Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Nutritional deficiencies
Heart Failure With Preserved Ejection Fraction
In diastolic heart failure , the same pathophysiologic processes occur that lead to decreased cardiac output in systolic heart failure, but they do so in response to a different set of hemodynamic and circulatory environmental factors that depress cardiac output.
In HFpEF, altered relaxation and increased stiffness of the ventricle occur in response to an increase in ventricular afterload . The impaired relaxation of the ventricle then leads to impaired diastolic filling of the left ventricle .
Morris et al found that right venticular subendocardial systolic dysfunction and diastolic dysfunction, as detected by echocardiographic strain rate imaging, are common in patients with HFpEF. This dysfunction is potentially associated with the same fibrotic processes that affect the subendocardial layer of the LV and, to a lesser extent, with RV pressure overload. It may play a role in the symptomatology of patients with HFpEF.
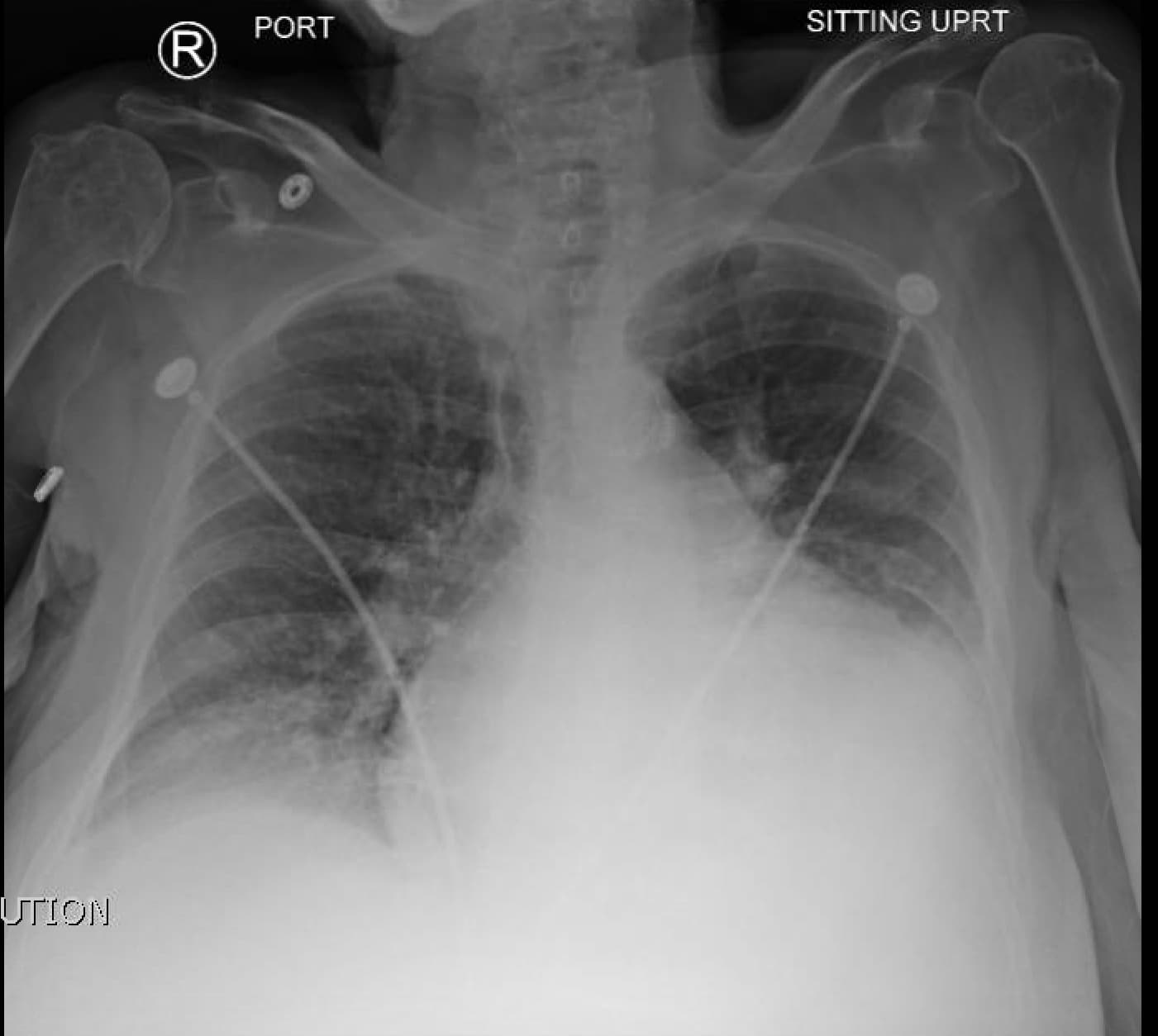
Dilatation Of Azygos Vein
Dilation of the azygos vein is a sign of increased right atrial pressure and is usually seen when there is also an increase in the width of the vascular pedicle.The diameter of the azygos vein varies according to the positioning.In the standing position a diameter > 7 mm is most likely abnormal and a diameter > 10 mm is definitely abnormal.In a supine patient > 15 mm is abnormal. An increase of 3 mm in comparison to previous films is suggestive of fluid overload. The difference of the azygos diameter on an inspiration film compared to an expiration film is only 1mm. This means that the diameter of the azygos is a valuable tool whether or not there is good inspiration.
Don’t Miss: Can Flying Cause Heart Attacks
Why Pulmonary Edema Is A Problem
Pulmonary edema is a serious medical condition that happens when excess fluid begins to fill the lungsâ air sacs . When the alveoli are filled with fluid, they cannot adequately add oxygen to, or remove carbon dioxide from, the blood. So pulmonary edema produces significant breathing difficulties, and may often become a life-threatening problem.
