Conquer All Your Heart Failure Icd
Hint: Report I50.21 for acute systolic heart failure.
Heart failure can be tricky to code because you may see numerous acronyms, and you need to decipher whether its chronic, acute, or acute on chronic. If you dont pay close attention to all of the details in the documentation, you run the risk of reporting the wrong code.
Learn which codes you will report for different types of heart failure to always report clean claims in your cardiology practice.
Differentiate Between Systolic, Diastolic Heart Failure
When a patient has heart failure, their heart does not adequately pump blood to meet their bodys need for blood and oxygen. This, in turn, can cause blood and fluids to back up in the patients body in their lungs, hands, or feet.
Heart failure can be categorized as systolic or diastolic, says Rebecca Sanzone, CPC, CPMA, quality assurance specialist at St. Vincent Medical Group/ Accension Health and coding consultant at the American College of Cardiology.
Systolic heart failure: HFrEF is the acronym for heart failure with reduced ejection fraction, which is also known as systolic heart failure. When a patient has systolic heart failure, the left ventricle of their heart is not able to contract normally, so their heart cant pump with enough force to push enough blood into circulation.
The clinical definition of systolic heart failure is an ejection fraction < 50%, Sanzone explains.
In diastolic heart failure, the ejection fraction > = 50%, Sanzone adds.
Chf Icd 10 Codes And Guidelines
Most of the heart failure codes include in chapter 9 of ICD-10 CM manual, diseases of circulatory system, code range I00-I99.
- Combination code If patient has any type of heart failure and hypertension, it should be combined and coded as I11.0 eventhough physician has not linked both. It should not be coded combined if the medical record states the conditions are unrelated.
- Heart failure should be coded additionally when coding I11.0
- Do not code I11.9 when coding I11.0 .
- When coding biventricular heart failure it is necessary to code the type of left heart failure also according to the code also note with I50.82
Go by Failure, Heart to find correct codes for heart failure in ICD-10 CM manual index.
Look at the below scenarios to clearly understand the coding concepts of CHF.
CHF ICD 10 Code Example 1
Elizabeth is a 65 year old female who comes to emergency department for shortness of breath and leg edema from past 2 days. She came to visit doctor as the symptoms are getting worse. She has hypertension and takes Lisinopril for the same. She does not have chest pain or palpitation. She is not a smoker. Her family history includes heart disease for her mother and brother. Vitals showed temperature 97.3 F, heart rate 72 bpm, respiratory rate 25, BP 150/96 mmHg. Physical exam showed pitting edema on both the extremities, shortness of breath and dry skin. Physician ordered for blood tests, EKG and chest X-ray. This case was diagnosed as acute diastolic heart failure.
Warning Signs Of Worsening Systolic Heart Failure
Systolic heart failure can worsen gradually over time or quickly. Your doctor will explain the warning signs that systolic heart failure is getting worse. They may include any symptoms that intensify, such as:
- Cough that wont go away
- Dizziness, confusion or fainting
- Sudden increase of swelling in the belly, legs, ankles or feet
- Weight gain of 3 or more pounds in one day or 5 or more pounds in one week
You should always report worsening heart failure symptoms to your doctor. Quick treatment can help prevent complications of systolic heart failure, which include:
- Damage to the kidneys and liver
- Right-sided heart failure, which damages the right ventricle and leads to combined systolic and diastolic heart failure symptoms
Careful management is key to slowing the progression of systolic heart failure and preventing complications. You should be sure to attend all your follow-up appointments, follow your treatment plan and take all your medications as prescribed.
Also Check: How To Measure Heart Rate On Iphone
Unspecified Systolic Heart Failure
- 2016201720182019202020212022Billable/Specific Code
- I50.20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM I50.20 became effective on October 1, 2021.
- This is the American ICD-10-CM version of I50.20 – other international versions of ICD-10 I50.20 may differ.
