Caring For Someone With Heart Failure Towards The End Of Life
Please be aware – this information is for healthcare professionals.
You can use our My Learning form to reflect on how this page has helped with your continuing professional development.
If you’re a patient, or a family member or friend, you can find more information on heart failure from the British Heart Foundation .
Heart failure means the heart is not pumping blood around the body as well as it should. People with heart failure may have symptoms such as fatigue, breathlessness and oedema . Here, we’ll talk about knowing when a patient with heart failure is near the end of life, and how to support them.
This information is about supporting adults with advanced heart failure.
On this page:
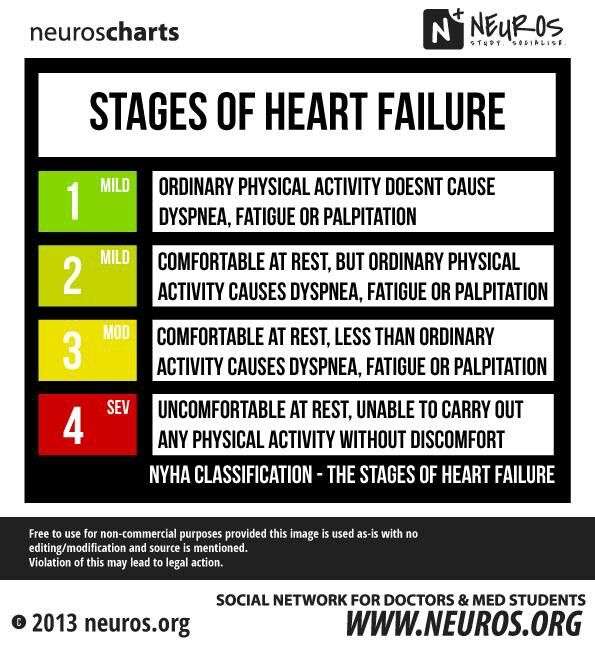
Stages And Classes Defined
Heart failure is generally classified by the severity of a patients symptoms. The most common classification system is the New York Heart Association Functional Classification. There are four levels of clinical classification used to stratify both the presence of symptoms and limitations experienced during physical activity. The severity of symptoms is made by comparison to normal breathing, shortness of breath, and/or angina .1
The symptoms of heart failure associated with function during physical activity are an important indicator of disease progression and prognosis.1-2
- Class I: No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF.
- Class II: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF.
- Class III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF.
- Class IV: Symptoms occur even at rest discomfort with any physical activity. Unable to carry on any physical activity without symptoms of HF.
Class I and II are typically categorized as mild heart failure, while class III and IV are considered more severe or advanced heart failure. A person can move back and forth between these classes based on their symptoms. When a patient has a heart failure exacerbation, they will have more symptoms and likely be a higher class, but when their symptoms are better controlled, they will fall into a lower class.1-4
B: Delivery Of Health Care
B1: Perceptions regarding care
B1.a: Appropriateness of care
The interviewed patients assessment of the quality of medical and nursing care varied depending on whether they thought the treatment was appropriate, necessary and met their needs. If decisions about medical treatment, prescriptions and home visits made by the professionals do not meet a patients expectations, they may be perceived as inadequate or wrong. Treatment of pain was particularly highlighted: The fact that patients often perceive pain as an expression of complete suffering not attributable to any particular cause leads to a type of indifference that makes any medical help inconceivable. The following quotation clearly illustrates this perception of ubiquitous suffering, which the patient repeatedly mentioned in every interview.
Patient HD12, T2 : I only want to feel better. But it seems its not to be, nothing good. Being ill, theres nothing wanted, nothing needed, its always the same. I dont need anything, I can be quite alone. Pain everywhere
Patient HD06, T1 : So you know, if a patient is really ill, yes, its good when you have someone who looks after you. I mean, I do not want too much care, it would be too much responsibility for me, you know. But if youre not feeling well, its good to have someone.
B1.b: Continuity of care
B2: Interpersonal relationships
B2.a: Interaction in the processes of care
B2.b: Specific aspects in physician-patient interaction
B3: Meaning of family
You May Like: What Can Cause Low Heart Rate
What Happens If You Have Heart Failure
People with heart failure have weak hearts that dont work as well as they should. Over time, the illness causes significant damage to the body.
In the first stages, the heart is less effective. It stretches, grows bigger, and pumps faster to compensate for the lack of strength. The body also changes, with arteries getting smaller and blood being directed away from certain body parts. Many people with heart failure dont know they have a problem in these early stages.
Towards the end stages of CHF, symptoms will worsen even if lifestyle changes are made, and the body will be unable to compensate for the loss of blood flow. As soon as that happens, the person may start to feel tired, have trouble breathing, and have other problems.
People can get help managing their end stages congestive heart failure symptoms and slowing down the progress of their condition with a variety of treatments. Its a long-term condition that cant be cured, as well as heart failure. People will eventually reach the end stages of heart failure.
Even when the person is lying down, they feel a shortness of breath. Their symptoms can change rapidly over a short period of time.
