Angiotensin Converting Enzyme Inhibitors
ACE inhibitors relax and widen your blood vessels. This helps to improve the flow of blood around your body, which reduces the amount of work your heart has to do.
ACE inhibitors have been shown to improve the symptoms of heart failure, reduce the need for hospital admission and improve life expectancy caused by heart failure.
Your symptoms should improve within a few weeks of starting treatment.
The main side effects of ACE inhibitors are dizziness and a cough. You will need to have regular blood tests, at least once every year, while taking an ACE inhibitor.
If you are taking an ACE inhibitor, you should check with your doctor or pharmacist before taking any other medicines. In particular, nonsteroidal anti-inflammatory medicines should not be taken with an ACE inhibitor. You should also avoid products containing high levels of potassium, such as salt substitutes.
When To Get Medical Advice
See your GP if you experience persistent or gradually worsening symptoms of heart failure.
The symptoms can be caused by other, less serious conditions, so it’s a good idea to get them checked out.
Call 999 for an ambulance or go to your nearest accident and emergency department as soon as possible if you have sudden or very severe symptoms.
This is a medical emergency that may require immediate treatment in hospital.
Page last reviewed: 19 May 2022 Next review due: 19 May 2025
Heart Failure In Women
Heart failure affects increasing numbers of older women, but it’s becoming easier to prevent and treat.
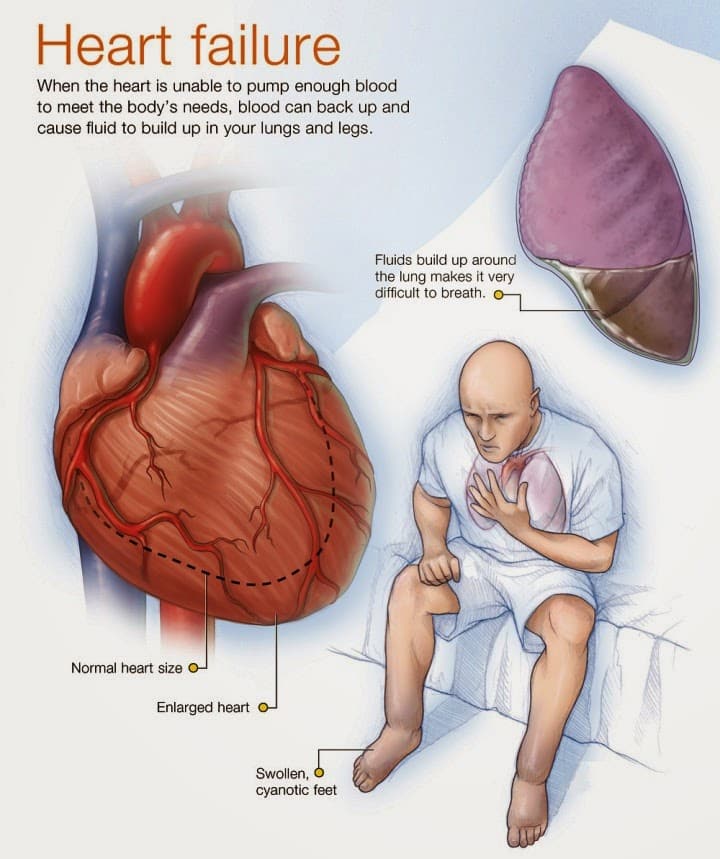
When we think about cardiovascular catastrophes, heart attack and stroke leap to mind. We’re less likely to think of heart failure, though it affects more than 2.5 million women and is the leading reason for hospitalization in women over 65. The term “heart failure” evokes an image of a suddenly silent heart, but the condition is better described as a gradual decline in the heart’s ability to pump and circulate blood.
Like other muscles in the body, the heart weakens over the years. For most people, the effects are subtle: color fades from the cheeks hands grow cold you begin to nod off earlier in the evening. But for the 1% of people over 65 who develop heart failure, a decline in the supply of oxygenated blood to organs and tissues can eventually jeopardize the lungs, kidneys, and liver.
