation is that its a life-saving option when other options didnt work, were too risky to use, or were unlikely to help.
The biggest disadvantages of heart transplant are:
- More people need a heart transplant than there are available donor hearts.
- Its an extremely complicated surgery, limiting it to only the most well-equipped and best-staffed hospitals.
- Some people may be too ill to survive the procedure.
- The procedure has several potential risks and complications .
What are the risks or complications of this procedure?
The most common risks and complications of heart transplant include the following:
- Organ rejection.
- Infections .
- Graft failure .
Congestive Heart Failure In Dogs
Written bySmall Door’s medical experts
Congestive heart failure is fairly common in dogs. Approximately 10% of all dogs, and 75% of senior dogs, have some form of heart disease. CHF itself is not a disease: it is a condition that is a result of heart disease.
In This Article
Read Also: Survival Rate Of Heart Attacks By Age
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
Side Effect: Leg Crampsconceivable Reason: Dehydration
A spasm in your leg after youve been working out, particularly in the hotness, could be a significant sign that your body is coming up short on liquids.
To contract and unwind ordinarily, muscles depend on water and electrolytes like sodium and potassium.
Excessively minimal liquid or electrolytes can hypersensitize the nerves that manage muscle tissues withinside the legs, inflicting the muscle tissues to agree abnormally or spasm.
Each of your organs depends on liquids to working typically.
Parchedness keeps cells from appropriately utilizing energy, shipping supplements, and isolating.
Also Read: Pulsatile tinnitus when lying down
If not immediately cured, it can turn into a hazardous condition.
To try not to get too coming up short on liquids, drink water or an electrolyte-containing sports drink previously, during, and after a workout.
Don’t Miss: What Does Heart Attack Look Like On Ekg
Supporting Those Around The Patient
Those close to the patient may also need emotional and practical support. They may need:
- information about heart failure to help them understand the symptoms and treatment options
- support if they’re caring for the patient
- time to relax or look after their own health.
If the patient’s heart failure is due to an inherited heart condition, their family may have concerns about their own health. Talk to them about their worries. It might be appropriate to refer immediate family members to a clinic which specialises in inherited heart conditions. This may have been done when the patient was first diagnosed.
Inherited heart conditions services offer specialist assessment and investigations, genetic counselling and testing. GPs can refer to this service.
How To Improve Your Quality Of Life
There are a number of approaches to improve your quality of life, including getting more moderate-intensity exercise and managing stress.
Eating a heart-healthy diet thats low in trans fats and high in whole grains is also good for slowing down CHF, according to Medical News Today. You should also be sure to get your blood pressure checked during routine check-ups at the doctor or get an at-home blood pressure monitor to check it yourself regularly.
Also Check: How To Fight Heart Disease
Myocytes And Myocardial Remodeling
In the failing heart, increased myocardial volume is characterized by larger myocytes approaching the end of their life cycle. As more myocytes drop out, an increased load is placed on the remaining myocardium, and this unfavorable environment is transmitted to the progenitor cells responsible for replacing lost myocytes.
Progenitor cells become progressively less effective as the underlying pathologic process worsens and myocardial failure accelerates. These featuresnamely, the increased myocardial volume and mass, along with a net loss of myocytesare the hallmark of myocardial remodeling. This remodeling process leads to early adaptive mechanisms, such as augmentation of stroke volume and decreased wall stress and, later, to maladaptive mechanisms such as increased myocardial oxygen demand, myocardial ischemia, impaired contractility, and arrhythmogenesis.
As heart failure advances, there is a relative decline in the counterregulatory effects of endogenous vasodilators, including nitric oxide , prostaglandins , bradykinin , atrial natriuretic peptide , and B-type natriuretic peptide . This decline occurs simultaneously with the increase in vasoconstrictor substances from the RAAS and the adrenergic system, which fosters further increases in vasoconstriction and thus preload and afterload. This results in cellular proliferation, adverse myocardial remodeling, and antinatriuresis, with total body fluid excess and worsening of heart failure symptoms.
When Should I See My Healthcare Provider
Your healthcare provider will set up a schedule of visits after your procedure, especially within the first three months. Those visits are critical to making sure you are recovering and arent experiencing any complications or problems related to your new heart.
Your provider will also tell you what signs and symptoms to watch for that mean you need emergency medical attention. Most commonly, the signs and symptoms involve the rejection of your new heart or infections. These symptoms include:
- Fever.
- Drainage or oozing from the incision in your chest.
- Redness or warmth around the incision.
- If your breastbone moves, shifts or causes any kind of cracking or popping sound/feeling when you move.
Your healthcare provider will also recommend and help you do the following:
- Make sure you get preventive dental care .
- Stay current on all your vaccinations .
- Get routine health screenings as needed .
A note from Cleveland Clinic
Don’t Miss: Is Aspirin Good For Heart Palpitations
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
