Implantation Techniques And Difficulties
The major problem with applying this mode of therapy has been access to, and maintenance of, effective left ventricular pacing. Epicardial leads had been used initially, but the practical approach of inserting the left ventricular lead via the coronary sinus tributaries has since been adopted.4, 5, 55, 56 A new method to the epicardial approach via robotic-enhanced thoracoscopic implantation of the left ventricular lead has been proposed recently.57 A transseptal approach to endocardial left
Your Beat Monitored Remotely
There are more ways to allow you to live life to the fullest. Remote monitoring of your Abbott implanted CRT heart device may help you do just that, and it gives you and your doctor the feeling of safety and security of continuous monitoring of your heart from the time of implant to the time you are at home.
With remote monitoring, your CRT device is able to communicate to your doctor’s office or clinic without you having to go in for an in-person visit. Your doctor may schedule your in-person visits less frequently, based on the data they receive from your device.
After your CRT device is implanted, you will use either a transmitter or downloadable mobile app to transmit information to your doctor.
Indications, Safety & Warnings
Rx Only
Brief Summary: Prior to using these devices, please review the Users Manual for a complete listing of indications, contraindications, warnings, precautions, potential adverse events and directions for use.
Refer to the Users Manual for detailed indications, contraindications, warnings, precautions and potential adverse events.
MAT-2115398 v1.0
Predictors Of Response To Cardiac Resynchronization Therapy
Cardiac resynchronization is indicated in patients with heart failure, systolic dysfunction, and prolonged QRS interval since it could decrease mortality in this group of patients. Unfortunately, up to 40% do not experience clinical improvement to this therapy. Table 1 shows the probable causes of this absence of response.
|
Read Also: Under Resting Conditions, Heart Rate Is Primarily Under The Control Of What Control System
How Do I Get Ready For The Insertion Of A Crt Device
You should discuss all the risks and benefits of the procedure with your doctor. He or she will probably tell you to not eat or drink anything after the midnight before surgery. If you usually take medicines in the morning, ask your doctor if you can take them with a sip of water.
Your healthcare team may ask you to stop taking any medicines that thin your blood several days before the procedure. If you take medicines for diabetes, ask your doctor to help you adjust your dose around your surgery. Let your doctor know about:
- Prescription medicines that you take
- Over-the-counter medicines or supplements you take, especially aspirin
- Recent symptoms of colds or infections
- History of problems with anesthesia
Candidates Selection: Keep An Eye On Pr Interval
PR prolongation alters normal AV mechanical coupling reducing LV filling, stroke volume and resulting in diastolic mitral regurgitation. Dual-chamber pacing acutely improves haemodynamics restoring AV coupling but it failed to demonstrate improved long-term outcomes probably due to the detrimental effects of ventricular desynchronization. Therefore, patients with longer AV delay would be more likely to respond positively to CRT as it was described by a post hoc analysis of the COMPANION study.
However, other studies have found that a prolonged PR interval seems to be a marker of atrial and structural remodelling and it is associated with more severe HF disease., The CARE-HF trial described worse outcomes in patients with prolonged PR interval regardless of the treatment arm . In a recent study comparing patients with CRT, a baseline PR prolongation is an independent predictor of worse prognosis and lower probability of reverse remodelling, especially for patients with non-LBBB morphology.
Recommended Reading: How Does Fitbit Calculate Resting Heart Rate
Iatrogenic Dyssynchrony Caused By Right Ventricular Apical Pacing And Alternate Sites Of Pacing
Another important point to consider is the accumulating evidence that not only is spontaneous left bundle branch block harmful to our patients, but the iatrogenic left bundle branch block produced by right ventricular apical pacing is equally deleterious. In a study involving 24 young patients in need of permanent pacing compared with 33 age- and basal surface area-matched healthy control individuals over a mean follow-up of 9.5 years, right ventricular apical pacing led
Can Cardiac Resynchronization Therapy Cure Heart Failure
While CRT can help many people with heart failure resume some of their usual activities and improve their quality of life, it is not a cure. Though you can often manage heart failure, it cannot be cured.
Its worth noting that CRT is usually just one component of heart failure treatment. If you have heart failure, you may also be prescribed anti-hypertensive medications to lower blood pressure, including beta blockers, which slow the heart rate and ease the burden on the heart muscle.