Today, we know that practicing healthful habits earlier in life can often prevent heart failure. And thanks to improved treatments aimed at preserving heart function, women with heart failure can expect to survive longer than in past generations.
Recommended Reading: High Blood Pressure And High Heart Rate
What Makes Yale Medicines Approach To Treating Congestive Heart Failure Unique
Yale Medicines team comprises heart failure cardiologists and cardiac surgeons, dedicated advanced-practice, registered nurses and nurse coordinators, dietitians, exercise physiologists, financial counselors, immunologists specializing in transplants, psychologists, and specialists in palliative care.
With a multidisciplinary approach, Yale Medicine physicians include the patients desires as well as input from the family to develop a comprehensive treatment plan that’s right for them.
Medications For Heart Failure
Certain medications can help treat heart failure and its underlying cause:
- Aldosterone blockers block the effects of the hormone aldosterone, encouraging the body to release sodium and water. They also help prevent scarring in the heart.
- Angiotensin receptor-neprilysin inhibitor : Treatment with sacubitril-valsartan reduces excess fluid in the body and relaxes blood vessels. This makes it easier for your heart to pump blood. Alternatives to ARNIs include angiotensin-converting enzyme inhibitors andangiotensin receptor blockers .
- Beta blockers make the heart beat more slowly and with less force. They also help keep heart rhythm regular.
- Sodium-glucose transport protein 2 inhibitors are diabetes drugs that have recently been found to be very beneficial in heart failure. They help remove glucose via the kidneys into the urine.
Other medications can relieve the heart failure symptoms:
- Diuretics reduce the amount of fluid in the body.
- Vasodilators dilate the blood vessels and reduce the hearts workload.
- Digoxin helps the heart beat stronger with a more regular rhythm.
- Anti-arrhythmics control arrhythmia and maintain normal heart rhythm.
Read Also: What Does Heart Failure Mean
Nyha Functional Classification System
The New York Heart Association functional classification considers heart failure symptoms that happen during exercise to determine stage. Patients can go back and forth between stages depending on how well-controlled symptoms are on a given day.
- Stage 1: The person has heart disease, but it isnt yet causing symptoms or limiting activities.
- Stage 2: The person has mild symptoms that only slightly limit activity.
- Stage 3: The person has significant limitations to activities. He or she is only comfortable when resting.
- Stage 4: The person has major limitations and experiences symptoms when at rest.
Heart Failure Symptoms By Class And Stage
- Bookmark for later
Heart failure is a complex, chronic syndrome that gets worse over time. During the diagnostic process, physicians classify each case of heart failure. The American College of Cardiology/American Heart Association and the New York Heart Association have complementary classification systems.1-4
The ACC/AHA stages reflect the range from a high risk of developing heart failure to advanced heart failure and are associated with an approach to treatment plans.1-4 The New York Heart Association clinical classifications of heart failure reflect the severity of symptoms or functional limits due to heart failure.1-2 A diagnosis can have an assignment of a stage and a class.
Don’t Miss: What Causes Heart Attack In Women
Other Causes Of Heart Failure Include:
- abnormal heart rhythms where your heart beats too fast, too slow or irregularly
- amyloidosis – a build-up of abnormal proteins in organs such as your heart and tissues. When it affects the heart it’s called cardiac amyloidosis – stiff heart syndrome – and can lead to heart failure
- anaemia a lack of red blood cells carrying oxygen in your blood
- congenital heart conditions different heart problems that youre born with
- endocarditis – a viral infection affecting the heart muscle
- heart valve disease – where blood struggles to flow through the heart properly, putting extra strain on the muscle
- pulmonary hypertension – raised blood pressure in the blood vessels that supply your lungs. This condition can damage the right side of your heart, leading to heart failure. Find out more about pulmonary hypertension on NHS Choices and PHA UK
- some cancer treatments, such as chemotherapy
- thyroid gland disease an underactive or overactive thyroid gland which produces too few or too many hormones
- too much alcohol .
