Systematic Reviews And Meta
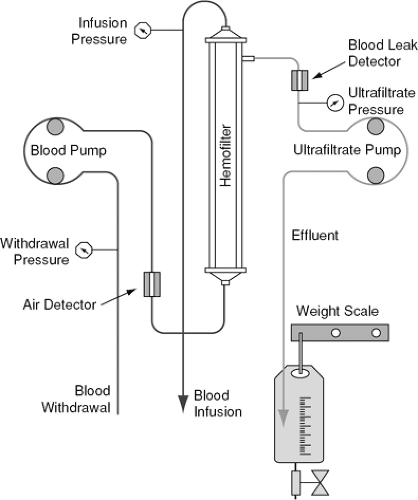
Recently, several meta-analyses have been performed to compare UF with diuretics for treating volume overload in patients with ADHF. The first meta-analysis comprised nine studies involving 613 patients . The mean weight loss in patients receiving UF therapy was 1.78 kg . This loss was more than for those treated with standard diuretic therapy. However, between the two groups, there was little difference in post-intervention creatinine levels . In addition, the results showed that, compared with patients treated with standard diuretics, in those treated with UF, the risk of all-cause mortality persisted .
Figure 2.
Forest plot of: a) Changes in weight loss at 48 h post therapy, b) all-cause mortality, c) all-cause rehospitalization. Reprinted from Cheng et al. , copyright with permission from International Heart Journal.
You May Like: What Are The Signs Of Heart Attack In Women
How Is Congestive Heart Failure Treated
Doctors will assess the current health status of the patient to establish a baseline, and develop a long-term health plan. This may involve the optimization of medicines and therapies, adding new medication, or possibly enrollment in a clinical trial.
Stabilizing and/or reversing a patients condition often involves long-term, collaborative follow-up with a referring cardiologist or physician.
In serious situations, advanced therapies, which include mechanical solutions, a heart transplant, or hospice, may be offered.
You May Like: What Causes Heart Palpitations At Night
Reducing Right Ventricular Afterload
Studies show BiPAP is very helpful for CHF, supporting your breathing so you dont have to work as hard to inhale.1-2 It also helps your heart. Some people might say that it pushes fluid out of your lungs, and though it might happen to a small degree, its not the main reason BiPAP is helpful for CHF.
The main way BiPAP helps is by reducing right ventricular afterload. Thats a fancy medical term meaning the heart doesnt have to work as hard to push blood through your lungs. In essence, it makes your heart a better pump.2 It also reduces systemic venous return to your heart. This means less blood flows back to your heart, less work for your heart, and less swelling overall. Lastly, BiPAP helps maintain normal oxygen levels which can help you feel better.1-2
Also Check: Final Stages Of Diastolic Heart Failure
Enhancing Healthcare Team Outcomes
The treatment of heart failure and acute decompensated heart failure is challenging despite the use of maximal evidence-based therapy based on the stage of heart failure. Given the limited effect that current treatment strategies have on the progression of heart failure, it is important to identify ways to maximize patient outcomes and quality of care by the interprofessional team.
Patients at potential risk for heart failure based on comorbidities or other identified risk factors should receive appropriate evidence-based preventative counseling and treatments. When appropriate, the primary care providers who may be the most involved in the management of the patients’ risk factors should consult other specialists, including cardiologists, endocrinologists, pharmacists, cardiology nurses, and nutritionists, to ensure that they are providing the best advice and treatment for their patients. Nurses monitor patients, provide education, and collaborate with the physicians and the rest of the team to improve outcomes. Pharmacists review medications, inform patients and their families about side effects and monitor compliance.
Given the propensity of heart failure patients to require re-current admissions, often because of non-heart failure related conditions, the collaboration between inpatient and outpatient services can be of benefit in the continuity of care and helping promote improved outcomes.