Other medications you may be prescribed include digoxin , which strengthens heart contractions. And, if you have high cholesterol, you may need to take a statin to lower your LDL cholesterol levels.
Depending on the cause, heart failure may be treated with other procedures. For instance, if you have valve disease, surgery or catheter-based procedures to replace or repair a valve may improve your symptoms.
You May Like: Do Antibiotics Increase Heart Rate
Candidatess Selection: Right Ventricular Apical Pacing For Bradycardia And Heart Failure
In the last decade, increasing evidences showed that conventional right ventricular apical pacing might have detrimental effects on cardiac structure and LV function, possibly leading to the development of HF.
In the PREventing VENTricular Dysfunction in Pacemaker Patients Without Advanced Heart Failure trial and in the biventricular vs. right ventricular pacing in patients with atrioventricular block trial, de novo CRT pacing was tested in patients with conventional indication for anti-bradycardia pacing. The PREVENT-HF showed no advantage to CRT compared with conventional right ventricular pacing in terms of LV remodelling in patients with AV block and expected ventricular pacing > 80% after 12months. In the BLOCK-HF trial, patients with AV block, LVEF 50%, and NYHA functional Class I to III were randomly assigned to biventricular or right ventricular pacing and followed for 37months. The trial showed a significant reduction in the primary composite endpoint of death, HF-related urgent care or adverse LV remodelling in CRT patients compared with patients with right ventricular pacing only.
How Will I Know If My Pacemaker Needs To Be Changed
After getting a pacemaker, you will need to follow-up with the doctor and nurses in a pacemaker clinic and through phone check-ups. This will allow them to monitor your pacemaker’s function and anticipate when it will need to be changed. In addition, the pacemaker may be programmed to beep when the battery is low. Your doctor will demonstrate this beep for you.
Resynchronization therapy is only one part of a comprehensive heart failure management program. Device and/or surgical therapy, when combined with taking medications, following a low-sodium diet, making lifestyle changes, and following up with a heart failure specialist, will help you decrease symptoms and live a longer, more active life. Your doctor will help determine what treatment options are best for you.
Also Check: When Does A Heart Attack Occur
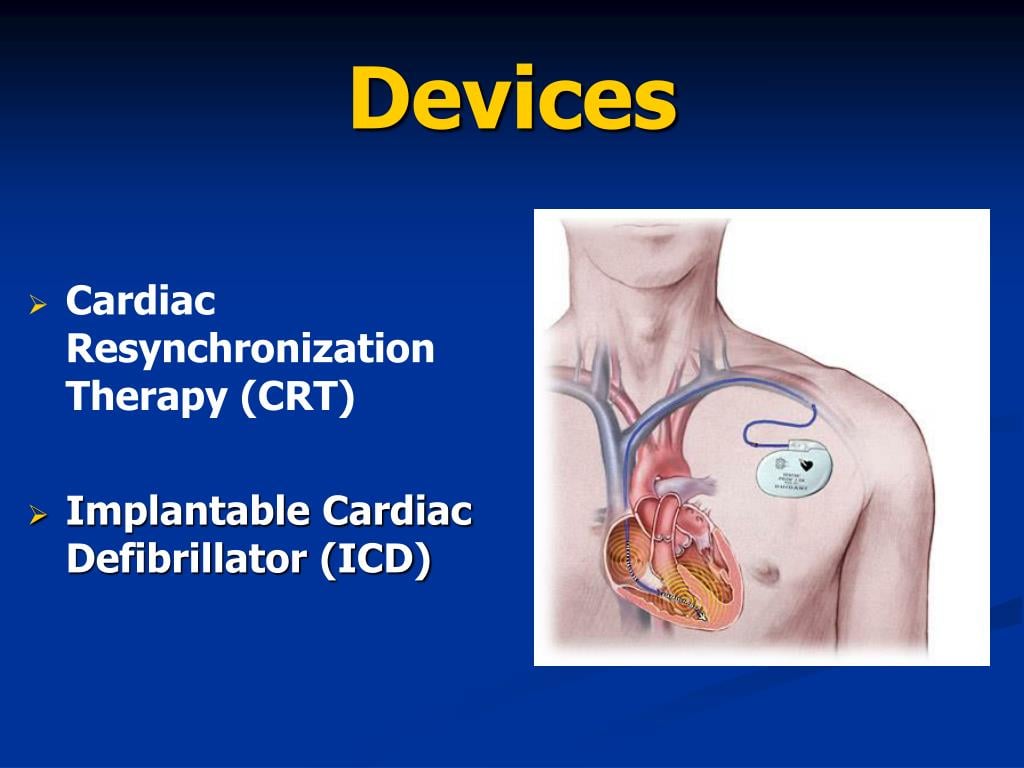
What Is A Crt Device
CRT is a clinically proven treatment option for some individuals with heart failure. A CRT device sends small electrical impulses to both lower chambers of the heart to help them beat together in a more synchronized pattern. This may improve the hearts ability to pump blood and oxygen to your body.