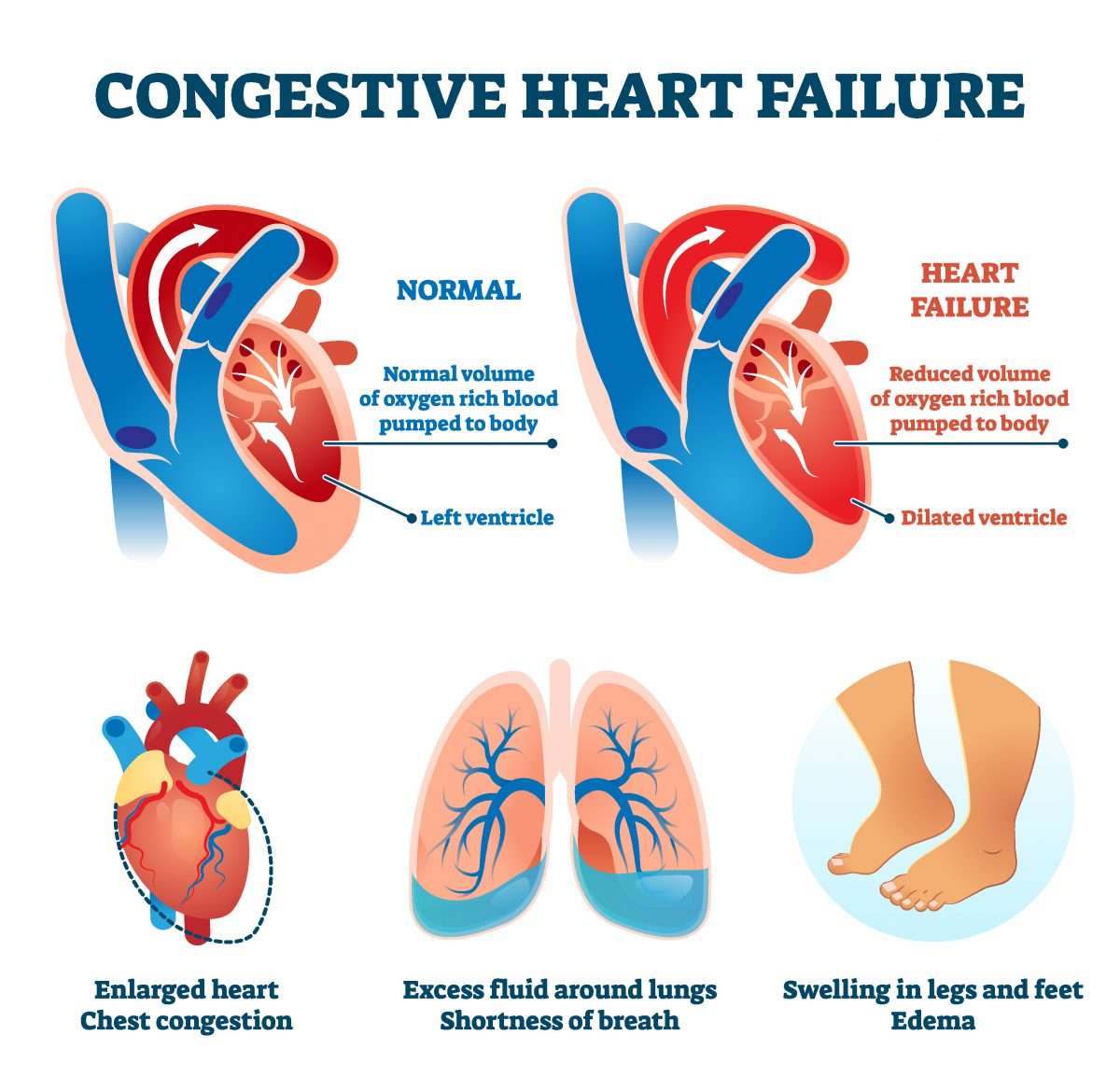
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Also Check: Why Is My Heart Rate Higher On Keto Diet
Women With Heart Failure Are More Likely To Get An Upset Stomach
The report said women with heart failure were more likely than men to report nausea, heart palpitations, an upset stomach, sweating, swelling, pain, depression, anxiety, and a lower quality of life.