You May Like: Average Exercise Heart Rate
What You Can Do
Some risk factors of heart failure, like age, cant be modified. Still, people with CHF can take steps to improve the long-term prognosis. The first thing to do is to be familiar with any family history of heart disease. You’ll also want to learn about all the possible symptoms. Don’t ignore any symptom that you think is cause for concern. Tell your healthcare provider about them right away.
Regular exercise, along with managing any other health issues you may have, can also help to keep CHF under control.
Also Check: What Is A Heart Attack Definition
Can Chf Cause Copd
Although COPD may lead to CHF, CHF cannot directly cause COPD.
Smoking is by far the most common cause of COPD. However, nonsmokers can also get COPD, particularly if they have long-term exposure to environmental hazards, such as air pollution, dust, fumes, secondhand smoke, and chemicals.
In rare cases, an inherited condition that causes the deficiency of a protein called alpha-1 can lead to COPD.
Researchers have noted several links between COPD and CHF, pointing out that they share similar features, including:
- certain risk factors, such as smoking
- changes in how the lungs and heart function
- some signs and symptoms, such as shortness of breath and difficulty breathing
- both can make the other condition worse
Also, COPD can lead to CHF if the breathing issues that it causes place extra strain on the heart.
According to a 2018 journal paper, COPD and cardiovascular disease often occur together. The authors note that each condition can make the other one worse. They also say that the appropriate treatment of COPD can often have a positive effect on cardiovascular health, which may make it less likely that a person will develop CHF or another form of cardiovascular disease.
Other recommend that healthcare teams monitor people with a diagnosis of one of these conditions for the presence of the other.
Another potentially confounding factor is that doctors may use the same tools to assess the conditions.
