Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
Causes Of Heart Failure
Heart failure is often the result of a number of problems affecting the heart at the same time.
Conditions that can lead to heart failure include:
- coronary heart disease where the arteries that supply blood to the heart become clogged up with fatty substances , which may cause angina or a heart attack
- high blood pressure this can put extra strain on the heart, which over time can lead to heart failure
- conditions affecting the heart muscle
- heart rhythm problems , such as atrial fibrillation
- damage or other problems with the heart valves
- congenital heart disease birth defects that affect the normal workings of the heart
Sometimes obesity, anaemia, drinking too much alcohol, an overactive thyroid or high pressure in the lungs can also lead to heart failure.
End Stages Of Heart Failure: What To Expect
Congestive heart failure is one of the most common reasons for hospital admissions for senior citizens. In fact, over 5 million adults in the United States experience heart failure.
Heart failure occurs when the heart muscle becomes damaged and can no longer pump blood effectively. Although symptoms can be managed, this is a chronic condition with no cure. In time, patients will reach the final stages of congestive heart failure.
Patients in the end stages of heart failure want to know what to expect. The symptoms of end-stage congestive heart failure include dyspnea, chronic cough or wheezing, edema, nausea or lack of appetite, a high heart rate, and confusion or impaired thinking.
Recommended Reading: How Do You Know If You Are Having A Heart Attack
Caring For Someone At The End Of Their Life
When someone you love is facing the end of life, its an extremely worrying and upsetting time. Given the current situation with coronavirus, you might have lots of questions about what youre allowed to do, especially if your loved one is in a hospice or care home. Many care homes are limiting visitors but government guidance has specified that visiting loved ones who are at the end of their life is important and should continue. Check with your loved ones hospice or care home about what restrictions they have in place. Unfortunately, if you have coronavirus symptoms, you wont be able to visit a loved one. Government guidance states that carers are still able to perform their caring duties if the carer doesnt have coronavirus symptoms. If you live with the person you care for and you have coronavirus symptoms, the government are advising you to ask friends and family for help with providing care or contact your local authority or healthcare provider. If someone you care for has a heart condition, they are at higher risk of severe complications of coronavirus. Be mindful of this when visiting and always follow NHS guidance around hand washing and hygiene.
-
Carers UK has helpful coronavirus guidance.
-
If you’re caring for someone who’s approaching their end of life you can find support on our caring for a heart patient page.
Supporting You And Your Loved Ones
A person-centered care model is how we approach caring for individuals and their families at the end-of-life. Hospice of Southern Illinois provides the personal care, attention and comfort during the final weeks and days of a loved ones prognosis. We want to ensure your loved ones comfort and dignity remains a priority. The circle of care for our patients starts with their needs and wishes and extends out to family, friends and caregivers. We are here to support and help you through what to expect too.
- Managing pain and other symptoms we carefully monitor pain levels and other symptoms, coordinate proper equipment, and evaluate medications to provide as much comfort and peace as possible.
- Providing support hospice offers regularly-scheduled visits from our care team to check in, provide education, listen, advocate, and explain what you need to know about the weeks ahead. Further, we offer emotional support to families along the way. Hospice care doesnt stop there. For several months after the loss of a loved one, we continue to be available for bereavement support.
- Knowing what to expect as the experts in end-of-life care, you can trust that we will work tirelessly to keep your loved one comfortable, supported and safe, all the while keeping you informed of any changes.
Also Check: Can Hypothyroidism Cause Heart Palpitations
Signs Of A Dog Dying Of Heart Failure
If your dog has just been diagnosed with congestive heart failure, you likely have many questions about what this means for their future.
CHF is a serious condition that cannot be cured, but can be managed over time with proper care. So how do you know if your dog is beginning to suffer in their condition?
In this article we will discuss the details of CHF in dogs, and help you understand the signs of a dog dying of heart failure.