Heart failure is diagnosed at a later age in women, and women can have more concurrent illnesses, which may partly explain these differences, the American Heart Association said.
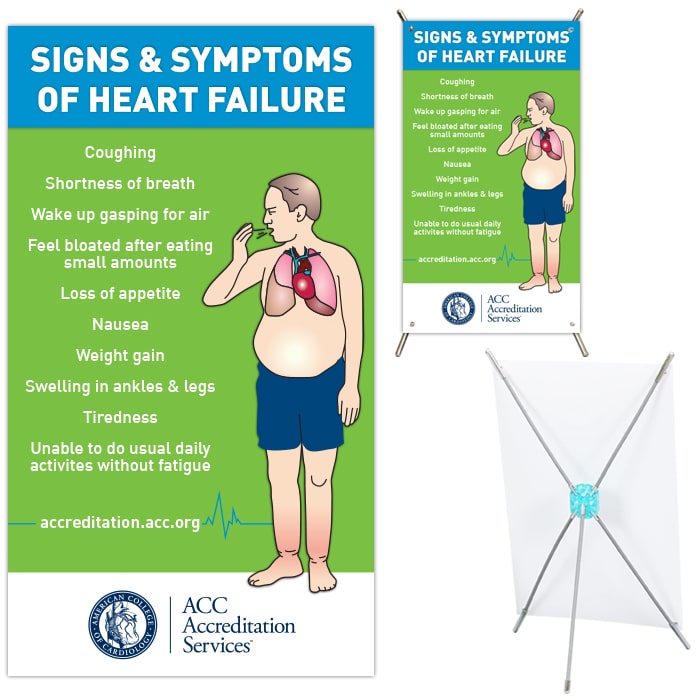
Heart Failure Signs And Symptoms
By themselves, any one sign of heart failure may not be cause for alarm. But if you have more than one of these symptoms, even if you haven’t been diagnosed with any heart problems, report them to a healthcare professional and ask for an evaluation of your heart. Congestive heart failure is a type of heart failure which requires seeking timely medical attention, although sometimes the two terms are used interchangeably.
This table lists the most common signs and symptoms, explains why they occur and describes how to recognize them.
Read Also: How To Determine Max Heart Rate
How Can I Prevent Left
Living a heart-healthy lifestyle can lower your risk of left-sided heart failure. If youve already experienced this condition, healthy habits can help you avoid future issues.
Steps you can take to prevent left-sided heart failure include:
- Get high blood pressure or coronary artery disease under control.
- Make time for regular physical activity and a good nights sleep.
- Maintain a healthy weight and eat fruits and vegetables.
- Manage stress with deep breathing or relaxation techniques.
- Quitting tobacco if you use it and avoiding secondhand smoke.
When To Call A Doctor
Make an appointment to see the doctor if you are experiencing some of the signs or symptoms of heart failure.2,3 Managing an HF condition can involve medications and lifestyle choices including diet and exercise, but the symptoms of heart failure can fluctuate. See your doctor right away if you experience a sudden change and increase in the number of symptoms or a worsening of symptoms.2,3 There may be other underlying causes, medical conditions called comorbidities, that can be exacerbating your HF. Other illnesses like diabetes, lung disease, and chronic kidney disease can cause physiological complications that can be resolved by your health care team.