Talk To Them About Their Symptoms
People with heart failure may feel worried about their symptoms, treatment or risk of dying suddenly. Reassure them by talking openly and honestly about their concerns. Speak to their cardiac or palliative care team if you need support. If the patient has a plan for managing symptoms or emergencies, they may feel less anxious.
Recommended Reading: Does Gabapentin Affect Your Heart Rate
Even For Advanced Hf There Are Treatment Options
When heart failure progresses to an advanced stage, difficult decisions must be made. Do I want to receive aggressive treatment? Is quality of life more important than living as long as possible? How do I feel about resuscitation?
For advanced heart failure patients and their doctors, making good decisions requires teamwork. Through shared decision-making, doctors and patients consider both the options and the patients preferences before charting a treatment course.
Causes Of Heart Failure
Heart failure is often the result of a number of problems affecting the heart at the same time.
Conditions that can lead to heart failure include:
- coronary heart disease where the arteries that supply blood to the heart become clogged up with fatty substances , which may cause angina or a heart attack
- high blood pressure this can put extra strain on the heart, which over time can lead to heart failure
- conditions affecting the heart muscle
- heart rhythm problems , such as atrial fibrillation
- damage or other problems with the heart valves
- congenital heart disease birth defects that affect the normal workings of the heart
Sometimes obesity, anaemia, drinking too much alcohol, an overactive thyroid or high pressure in the lungs can also lead to heart failure.
Also Check: How Long Can A Heart Attack Last
Recommended Reading: How Do You Find Your Target Heart Rate Zone
Heart Failure Expectations Unrealistic
In the study, researchers surveyed 122 people with moderate to advanced congestive heart failure about their perception of their life expectancy.
They found the heart failure patients tended to overestimate their life expectancy by about three years. The average patient survival estimate was 13 years compared with a validated medical model estimate of 10 years.
Overall, 63% of people with heart failure overestimated their remaining life expectancy by an average of 40% compared with medical model predictions. Those who were younger and with more advanced disease were most likely to overestimate how long they had left to live.
During the three-year follow-up period, 29% of the people involved in the survey died. Researchers found no relationship between longer life expectancy perceptions and survival.
How Long Can A Chihuahua Live With Heart Failure?
Is dying of congestive heart failure painful? Pain. Some people with heart failure can experience pain or discomfort towards the end of their life. They should be assessed using a pain scale. Pain-relieving medicines can be used to relieve pain and discomfort this can include opioid and non-opioid medicines .
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
You May Like: Neurological Problems After Open Heart Surgery
Signs It Might Be Time For Hospice
Patients are considered to be in the terminal end stage of heart disease when they have a life expectancy of six months or less. Only a doctor can make a clinical determination of congestive heart failure life expectancy. However, look for these common signs that the disease has progressed to a point where all involved would likely benefit from hospice services:
- The patient has advanced congestive heart failure or advanced coronary disease with frequent episodes of angina .
- The patient has an abnormal heart and suffers significant symptoms of fatigue, shortness of breath or functional decline.
- Optimal treatment for the patients condition has already been provided and he or she is not a candidate for further surgical or medical intervention.
- The patient has tried optimal treatment and made the personal choice not to pursue any further specialized treatment.
People often say, I wish I had asked about hospice sooner.1 Reports show early referral to hospice results in greater satisfaction for the patient and their caregivers. In 2015, seriously ill patients received hospice services for an average of 69.5 days, but given more time, hospice resources can supplement care provided by doctors and loved ones through a patients last six months of life.
How Palliative And Hospice Care Can Help With End
Both palliative and hospice care focus on the whole person, including their physical, emotional, social, and spiritual needs. The main difference is that palliative care can be given at any time during a serious illness, and hospice care is given near the end of life typically when a persons prognosis is six months or less.
Palliative and hospice care can also provide help with making difficult treatment decisions, such as whether to be resuscitated if the persons heart stops, or whether to have a tube placed in their throat to help them breathe.
Similarly, people with end-stage heart failure may need to decide when to disable certain medical devices implanted in their body:
- Implantable cardioverter defibrillator . Patients can have the shock function turned off, or not replace the battery when the current one runs out. Electrical shocks from ICDs can cause unnecessary distress for patients and loved ones at the end of life.
- Left ventricular assist device . Typically, the patient decides when this heart pump will be shut off before it is implanted. The decision can be discussed again as the end of life nears.
Recommended Reading: What Is A Normal Heart Rate While Walking
What Do Symptoms Of End Stage Congestive Heart Failure Look Like
Dyspnea
Dyspnea or shortness of breath can occur both during activity and rest. This is the symptom that often sends patients racing to the hospital late at night. Work with your hospice or palliative care team to manage symptoms at home and avoid these stressful hospital trips.
Chronic Cough
When the heart cannot keep up with the supply of blood moving between it and the lungs, fluid can build up in the lungs. This results in a chronic cough or wheezing that can produce white or pink mucus.
Edema
As the hearts ability to pump slows down, fluid can build up in the body. This creates swelling in the extremities particularly the feet, ankles, legs, or abdomen.