Stage B Treatment Options
While stage A CHF is managed with lifestyle changes, the treatment plan for stage B typically includes taking medications regularly. People at this stage should still make the same lifestyle changes as those appropriate for stage A. However, your doctor may also prescribe additional treatments such as:
- Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, if you arent taking any as part of your stage A treatment plan
- Beta blockers if youve had a heart attack and your EF is 40% or lower, if you arent taking any as part of your stage A treatment plan
- Possible surgery or intervention as a treatment for coronary artery blockage, heart attack, valve disease, or congenital heart disease
Don’t Miss: What Is A Dangerously Low Heart Rate
Evaluation Of The Patient Being Considered For Lvad
Historically, LVADs were implanted to support patients awaiting cardiac transplantation. The REMATCH trial demonstrated the survival benefit with LVAD over inotropes in transplant-ineligible candidates, and the FDA approved LVAD use as destination therapy and added a life-saving option for patients for whom palliation was previously the only one.
Compared to transplant, the contraindications to LVAD are slightly less stringent. Nonetheless, outcomes vary and scoring systems have been devised to improve patient selection. Specific considerations include assessment of RV function, body surface area, end organ dysfunction , bleeding risk, frailty, and adequacy of social supports.
Thinking About What Care And Treatment You Would Like
For different heart conditions, there are different things you might need to consider when approaching the end of life:
-
Some people with heart failure are at risk of dying suddenly because they may develop a life-threatening heart rhythm. This can lead to a cardiac arrest. You may want to think about what you would want to happen if you had a cardiac arrest and whether you would want to have CPR or not. Without CPR, your heart rhythm would not be restored, and you would die.
-
If you have an ICD fitted, you might want to discuss whether to deactivate it . This would mean that if you were to have a cardiac arrest, your ICD wouldnt be there to restore your heart rhythm which would help to minimise any discomfort or distress. Read our ICD deactivation FAQs for more information.
-
Antibiotics are given to help your body fight infection. You may decide to refuse antibiotics.
Its good idea to involve loved ones in these kinds of decisions so theyre aware of your wishes. You might also want to discuss matters like organ donation and how you intend for your wishes to be recorded.
Recommended Reading: What Artery Supplies Blood To The Heart
What Are The Symptoms Of End
Heart Failure: Quick Facts
1. More than 6 million U.S. adults have heart failure.
2. About half of people who develop heart failure die within 5 years of diagnosis.
3. Most people with end-stage heart failure have a life expectancy of less than 1 year.
4. The leading causes of heart failure are diseases that damage the heart, such as heart disease, high blood pressure, and diabetes.
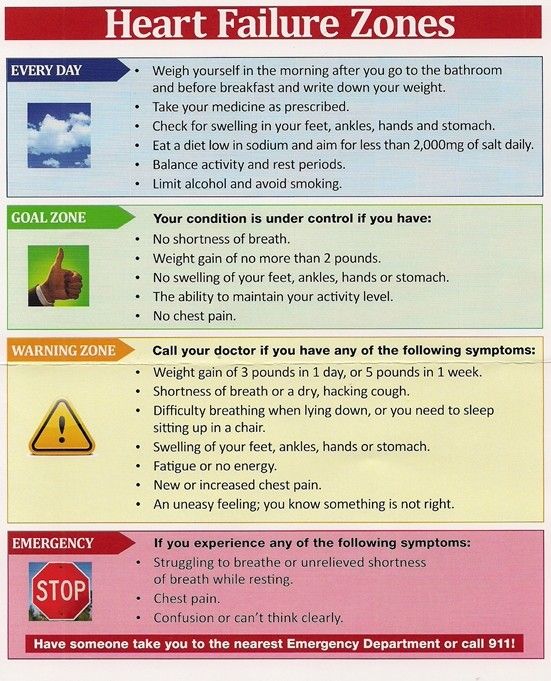
Heart failure worsens over time, so symptoms are most severe during the final stages. It causes fluid to build up in the body, which produces many of these symptoms:
- Shortness of breath . In the final stages of heart failure, people feel breathless both during activity and at rest.
- Persistent coughing or wheezing. This may produce white or pink mucus. The cough may be worse at night or when lying down.