Pulmonary Hypertension And Congestive Heart Failure
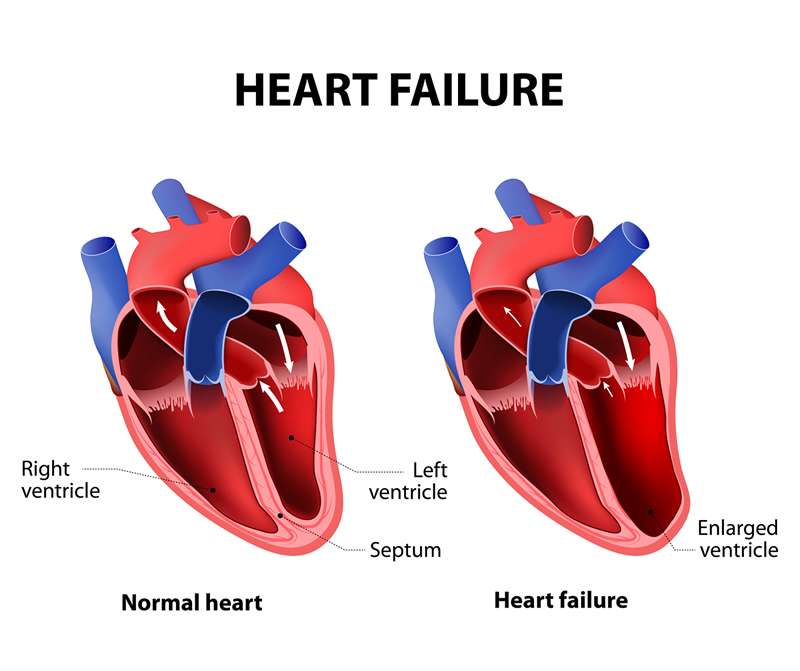
Congestive heart failure is also called heart failure and is the pathophysiological state in which an abnormal cardiac function is responsible for decreased efficiency in the ability of the heart to pump blood. This decreased efficiency and effectiveness leads to a decreased oxygen supply to tissues around the body and subsequent symptoms which can result in death. In order to understand the relationship between pulmonary hypertension and congestive heart failure it is essential that you have a basic understanding of how the heart works.
The heart consists of four separate chambers. The top two chambers are called atria in the bottom two chambers are called ventricles. Blood enters the heart through the right atrium, passes through to the right ventricle where it is pumped out to the lungs through the pulmonary artery. Here the blood picks up oxygen and is carried back to the heart in through the left atrium through the pulmonary vein. The blood then travels into the left ventricle where the heart pumps it out through the aorta to the rest of the body.
In the United States more than 3 million people have congestive heart failure. Individuals who suffer from congestive heart failure and pulmonary hypertension should avoid pregnancy, high altitude, decongestants, beta-blockers and nonsteroidal anti-inflammatory is because they place a large workload on the heart and lungs.
Recommended Reading: When To Be Concerned About Heart Palpitations
Pulmonary Edema Or Pneumonia
Pulmonary edema can overlap with pneumonia, but it is a different condition. Pneumonia is an infection that often occurs as a complication of a respiratory infection, such as the flu.
It can be difficult to distinguish between the two. If the individual or a family member can provide a detailed medical history, this will make it easier for a physician to make the correct diagnosis and provide the right treatment.
The patient will undergo a physical exam first. The doctor will use a stethoscope to listen to the lungs for crackles and rapid breathing, and the heart for abnormal rhythms.
Blood tests will be carried out to determine blood oxygen levels the doctor will often order other blood tests, including:
- electrolyte levels
- blood counts and blood markers of heart failure
An ultrasound of the heart, an echocardiogram, and an electrocardiogram can help determine the condition of the heart.
A chest X-ray may be used to see whether there is any fluid in or around the lungs and to check the size of the heart. A CT scan of the chest may also be ordered.