- Applicable To annotations, or
Seattle Heart Failure Model
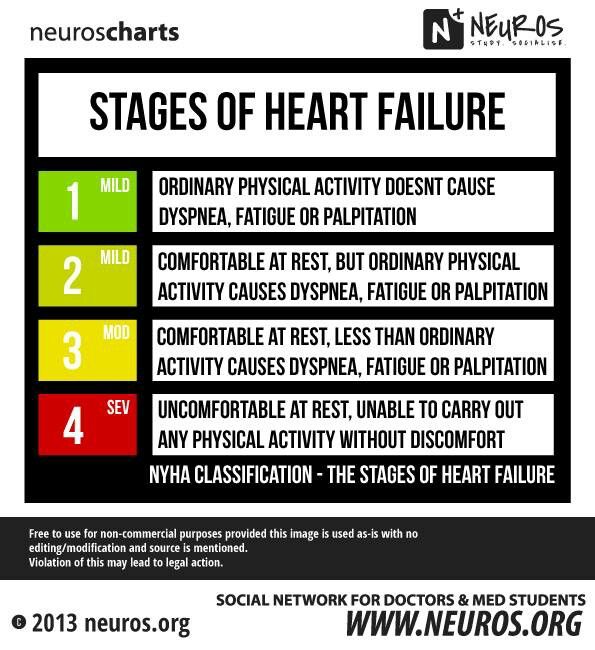
2 days agoNYHA Class 1. BiV Pacer/ICD. Same as BiV pacer. LVAD. NYHA Class 4 and. EF 25% and. Mean 2 year survival 50%. If you want to see the effect in the model anyway, make the patient characteristics match the criteria, then click on the device you want, then set the patient criteria back to the original values.
Read Also: What Is The Difference Between Heart Rate And Blood Pressure
Don’t Miss: Congestive Heart Failure In Espanol
Determine The Cause Of Heart Failure
One of the most important things you understand, when coding for heart failure, is that there can be many very different reasons why somebody can develop heart failure, and the ICD-10-CM coding system, as complex as it is, allows for very fine granuation in this respect. Therefore, your first decision to make, when looking for a code to use, is to determine, from the note, what is the underlying cause for heart failure. To illustrate, I am listing a few of the more common ICD-10 codes for heart failure based on cause:
- I11.0 Hypertensive heart disease with heart failure
- I09.81 Rheumatic heart failure
- I97.131 Postprocedural heart failure following other surgery
- I97.130 Postprocedural heart failure following cardiac surgery
- I13.0 Hypertensive heart and chronic kidney disease with heart failure and stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease
- P29.0 Neonatal cardiac failure
Note that none of the above conditions where heart failure is present use the root I50 for buidling the ICD-10 code.
Donât Miss: Which Part Of The Brain Controls Blood Pressure, Heart Rate And Respiration
Chronic Systolic Chf Icd 10
The Chronic Systolic CHF ICD 10 code is I50.22. The third code in this category as chronic systolic heart failure I50.22 is the code of choice here. The main code has excluded notes beneath it that states that a code cannot be used here if there is a combination of the acute and chronic condition of systolic/diastolic heart failure.
- Pulmonary edema with heart disease NOS
- Pulmonary edema with heart failure
- edema of lung without heart disease or heart failure
- pulmonary edema without heart disease or failure
Don’t Miss: What Takes Blood Away From The Heart
Matters Of The Heart: Fy2018 Code Changes Impacting Heart Failure
C. Matheson, RHIA, CCS CDI
Heart failure is a serious medical condition that an estimated 5.7 million Americans are diagnosed with. This is a condition that occurs when the heart muscle cannot pump enough blood and oxygen needed by the body to support the other organs. According to the Center for Disease Control, the national estimated cost to treat heart failure is nearly $31 billion each year. As new technology and advancements in treatment progresses, ICD-10-CM and PCS changes can keep up the pace to appropriately categorize and capture accurate disease data. FY2018 ICD-10-CM code changes brought forth an onslaught of new and revised codes. One diagnosis category to receive updates and new expansion is in Heart Failure. This brief article will discuss the high level changes impacting heart failure coding.
A new subcategory was created to uniquely identify several different types of heart failure. I50.8, Other Heart Failure, was created to delineate other very specific cases of heart failure, such as these below:
- I50.810 Right heart failure, unspecified
- I50.811 Acute right heart failure
- I50.812 Chronic right heart failure
- I50.813 Acute on chronic right heart failure
- I50.814 Right heart failure due to left heart failure
- I50.82 Biventricular heart failure
What Is The Main Term For Congestive Heart Failure
Congestive Heart Failure Congestive heart failure is a chronic progressive condition that affects the pumping power of your heart muscle. While often referred to simply as heart failure, CHF specifically refers to the stage in which fluid builds up within the heart and causes it to pump inefficiently.