Recommended Reading: Can Gas Bubbles Feel Like Heart Palpitations
Early Symptoms Of Heart Failure
A person with early heart failure might not have any noticeable signs. When early symptoms occur, they can be subtle and easy to miss or ignore. Early signs of heart failure include:
- Shortness of breath, at first when youre active and later even when youre sitting or lying down
- Lowered ability to exercise or be active
- Confusion or forgetfulness
- Frequent fatigue, sleepiness or weakness
- Palpitations, or a fluttering feeling in your chest, as the heart pumps harder and faster
Without treatment, heart failure can worsen over time. Symptoms that were once mild can become increasingly more severe, and may prevent you from doing everyday tasks.
What Are The Symptoms Of Left
Symptoms may be mild at first or you may think it’s a cold or allergy. You might not even notice them. But as heart functioning worsens, you may experience:
- Constant coughing.
- Shortness of breath with walking or bending over.
- Waking up short of breath or unable to lie flat at night.
- Swelling in your ankles, legs or abdomen.
Over time, the heart works harder to do its job. This causes complications that may include:
- Abnormal heart rates and rhythms .
Read Also: What Is The Heart Rate For A Baby Boy
Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Nutritional deficiencies
What Can You Expect From Heart Failure Treatment
Heart failure treatment is designed to dramatically reduce or halt your symptoms and hopefully prevent potential complications like kidney or liver damage, Dr. Wong says.
There are lots of medications that can be used to treat heart failure. In the early stages, the basic gist is that certain drugs can help to relax blood vessels, lower blood pressure, improve blood flow, and decrease the strain on your heart. Others can help you release extra fluid to keep it from building up in your body. If you progress to more advanced heart failure stages, there are medications that can help strengthen your heart muscle contractions to pump blood more effectively, according to the Mayo Clinic.
Youll likely be encouraged to make some lifestyle changes as well. According to the AHA, that can include things like quitting smoking if you use tobacco, avoiding alcohol, limiting your sodium intake or making other dietary changes, exercising regularly, prioritizing sleep, reducing stress, monitoring your blood pressure, and more.
Your doctor may also recommend certain surgeries or medical procedures if needed in more severe cases, which can include options like coronary bypass surgery, heart valve repair or replacement, a heart transplant, among others, depending on the specific cause of your heart failure.4
You May Like: What Causes Heart Attacks In Women
How Is Congestive Heart Failure Treated
Doctors will assess the current health status of the patient to establish a baseline, and develop a long-term health plan. This may involve the optimization of medicines and therapies, adding new medication, or possibly enrollment in a clinical trial.
Stabilizing and/or reversing a patients condition often involves long-term, collaborative follow-up with a referring cardiologist or physician.
In serious situations, advanced therapies, which include mechanical solutions, a heart transplant, or hospice, may be offered.
What Are Common Heart Failure Risk Factors To Be Aware Of
Heart failure typically develops because the heart has been weakened in some way, according to the Mayo Clinic. It could also happen if your heart becomes too stiff, which prevents it from filling with blood properly between beats, a condition that is more common in people assigned female at birth.
Theres a long list of potential heart failure risk factors because there are many different health issues that can weaken your heart. Here are some of the most common ones to be aware of:
- Coronary artery disease and heart attack
Recommended Reading: Heart Rate Of 120 At Rest
Imaging And Other Tests
Other tests provide pictures of the heart and surrounding structures or show how well the heart is working:
- Electrocardiogram : An electrocardiogram test uses small sensors to measure heart rate , rhythm and electrical impulses.
- Chest X-ray: A chest X-ray is a picture of your lungs, heart and surrounding structures. It can show whether there is fluid in your lungs from heart failure, or if your heart muscle is enlarged.
- Echocardiogram : Echocardiography uses sound waves to create images of your heart. It can show how thick the heart muscle has become, as well as measure ejection fraction.
- MRI: MRI is an advanced imaging test that takes pictures of the heart and surrounding structures. It helps determine your heart function and size and whether there are any changes in the heart muscle. A cardiac MRI may help your doctors identify causes of heart failure.
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
You May Like: Heart Attacks Signs And Symptoms
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