A CRT system is made up of two parts.
- The heart device, which is actually a tiny computer, plus a battery, contained in a small titanium metal case that is about the size of a pocket watch.
- Insulated wires, called leads, that are implanted to carry information signals from your heart to the heart device and to carry electrical impulses to your heart
After the device system is implanted, an external computer, called a programmer, located at your doctor’s office or clinic can be used to program the heart device and retrieve information from your heart device that will assist your doctor in your heart failure treatment. Your doctor will schedule periodic monitoring which may be done remotely if physician deems appropriate.
Availability Of Full Report
The full evidence report from which this summary was taken was prepared for the Agency for Healthcare Research and Quality by the University of Alberta Evidencebased Practice Center under Contract No. 290020023. Printed copies may be obtained free of charge from the AHRQ Publications Clearinghouse by calling 8003589295. Requesters should ask for Evidence Report/Technology Assessment No. 106, Cardiac Resynchronization Therapy for Congestive Heart Failure.
The Evidence Report can be also downloaded as a set of PDF files.
AHRQ Publication Number 05E0011
Current as of November 2004
Internet Citation:
McAlister F, Ezekowitz J, Wiebe N, et al. Cardiac Resynchronization Therapy for Congestive Heart Failure. Summary, Evidence Report/Technology Assessment: Number 106. AHRQ Publication Number 05E0011, November 2004. Agency for Healthcare Research and Quality, Rockville, MD.
Read Also: When Is Resting Heart Rate Too High
What Happens After The Pacemaker Is Implanted
Hospital stay: After the pacemaker implant, you will be admitted to the hospital overnight. The nurses will monitor your heart rate and rhythm. You will also have a monitor . It will record your heart rhythm while you are in the hospital. This is another way to check proper pacemaker function. The morning after your implant, you will have a chest X-ray to check your lungs and the position of your pacemaker and leads. Your pacemaker will be checked to make sure it’s working properly. The results of the test will be reported to your doctor.
Final pacemaker check: For your final pacemaker check, you will sit in a reclining chair. A small machine known as a programmer is used to check your pacemaker. It has a wand that is placed directly over the device. This machine allows the technician to read your pacemaker settings and make changes during testing. With these changes, the function of the pacemaker and leads can be evaluated. You may feel your heart beating faster or slower. This is normal however, report all symptoms to the technician. Results of the pacemaker check are discussed with your doctor who will then determine your pacemaker settings.
After your pacemaker check, an echocardiogram may be done. The technician nurse will be there during your echo and will check your pacemaker settings. The echocardiogram will be repeated with each setting to evaluate heart function. The pacemaker will keep the settings that were associated with your best heart function.
How Cardiac Resynchronization Works
Nearly one third of people with congestive heart failure have lower heart chambers, called ventricles, that do not pump in unison. This issue worsens the function of an already damaged heart.
Cardiac resynchronization therapy uses a small device called a biventricular pacemaker implanted under the skin just below the collarbone. It produces electrical pulses to stimulate the heart muscles to pump at the same time.
Some CRT devices have a built-in defibrillator. The implantable cardiac defibrillator detects dangerous, fast heartbeats and sends an electric pulse to restore a normal rhythm.
Youll receive personalized cardiac resynchronization therapy customized for the best possible results.