Donât Miss: Congestive Heart Failure End Stages
Don’t Miss: Does Magnesium Help With Heart Palpitations
Heart Failure With Reduced Ejection Fraction
Systolic heart failure is also called heart failure with reduced ejection fraction .
Ejection fraction is the percentage of blood the left ventricle pumps out with every beat. A normal, healthy ejection fraction is 55% to 65%. If its higher or lower, that can indicate a heart problem.
With systolic heart failure, the ejection fraction is usually less than 50%.
Is Hfmref Systolic Or Diastolic
A new term, HFmrEF, has been introduced when the EF is 41-49 and coded as systolic failure. HFrecEF describes a significant improvement in a reduced EF usually following TAVR. If recovered to > =50% it is coded as diastolic if < 50% it ought to constitute improved, but persistent, systolic failure.Oct 6, 2020
Don’t Miss: Do Heart Palpitations Make You Cough
Acute Systolic Heart Failure Versus Chronic Systolic Heart Failure
Systolic heart failure can be classified as acute or chronic:
- Acute: You have active symptoms of heart failure with a new diagnosis or a long-term condition.
- Chronic: You have a history of heart failure, but are relatively stable.
Acute systolic heart failure is a medical emergency. Depending on the cause, some cases can be reversed with prompt treatment. Chronic systolic heart failure is a lifelong condition, and treatment aims to slow the disease and minimize symptoms.
What Is Diastolic Chf
Diastolic heart failure occurs when a heart is unable to relax fully, making ventricles deprived of enough blood to pump the blood to other organs. The volume and pumping force decreases significantly making the heart as well as other body areas deprived of oxygenated blood significantly. Doctors use different medications as well as surgical options to treat this condition.
Also Check: Congestive Heart Failure Age 30
Acute On Chronic Diastolic Chf Icd 10
The Acute On Chronic Diastolic CHF ICD 10 code is I50.33.
When looking at diastolic under failure/heart in the alphabetic index, the ICD 10 system provides subcategory I50.3 for diastolic heart failure. Under this category, several codes according to different specified descriptions are provided I50.33 at the bottom of this subcategory is the code of choice to fully describe the condition acute on chronic diastolic heart failure.
Symptoms Of Congestive Heart Failure
Heart failure can be ongoing , or your condition may start suddenly . Heart failure signs and symptoms may include shortness of breath when you exert yourself or when you lie down, fatigue and weakness, swelling in your legs, rapid or irregular heartbeat, reduced ability to exercise, persistent cough or wheezing with white or pink blood-tinged phlegm, increased need to urinate at night, swelling of your abdomen , very rapid weight gain from fluid retention, lack of appetite and nausea, difficulty concentrating or decreased alertness, sudden or severe shortness of breath and coughing up pink and foamy mucus, and chest pain if your heart failure is caused by a heart attack
Also Check: Why Do I Have Heart Palpitations When I Lay Down
Treatment For Congestive Heart Failure
There are several medications that can be used to treat CHF. The first is ACE inhibitors. Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cannot tolerate ACE inhibitors. ACE inhibitors shouldnt be taken with the following medications without consulting with a doctor, because they may cause an adverse reaction. The second type of medication is beta-blockers. Beta-blockers can reduce blood pressure and slow rapid heart rhythm. Beta-blockers should be taken with caution with the following medications, as they may cause an adverse reaction. The third type of medication is diuretics. Diuretics reduce your bodys fluid content. CHF can cause your body to retain more fluid than it should. Thiazide diuretics cause blood vessels to widen and help the body remove any extra fluid. Loop diuretics cause the kidneys to produce more urine. This helps remove excess fluid from your body. Potassium-sparing diuretics help get rid of fluids and sodium while still retaining potassium. If medications arent effective on their own, more invasive procedures may be required. Angioplasty, a procedure to open up blocked arteries, is one option. Your cardiologist may also consider heart valve repair surgery to help your valves open and close properly.
The table below includes the most commonly used ICD-10 codes for Congestive Heart Failure:
| ICD-10 Chapter |
|---|
Can You Have Combined Systolic And Diastolic Heart Failure
There is increasing recognition that disorders of both left ventricular systolic and diastolic function can result in congestive heart failure. As such, consideration of both the filling and emptying characteristics of the left heart is needed to evaluate the hemodynamic abnormalities present in this syndrome.