Fluid Overload Recognition And Assessment
Fluid overload recognition and assessment in critically ill patients requires an accurate documentation of intakes and outputs however, there is a wide variation in how this information is recorded, reviewed and utilized. Mehta RL and Bouchard J proposed some useful definitions to help us to standardize the approach and facilitated comparisons :
Daily fluid balance: daily difference in all intakes and all outputs, which frequently does not include insensible losses.
Fluid accumulation: positive fluid balance, with or without linked fluid overload.
Percentage of fluid overload adjusted for body weight: cumulative fluid balance that is expressed as a percent. A cutoff of 10 % has been associated with increased mortality. Fluid overload percentage can be calculated using the following formula :
Recommended Reading: Heart Attack Symptoms In Females
Cirrhosis Of The Liver
Hypervolemia may occur when the liver cannot properly store and process nutrients and filter toxins. Liver problems tend to cause fluid retention in the abdominal area and the extremities.
According to an article in the journal , fluid accumulation in the abdomen is the most common complication of cirrhosis of the liver. This specific buildup in the abdominal area is known as ascites.
How Do We Identify Congestion
The accumulation of fluids is a gradual process. In normal circulation, there is continuous filtration of fluid from the intravascular space into the tissues at a rate dependent on the gradient between the intravascular and extravascular hydrostatic pressure. Any filtered fluid is then drained by the lymphatics. Overt cardiogenic peripheral oedema develops because the fluid retention results in an increase in intravascular hydrostatic pressure and a commensurate increase in the filtration rate, which eventually exceeds the capacity of the lymphatics to drain fluid away .
A Simplified Pathophysiology of Pulmonary Oedema or Peripheral Oedema Development in Patients with HFREF or HeFNEF
HeFNEF = heart failure with normal ejection fraction HFREF = heart failure with reduced ejection fraction LV= left ventricular.
Some patients do not present until they have developed widespread peripheral oedema. In such cases the need for medical intervention is obvious. However, a substantial number of cases of subclinical congestion will not be clinically recognised, despite the presence of symptoms . In patients with no known cardiac disease, particularly in older people, the identification of subclinical congestion at an earlier stage might change the trajectory of the disease. In patients who are already known to have HF, whether subclinical congestion is important is not clear.
Read Also: How To Improve Heart Rate Variability
How Is Fluid Overload Diagnosed
A number of conditions produce signs and symptoms that resemble fluid overload, and these need to be excluded. These conditions include:
- Blood tests to check your kidney function, blood count, liver function, blood gases.
- A special test for heart failure, called B-type natriuretic peptide .
- Charts to check how much you drink and pee and any weight changes in response to treatment.
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Recommended Reading: What Are Symptoms Of Heart Attack
Portion Out Your Fluids
Try to distribute your fluid consumption throughout your day. If you wake up and drink a bunch of coffee and water, you might not have much room for other fluids throughout the day.
Budget the 2,000 mL throughout your day. For example, have 500 mL for breakfast, lunch, and dinner. This leaves with room for two 250 mL drinks between meals.
Work with your doctor to determine how much you need to restrict your fluid intake.
Recommended Reading: Why My Heart Rate Is High
What Medications Should I Avoid If I Have Heart Failure
There are several different types of medications that are best avoided in those with heart failure including:
- Nonsteroidal anti-inflammatory medications such as Motrin or Aleve. For relief of aches, pains, or fever take Tylenol instead.
- Most calcium channel blockers
- Some nutritional supplements, such as salt substitutes, and growth hormone therapies
- Antacids that contain sodium
If youâre taking any of these drugs, discuss them with your doctor.
Itâs important to know the names of your medications, what theyâre used for, and how often and at what times you take them. Keep a list of your medications and bring them with you to each of your doctor visits. Never stop taking your medications without discussing it with your doctor. Even if you have no symptoms, your medications decrease the work of your heart so that it can pump more effectively.