Read Also: How To Bring Heart Rate Down
Eligible Patients And Other Issues For Crt Application
A key issue for CRT is the identification of eligible patients who are most likely to respond and receive the most benefit. QRS duration has been deemed a primary variable as a principal electrical marker of spatially dispersed mechanical activation thus, patients with wider QRS complexes seem to have a greater mechanical response to CRT. In addition, the worse the ventricular dysfunction, which probably reflects the degree of dyssynchrony, the greater the response to CRT.
The percentage of
When Will I Be Able To Go Home After A Pacemaker Implant
Usually, you will be able to go home the day after your pacemaker is implanted. Your doctor will discuss the results of the procedure and answer any questions you may have. A doctor or nurse will go over specific instructions for your care at home. Please ask a responsible adult to drive you home, as the medications you received may cause drowsiness, making it unsafe for you to drive or operate heavy machinery.
Read Also: What Causes Fast Heart Rate And Shaking
Description Of Included Studies
All nine of the trials enrolled only patients with prolonged QRS duration: > 120 millisecond in three trials,> 130 msec in two trials,> 140 msec in one trial,> 150 msec in one trial,> 180 msec in one trial, and > 200 msec in the remaining trial. Left bundle branch block was present in 64 percent of patients, and 95 percent of patients were in sinus rhythm. All trials also restricted enrollment to patients with reduced ejection fractions , and the mean ejection fractions were similar in all trials .
In total, 3,574 patients were enrolled and 3,216 were randomized to receive CRT or control in the nine trials. The mean age was 64 years, 74 percent were male, 75 percent had NYHA Class III symptoms, and 10 percent had NYHA Class IV symptoms. Two trials included some patients with NYHA Class II symptoms., Most of the patients in these trials had ischemic etiologies for their heart failure .
Including the nine additional singlearm prospective cohort studies, a total of 3,512 patients who had undergone CRT implantation were included in the safety analyses.
Who Should Consider Crt
CRT is not appropriate for all people with heart failure. The best candidates are those who have:
- A poor ejection fraction . Ejection fraction is a measurement of how much blood the left ventricle of the heart is able to pump out with each beat.
- An ejection fraction between 36% and 50% accompanied by another indication for a permanent pacemaker, such as heart block
- Severe to moderately severe heart failure symptoms
- Seen no improvement in heart failure symptoms despite medication and lifestyle changes
- Delayed electrical activation of the heart
- History of cardiac arrest or are at risk for cardiac arrest
People with heart failure who would not benefit from or need cardiac resynchronization therapy include those who have:
- Mild heart failure symptoms
- Heart problems that do not involve dissonance in how the heart chambers beat
- A reduced ejection fraction but no other symptoms or other indications for pacing
- A limited life-expectancy due to some non-cardiac condition
- Limited functional capacity due to a chronic non-cardiac condition
-
Deterioration of the skin near the implanted device
-
Movement of the device from the site of implantation or movement of the leads placed in the heart
-
Irritation or damage electrodes may cause to heart tissue and nerves
-
Malfunctioning of the device for any reason
-
Receiving electrical impulses when they are not needed
Recommended Reading: How Much Does Heart Surgery Cost
What Is Crt And How Can It Help Your Heart
Arrhythmias are irregular heart rhythms and can be caused by a variety of reasons, including age, heart damage, medications and genetics. In heart failure patients CRT, or biventricular pacing, is used to help improve the hearts rhythm and the symptoms associated with the arrhythmia.
The procedure involves implanting a half-dollar sized pacemaker, usually just below the collarbone. Three wires connected to the device monitor the heart rate to detect heart rate irregularities and emit tiny pulses of electricity to correct them. In effect, it is “resynchronizing” the heart.
Who Is Best Suited For Crt
CRT is especially indicated for moderate to severe heart failure patients whose left and right side of the heart do not beat in unison. CRT is specifically indicated for those who belong to Class III and Class IV classification by New York Heart Association .
Breathlessness, swelling, coughing, and tiredness are some of the symptoms of heart failure. An individual must always take notice of how his body functions, and, if he experiences symptoms with ordinary activities, he falls in Class III, whereas if he experiences severe limitation and experiences symptoms of heart failure even at rest, he may then belong to class IV. Whatever be the classification and category under which he may fall, he must always ensure to make a note of his condition and side effects that must be reported as soon as possible to the doctor, who can suggest the best medication and treatment before the condition worsens with time.