Read Also: Early Heart Attack Signs
Chronic Diastolic Chf Icd 10
Chronic CHF has the same subcategory to find the right code for this description. I50.33 is the second last code of this subcategory that states Chronic diastolic heart failure is most appropriately describing this condition.
According to CMS guidelines, verifying each code in the tabular index of CPT code and/or using a coding tool, there must be a complete description against each code with matching keywords and synonyms. The ICD 10 code for chronic CHF diastolic is I50.33.
What Is The Condition Called When The Heart Is Decompensated
Acute decompensated heart failure is a sudden worsening of the signs and symptoms of heart failure, which typically includes difficulty breathing , leg or feet swelling, and fatigue. ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart. An attack of decompensation can be caused by underlying medical illness, such as myocardial infarction, infection, or thyroid disease.
Recommended Reading: What Causes A Fast Heart Rate
Causes Of Systolic Heart Failure
Systolic heart failure is usually caused by another cardiovascular condition that weakens the heart muscle. For example:
- Aortic stenosis, a narrowing of the valve in the large blood vessel that branches off the heart
- Arrhythmia, an irregular heart rhythm
- Cardiomyopathy, any condition affecting the heart muscle
- Coronary artery disease, narrowing of the blood vessels that bring blood to the heart
- Heart attack, which occurs when the heart doesnt get enough blood
- High blood pressure , the force of blood pushing against arteries
- Mitral regurgitation, when a valve in the heart doesnt close tightly, allowing blood to flow backward in the heart
- Myocarditis, inflammation of the heart muscle
Fransoo Et Al And Fransoo Et Al
- In The 2013 RHA Indicators Atlas by Fransoo et al. and The 2019 RHA Indicators Atlas by Fransoo et al. residents were considered to have CHF if they met one of the following conditions:
- one or more inpatient hospitalizations in one year with a diagnosis for CHF: ICD-9-CM code 428 or ICD-10-CA code I50 OR
- two or more physician visits in one year with a diagnosis for CHF .
Only Manitoba residents aged 40 and older were included.For more information, please see:
Recommended Reading: What Should Resting Heart Rate Be For A Woman
Medications To Lessen Symptoms Of Systolic Heart Failure
Many of the symptoms of systolic heart failure are uncomfortable, and may limit the amount and type of activities you can participate in. Your doctor may recommend medications that treat the symptoms of systolic heart failure to make you more comfortable. Some of these options include:
- Diuretics reduce the amount of fluid in the body.
- Vasodilators dilate the blood vessels and reduce the hearts workload.
- Digoxin helps the heart beat stronger with a more regular rhythm.
- Anti-arrhythmics control arrhythmia and maintain normal heart rhythm.
Complications & Comorbid Conditions Rules For I5023
When I50.23 is used as a secondary diagnostic code, the patients visit may be considered to have Complications & Comorbid Conditions or Major Complications & Comorbid Conditions .
Exclusions apply. When the primary diagnostic code is is in the exclusion list, the patient visit CC/MCC does not qualify for a CC or MCC.
CC/MCC grouping rules are adjusted each year, so check the rules for the fiscal year of the patients discharge date.
Read Also: What Causes Heart Palpitations At Night
Diseases Of The Circulatory Systemtype 2 Excludes
- 2016201720182019202020212022Non-Billable/Non-Specific Code
Code First
- 2016201720182019202020212022Non-Billable/Non-Specific Code
Applicable To
- end stage heart failure, if applicable
- combined systolic and diastolic heart failure
- Heart failure caused by abnormal myocardial contraction during systole leading to defective cardiac emptying.
Applied Behavior Analysis Medical Necessity Guide
The Applied Behavior Analysis Medical Necessity Guide helps determine appropriate levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. The ABA Medical Necessity Guide does not constitute medical advice. Treating providers are solely responsible for medical advice and treatment of members. Members should discuss any matters related to their coverage or condition with their treating provider.
Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member’s benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply.
The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered for a particular member. The member’s benefit plan determines coverage. Some plans exclude coverage for services or supplies that Aetna considers medically necessary.
Please note also that the ABA Medical Necessity Guide may be updated and are, therefore, subject to change.
You May Like: Low Heart Rate When Sleeping