Recommended Reading: What Does Heart Attack Pain Feel Like
Fluid Overload And Outcomes
Several observational studies have demonstrated a correlation between fluid overload and mortality in critically ill patients with acute respiratory distress syndrome, acute lung injury, sepsis, and AKI. Bouchard et al., have shown that patients with fluid overload defined as an increase in body weight of over 10 % had significantly more respiratory failure, need of mechanical ventilation, and more sepsis. After adjusting for severity of illness, AKI patients with fluid overload had increased 30 day and 60 day mortality. Among survivors, AKI patients who required renal replacement therapy had a significantly lower level of fluid accumulation at initiation of dialysis and at dialysis cessation than non-survivors. Renal recovery was significantly lower in patients with fluid overload . In children, a multicenter prospective study found that the percentage of fluid accumulation at initiation of CRRT was significantly lower in the survivors .
Acute Decompensated Heart Failure With Adequate Perfusion
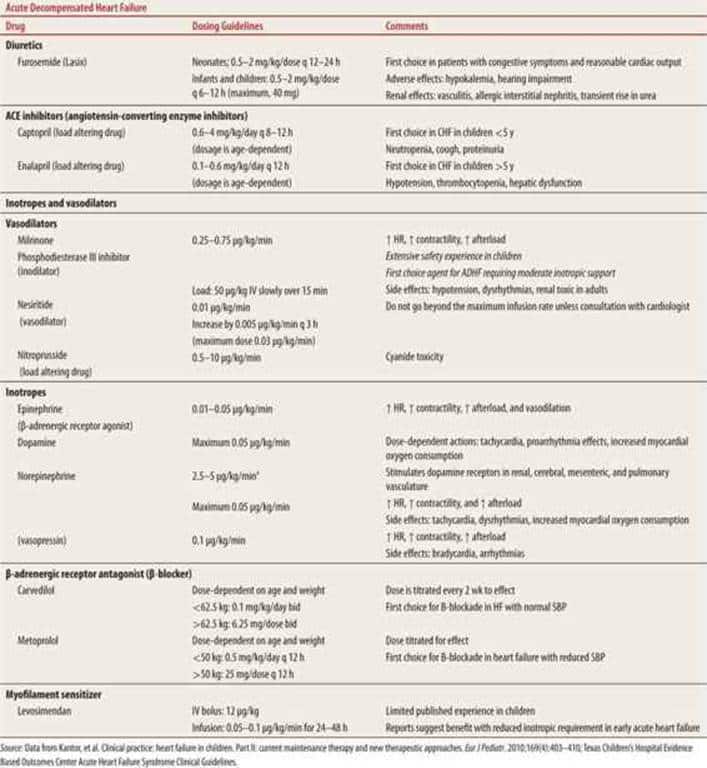
Management decisions for heart failure exacerbations should be guided based on assessment of perfusion and hemodynamic stability. Patients with stable to elevated blood pressures are demonstrating compensatory mechanisms to maintain systemic perfusion. Patients with such presentations have been shown to have lower mortality than those without substantial myocardial reserves.33
Therapeutic modalities in acute heart failure exacerbations involve reduction of preload and afterload, with careful monitoring to maintain adequate hemodynamic and respiratory function. Hypoxemia should be corrected with supplemental oxygen either via nasal cannula or high-flow face mask. Physicians and nursing staff should be careful not to administer supplemental oxygen routinely because excessive oxygen has been linked to worsened outcomes in decompensated heart failure.34
Patients who do not respond to supplemental oxygen should be considered candidates for noninvasive positive pressure ventilation based on mental status and respiratory effort. Use of these measures can restore vital signs rapidly and improve symptomatology by decreasing preload through increased intrathoracic pressures. The use of noninvasive ventilation in conjunction with medical therapy appears to reduce the need for intubation compared to medical therapy alone.35
Recommended Reading: Congestive Heart Failure And Afib In Elderly
Is There A Treatment For Heart Failure
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are to try to keep it from getting worse , to ease symptoms, and to improve quality of life.