- Weight gain or swelling of the feet, ankles, legs, abdomen, or neck veins.
- Tiredness, weakness.
In addition, people in the final stages of heart failure may suffer from:
- depression, fear, insomnia, and isolation
- anxiety about their future
- trouble navigating the health care system
What Are The Symptoms Of Heart Failure
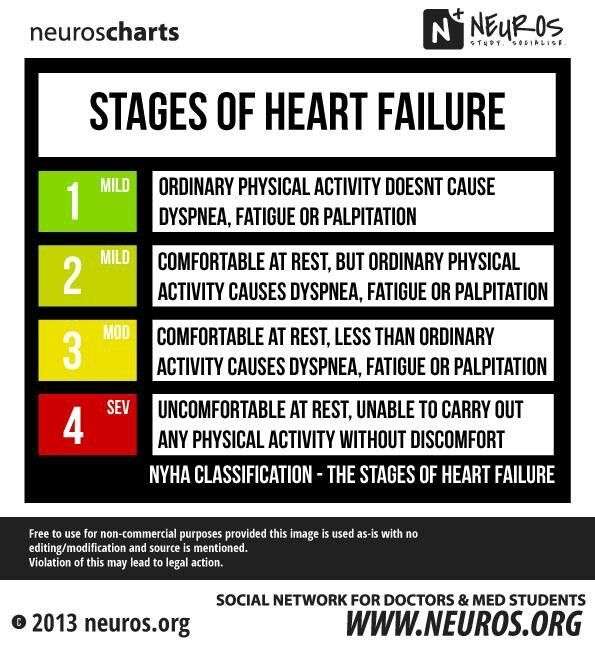
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesnt mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe, and may come and go.
In general, heart failure gets worse over time. As it worsens, you may have more or different signs or symptoms. It is important to let your doctor know if you have new symptoms or if your symptoms get worse.
Read Also: Acetaminophen Heart Rate
Also Check: Heart Attacks Signs And Symptoms
What Are The Signs Of End Stage Heart Failure
What Are the Signs of End Stage Heart Failure?
About 6.2 million adults in the U.S. have heart failure, and heart disease is responsible for one in four deaths. While there is no cure for end stage heart failure, symptoms can be managed through palliative or hospice care. If you have a loved one with heart failure, you may be wondering how to recognize the signs of end stage heart failure.
What Is Heart Failure?
Heart failure is a condition in which the heart is not pumping blood throughout the body as efficiently as it should. Heart failure is a serious condition, but it does not mean that the heart has stopped beating.
Most of the time, heart failure1 develops and progresses gradually. A person at the end stage of heart failure may have many symptoms and experience them even while resting. Symptoms may include:
- Difficulty breathing
- Increasing discomfort with any amount of physical activity
Managing Symptoms of Heart Failure
Good medical management of heart failure can help a person live longer, with a better quality of life. It can also help reduce emergency room visits and hospitalizations. Gilchrists Advanced Cardiac Care community-integrated partnership helps those living with end-stage heart disease manage their symptoms. In addition, hospice care can provide invaluable care and support to the patient and family.
How Can Hospice Help People With Heart Failure?
Sympathetic Nervous System Activation
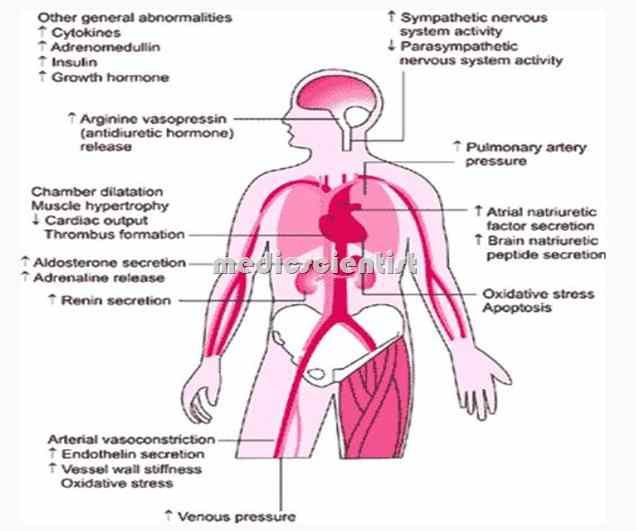
Under normal circumstances, the SNS is inhibited by the high-pressure baroreceptors and low pressure mechanoreceptors in the heart. In HF however, these inhibitory mechanisms are diminished due to increased pressure in the LV and reduced pressure at the level of the baroreceptor, resulting in over-activation of the SNS. Early on, this augments heart rate and contractility, helping to maintain cardiac output. However ultimately beta-adrenergic responsiveness decreases and norepinephrine stores are depleted, while increased hypertrophy, fibrosis, and myocyte necrosis ensue.