CRT is indicated in patients cardiomyopathy or weak heart muscles, as well.
CRT is not indicated in the following cases:
CRT may not work for mild heart failure patients.
CRT may not work for those who have no issue with the left and right sides of the heart not beating in unison.
CRT wont work for diastolic heart failures.
Don’t Miss: Heart Failure Guidelines Acc/aha
What Is Congestive Heart Failure Cardiac Resynchronization Therapy
In this procedure, implanting a half-dollar-sized pacemaker, just below the collarbone. It connected with three wires, and the monitor detects heart rate irregularities and emits tiny pulses of electricity to correct them. In effect, it is resynchronizing the patient heart.
This device very help full for those who have serious heart rhythm problems. This device, it may be combined with the CRT. Congestive heart failure cardiac resynchronization therapy will depend on the patients health and this decision is taken by the doctor.
What Is A Biventricular Pacemaker
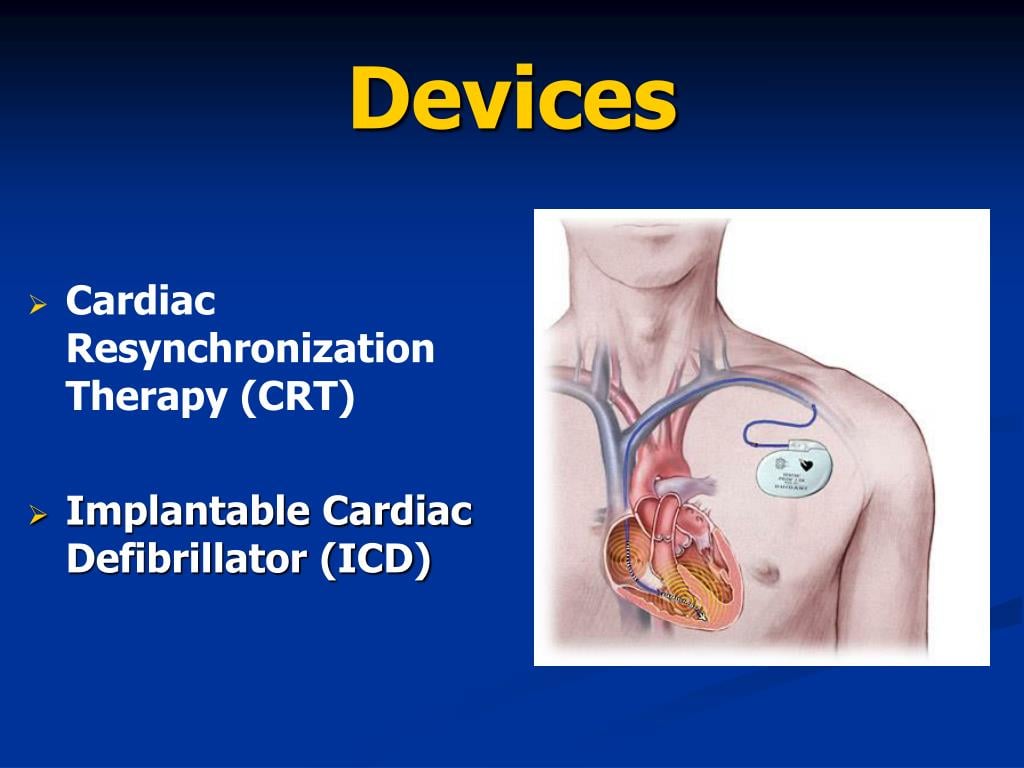
Leads are tiny wires implanted through a vein into the right ventricle and into the coronary sinus vein to pace or regulate the left ventricle. Usually , a lead is also implanted into the right atrium. This helps the heart beat in a more balanced way.
Traditional pacemakers are used to treat slow heart rhythms. Pacemakers regulate the right atrium and right ventricle to maintain a good heart rate and keep the atrium and ventricle working together. This is called AV synchrony. Biventricular pacemakers add a third lead to help the left ventricle have a more efficient contraction.
Recommended Reading: Which Of The Following Is Not A Technique Used To Diagnose Heart Disease