Lack of Appetite
As the digestive system receives less blood, patients may feel full or nauseous. Not wanting to eat is a natural part of the body shutting down, but families often find this distressing. Learn more about why it is okay for your loved one to stop eating and drinking at end of life.
High Heart Rate
In response to a loss in pumping capacity, the heart begins to beat faster. The patient experiences this as a racing or throbbing heartbeat.
Confusion
When the heart stops working effectively, it can change sodium levels in the blood. This leads to memory loss, confusion, and a general feeling of disorientation.
Dilemmas From The Patient And Caregiver Perspective
In an interview study of 64 caregivers at 6 months after the patients death, there were common themes regarding end of life planning issues: lack of availability of treatment options for certain patients, changes in preferences at the very end of illness, variability in patient and caregiver desire for and readiness to hear information about the patients illness, and difficulties with patientâcaregiver communication. Patients and their caregivers may fail to raise end-of-life issues for various reasons including: lack of understanding their condition unpredictability of the clinical trajectory of HF discomfort and anxiety in raising end-of-life discussions and a feeling of powerlessness while viewing clinicians as unapproachable or reluctant to give out information.
In a study of patient preferences regarding end-of-life treatment in advanced HF, two distinct groups of patients were identified: one group preferred life-prolonging treatments, while the other group favoring strategies that improved quality of life despite reduced survival time. As treatment preferences were independent of functional or symptom status, this may present an important opportunity for clinicians to discuss such treatment preferences early in the course of illness and help facilitate end-of-life planning.
You May Like: How To Take Your Heart Rate
Interactive Multiple Choice Questions
This Education in Heart article has an accompanying series of six EBAC accredited multiple choice questions .
To access the questions, click on BMJ Learning: Take this module on BMJ Learning from the content box at the top right and bottom left of the online article. For more information please go to: Please note: The MCQs are hosted on BMJ Learningthe best available learning website for medical professionals from the BMJ Group.
If prompted, subscribers must sign into Heart with their journal’s username and password. All users must also complete a onetime registration on BMJ Learning and subsequently log in on every visit.
When Should We Consider Hospice Care For Chf
Hospice can be appropriate for many types of end-stage heart disease, including heart failure, valvular heart disease and coronary artery disease. Regardless of the type of heart disease, hospice is a fitting choice when an individual begins to experience persistent, severe symptoms that interfere with their daily life. Hospice care should also be considered if an individual begins to have recurrent hospitalizations or complicated hospitalizations, such as an ICU stay.
One of the earliest symptoms of a declining heart is exercise intolerance. This begins with symptoms present with significant exertion and can progress to symptoms present with doing our activities of daily living, such as bathing and dressing. At its worst, symptoms are present at rest. Heart disease, depending on the etiology, can present with other more specific symptoms, including fluid overload, chest pain, lightheadedness, shortness of breath and arrythmias. Patients may experience unintentional weight loss despite a normal appetite. As the disease progresses, cardiac output can decline, resulting in low blood pressure and poor prefusion of our vital organs. This can lead to dysfunction of further organ symptoms, such as worsening kidney function.
You May Like: Which Structures Carry Blood Away From The Heart
Types Of Heart Failure
The main types of heart failure are named for where they occur in the heart:
- Left-sided heart failure
- Biventricular heart failure
Clinicians also may classify heart failure as:
- Acute: You have active symptoms of heart failure, with either a new diagnosis or with long-term heart failure.
- Chronic: You have a history of heart failure, but your condition is relatively stable with no symptoms or with manageable symptoms.
Surgery For Heart Failure
Your doctor may recommend surgery to implant a medical device that helps the heart function more effectively:
- Pacemaker, which maintains a steady heart beat in people with a slow or irregular heartbeat
- Implantable cardioverter defibrillator , which monitors the heart for fast rhythm and delivers an electrical shock to reset normal rhythm
- Left ventricular assist device , which takes over the pumping action of the heart
People with advanced heart failure may be candidates for heart transplantation. A heart transplant replaces the diseased heart with a donated heart from a person who has died.
Read Also: Coughing Congestive Heart Failure
Supporting You And Your Loved Ones
A person-centered care model is how we approach caring for individuals and their families at the end-of-life. Hospice of Southern Illinois provides the personal care, attention and comfort during the final weeks and days of a loved ones prognosis. We want to ensure your loved ones comfort and dignity remains a priority. The circle of care for our patients starts with their needs and wishes and extends out to family, friends and caregivers. We are here to support and help you through what to expect too.
- Managing pain and other symptoms we carefully monitor pain levels and other symptoms, coordinate proper equipment, and evaluate medications to provide as much comfort and peace as possible.
- Providing support hospice offers regularly-scheduled visits from our care team to check in, provide education, listen, advocate, and explain what you need to know about the weeks ahead. Further, we offer emotional support to families along the way. Hospice care doesnt stop there. For several months after the loss of a loved one, we continue to be available for bereavement support.
- Knowing what to expect as the experts in end-of-life care, you can trust that we will work tirelessly to keep your loved one comfortable, supported and safe, all the while keeping you informed of any changes.