Recommended Reading: Why Do Av Nodal Cells Not Determine The Heart Rate
Stage A Treatment Options
Treatment options in stage A mainly focus on promoting your overall health and disease prevention. If you meet the stage A criteria, your doctor will recommend lifestyle changes to slow or stop disease progression.
Heart Failure Doctor Discussion Guide
What Can Hospice Do For The Family Of A Person With Heart Disease
Family members may have to make difficult healthcare and financial decisions, act as caregivers and provide emotional support to others. If the decision is made to stop medical support, some families experience strong emotions and feel overwhelmed.
Hospice offers comprehensive services for families of patients with heart disease:
Read Also: How To Check Resting Heart Rate
What Is The Treatment For Congestive Heart Failure
The treatment of heart failure depends on the exact cause, but it can usually be treated effectively. The overall goals are to correct underlying causes, to relieve symptoms, and to prevent worsening of the condition. Symptoms are relieved by removing excess fluid from the body, improving blood flow, improving heart muscle function, and increasing delivery of oxygen to the body tissues. This can be done by the various congestive heart failure treatments listed in this sections.
If the underlying cause of heart failure is not correctable by surgery or catheterization procedures, medical treatment is composed of lifestyle changes and medications.
Dont Miss: Ibs And Palpitations
Addressing Comorbidities And Consequences
There is a myriad of comorbidities common in HF patients that may contribute to the pathology of the cardiomyopathy itself and/or the patients clinical status. These are, in general, associated with worse outcomes. Pre-existing comorbidities are often compounded by the consequences of advanced HF, resulting in severe end-organ dysfunction.
You May Like: Cost For Heart Surgery
Other Common Reversible Aetiologies
Important other reversible/correctable aetiologies include tachycardia , thyroid disease, alcohol, illicit drugs , certain chemotherapies , and valvular disease. In the latter case, one must decide if the valvular dysfunction is primary , in which case corrective intervention may allow for full ventricular recovery. In contrast, if mitral regurgitation is secondary to ventricular dilation, the evidence for correction is less well established and the risks may outweigh the benefits. In addition, medical therapies with beneficial effects on ventricular remodelling may reduce or even eliminate regurgitation.
How Can I Support Someone
The progression of heart failure can be unpredictable, which makes it difficult to know when to have conversations about end of life care. Its important to discuss things as early as possible, giving people the time to think about treatment options and where they want to be cared for towards the end of their life. This may help them achieve some peace of mind and a sense of control.
Its vital that the person is able to make informed decisions about their care, so find out if they have enough information about their condition, and how it may impact their life towards the end stages.
Its helpful for someone with suitable experience to start conversations about the following:
Don’t Miss: What Are Some Heart Disease
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Where Youd Like To Be Cared For
An important choice to make is where youd like to be cared for. Everyone is different and will have different priorities for their care. This is something to chat to family and friends about as they might have opinions too. You can express your wishes about where youd liked to be cared for in an advance statement or advance decision. Your decision might be affected by the coronavirus pandemic so its a good idea to have a second option. Bear in mind that you might need to be flexible about your wishes, as hard as this may be. Talk to your GP or nurse if you have any queries about how your care might be affected.
Recommended Reading: How To Measure Resting Heart Rate