When Should I Get Emergency Care
Go to the ER or call 911 if you have:
- New, unexplained, and severe chest pain that comes with shortness of breath, sweating, nausea, or weakness
- Fast heart rate , especially if you are short of breath
- Shortness of breath that doesn’t get better if you rest
- Sudden weakness, or you can’t move your arms or legs
- Sudden, severe headache
- Fainting spells
Don’t Miss: What Exactly Is A Heart Attack
What Is Cardiogenic Pulmonary Edema
Cardiogenic pulmonary edema is an accumulation of extra fluid in your lungs that can be life-threatening. This comes from pressure going up and blood collecting on the left side of your heart, usually because of heart failure. In addition to difficulty breathing, cardiac edema can lead to organ damage from a lack of enough oxygen.
Cardiac edema vs. pulmonary edema
Both of these mean you have too much fluid in your lungs, which makes it hard for you to breathe. Cardiogenic pulmonary edema is a type of pulmonary edema with a heart problem as its cause. An injury to your lungs causes the non-cardiogenic type of pulmonary edema.
Cardiac edema vs. renal edema
These are both names for excess fluid in your organs. With cardiac edema, theres too much fluid in your lungs. With renal edema, theres too much fluid in your kidneys. Heart failure can cause both of these. Also, your kidneys cant get enough fluid out of your blood and into your pee.
Q& a: Sequencing Pulmonary Edema And Congestive Heart Failure
Q: What advice do you have for sequencing pulmonary edema and congestive heart failure when both appear to meet the definition of principal diagnosis?
A: The ICD-9-CM guidelines state that when a patient has two or more interrelated conditions that both meet the definition of principal diagnosis, coders may sequence either condition as principal unless the circumstances of the admission, the therapy provided, or the tabular list or alphabetic index indicate otherwise.
Interrelated conditions are those in the same ICD-9-CM chapter. They also include manifestations characteristically associated with a disease process.
Applying this guideline to pulmonary edema and congestive heart failure can be tricky and is often scenario-specific. Consider the following scenarios:
A patient is admitted for pulmonary edema. The physician documents pulmonary edema secondary to end-stage renal disease . The patient also receives treatment for congestive heart failure. Code ESRD as the principal diagnosis.
A patient is admitted for pulmonary edema, congestive heart failure, ESRD, and pulmonary edemaall of which are listed as discharge diagnoses with no indication of the underlying etiology of the pulmonary edema. Query to determine the underlying cause of the pulmonary edema and the chronicity of the pulmonary edema.
A patient is admitted with a history of congestive heart failure and is taking medication. Code the congestive heart failure as a secondary diagnosis.
You May Like: What Cause Low Blood Pressure And High Heart Rate
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Q& A: Sequencing Pulmonary Edema And Congestive Heart Failure
Q: What advice do you have for sequencing pulmonary edema and congestive heart failure when both appear to meet the definition of principal diagnosis?
A: The ICD-9-CM guidelines state that when a patient has two or more interrelated conditions that both meet the definition of principal diagnosis, coders may sequence either condition as principal unless the circumstances of the admission, the therapy provided, or the tabular list or alphabetic index indicate otherwise.
Interrelated conditions are those in the same ICD-9-CM chapter. They also include manifestations characteristically associated with a disease process.
Applying this guideline to pulmonary edema and congestive heart failure can be tricky and is often scenario-specific. Consider the following scenarios:
A patient is admitted for pulmonary edema. The physician documents pulmonary edema secondary to end-stage renal disease . The patient also receives treatment for congestive heart failure. Code ESRD as the principal diagnosis.
A patient is admitted for pulmonary edema, congestive heart failure, ESRD, and pulmonary edemaall of which are listed as discharge diagnoses with no indication of the underlying etiology of the pulmonary edema. Query to determine the underlying cause of the pulmonary edema and the chronicity of the pulmonary edema.
A patient is admitted with a history of congestive heart failure and is taking medication. Code the congestive heart failure as a secondary diagnosis.
Read Also: Which Arm Goes Numb In A Heart Attack
Fast Facts On Pulmonary Edema
- Pulmonary edema is a condition involving fluid buildup in the lungs.