Some common types of medicines used to treat it are:
- Aldosterone antagonists
- Selective sinus node inhibitors
- SGLT2 inhibitor
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. It usually includes workouts that are designed just for you, education, and tips to lower your chance of heart trouble, like quitting smoking or changing your diet.
Cardiac rehab also offers emotional support. You can meet people like you who can help you stay on track.
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Read Also: What Is High Resting Heart Rate
Quality Of Patient Care
Brigham and Womens Hospital is committed to providing all of our patients with the safest, highest-quality, most-satisfying care possible and follow established protocols that have been shown to improve patient outcomes. Our inpatient satisfaction survey, sent to patients to assess their total care experience, helps us to monitor what we are doing well and areas for improvement. We pride ourselves in the quality of patient care we provide and how we are measured compared with other hospitals.
Dont Miss: Where Do You Feel Heart Palpitations
Pacemakers And Other Devices
The heart has its own electrical system that regulates the heartbeat. With every heartbeat, there’s an electrical signal that travels through your heart, causing it to contract and pump blood around the body.
For some people with heart failure, the electrical system doesnt work properly. People with heart failure have an increased risk of abnormal heart rhythms , like atrial fibrillation. If you have an abnormal heart rhythm, you may need a pacemaker or device to regulate the heart rate and rhythm.
You May Like: How To Lower My Resting Heart Rate
What Are Some Congestive Heart Failure Causes
According to the Mayo Clinic and the NHLBI, the most common congestive heart failure causes include:
- High blood pressure, which describes how forcefully your blood pushes against the walls of your arteries. Chronically high blood pressure can cause heart damage.
- Coronary artery disease, which happens when the arteries in your heart become narrow, restricting blood flow.
- Heart attack, which develops when part of the hearts muscle doesnt receive enough blood. This often occurs suddenly and can permanently damage your heart.
- Diabetes, which can damage your blood vessels and the nerves in your heart.
- Endocarditis, which is when harmful pathogens like bacteria get into your blood and infect previously-damaged heart tissue.
- Metabolic syndrome, which means you have several risk factors that increase your risk for heart disease. These include high blood pressure, a larger waistline, high blood sugar, high triglycerides , and low HDL cholesterol levels.
- Heart valve disease, which is when at least one of your four valves doesnt fully open or close.
- Congenital heart defects, which is when parts of your heart dont form properly. This generally happens before youre born and makes your heart work harder.
- Heartbeat irregularities, which means your heart beats too fast, too slow, or in an odd rhythm.
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Don’t Miss: Who Has More Heart Attacks Male Or Female
Find Alternative Thirst Quenchers
Its tempting to guzzle a bunch of water when youre thirsty. But sometimes, just moistening your mouth can do the trick.
The next time youre tempted to gulp down some water, try these alternatives.
- Swish water around your mouth and spit it out.
- Suck on sugar-free candy or chew sugar-free gum.
- Roll a small ice cube around the inside of your mouth.
Effects Of Fluid Retention
As fluid settles in different areas of the body, seniors may experience a range of symptoms.
- The fluids can settle in the lungs or chest cavity, resulting in shortness of breath or cough.
- If fluids settle in the extremities, individuals may experience swelling and weight gain due to fluid retention.
- Seniors may also experience bloating in their stomachs as fluid settles in the abdomen, reducing their appetite or causing nausea.
If a senior notices sudden swelling or changes in symptoms, they should seek medical attention immediately. The symptoms of CHF and fluid buildup as a result of the condition are gradual, so any sudden change is a sign that something else could be going on.
Dont Miss: Does Alcohol Speed Up Heart Rate
Recommended Reading: How Do You Lower Your Resting Heart Rate
What Happens In Congestive Heart Failure
The heart has two upper chambers and two lower chambers . Normally, blood:
But in heart failure, the heart cant work as it should and not enough blood and oxygen get to the organs. And blood backs up in the heart and then into the lungs.
Read Also: Congestive Heart Disease Symptoms