- Sudden onset pulmonary edema is a medical emergency.
- Symptoms include shortness of breath, cough, decreased exercise tolerance or chest pain.
To raise the patients blood oxygen levels, oxygen is given either through a face mask or prongs tiny plastic tubes in the nose. A breathing tube may be placed into the trachea if a ventilator, or breathing machine, is necessary.
If tests show that the pulmonary edema is because of a problem in the circulatory system, the patient will be treated with intravenous medications to help remove fluid volume and control blood pressure.
During normal breathing, the small air sacs in the lungs alveoli fill up with air. Oxygen is taken in, and carbon dioxide is expelled. Pulmonary edema occurs when the alveoli are flooded.
When the alveoli are flooded, two problems occur:
Common causes include:
Systolic And Diastolic Failure
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.
Recommended Reading: Can Lung Cancer Cause Heart Attack
When To Contact A Doctor
A person should contact a doctor if they start to experience symptoms of either COPD or CHF and do not have a diagnosis. A doctor can review a persons health history and test for either condition.
A person living with either condition should work with a doctor to manage their symptoms and ensure that the condition does not lead to other health issues.
COPD and CHF share several similarities, including some of the same symptoms and risk factors.
COPD can make CHF more likely, but CHF cannot directly cause COPD.
A person should talk with a doctor if they experience new respiratory symptoms, such as wheezing or trouble breathing.
A person can take steps to avoid both conditions by managing their weight, quitting smoking, and eating a nutritious, balanced diet.
What Causes Heart Failure
Heart failure is caused by many conditions that damage the heart muscle, including:
- Coronary artery disease.Coronary artery disease , a disease of the arteries that supply blood and oxygen to the heart, causes decreased blood flow to the heart muscle. If the arteries become blocked or severely narrowed, the heart becomes starved for oxygen and nutrients.
- Heart attack. A heart attack happens when a coronary artery becomes suddenly blocked, stopping the flow of blood to the heart muscle. A heart attack damages the heart muscle, resulting in a scarred area that doesnât work the way it should.
- Cardiomyopathy. Damage to the heart muscle from causes other than artery or blood flow problems, such as from infections or alcohol or drug abuse.
- Conditions that overwork the heart. Conditions including high blood pressure, valve disease, thyroid disease, kidney disease, diabetes, or heart defects present at birth can all cause heart failure. In addition, heart failure can happen when several diseases or conditions are present at once.
Also Check: What Can I Do To Slow My Heart Rate Down
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Treatment Of Pulmonary Edema
Pulmonary edema is a serious condition that requires quick treatment. Oxygen is always the first line of treatment for this condition. Your healthcare team may prop you up and deliver 100 percent oxygen through an oxygen mask, nasal cannula, or positive pressure mask.
Your doctor will also diagnose the cause of pulmonary edema and prescribe the appropriate treatment for the underlying cause.
Depending on your condition and the cause of your pulmonary edema, your doctor may also give:
- Preload reducers. These help decrease pressures from the fluid going into your heart and lungs. Diuretics also help reduce this pressure by making you urinate, which eliminates fluid.
- Afterload reducers. These medications dilate your blood vessels and take pressure off your heart.
- Heart medications. These will control your pulse, reduce high blood pressure, and relieve pressure in arteries and veins.
- Morphine. This narcotic is used to relieve anxiety and shortness of breath. But fewer doctors today use morphine due to the risks.
In severe cases, people with pulmonary edema may need intensive or critical care.
In other cases of pulmonary edema, you may need treatment to help you breathe. A machine will deliver oxygen under pressure to help get more air into your lungs. Sometimes this can be done with a mask or cannula, also called Continuous Positive Airway Pressure .
Your doctor may need to insert an endotracheal tube, or breathing tube, down your throat and use mechanical ventilation.
Recommended Reading: How Long Does A Heart Attack Last Before You Die
