Talk To Them About Their Symptoms
People with heart failure may feel worried about their symptoms, treatment or risk of dying suddenly. Reassure them by talking openly and honestly about their concerns. Speak to their cardiac or palliative care team if you need support. If the patient has a plan for managing symptoms or emergencies, they may feel less anxious.
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
End Stages Of Heart Failure: What To Expect
Congestive heart failure is one of the most common reasons for hospital admissions for senior citizens. In fact, over 5 million adults in the United States experience heart failure.
Heart failure occurs when the heart muscle becomes damaged and can no longer pump blood effectively. Although symptoms can be managed, this is a chronic condition with no cure. In time, patients will reach the final stages of congestive heart failure.
Patients in the end stages of heart failure want to know what to expect. The symptoms of end-stage congestive heart failure include dyspnea, chronic cough or wheezing, edema, nausea or lack of appetite, a high heart rate, and confusion or impaired thinking.
You May Like: Life Expectancy With Heart Failure
Helping Individuals With End
According to the National Hospice and Palliative Care Organization, heart disease is on the rise in the United States. Additionally, the disease comes with a high symptom burden, specifically at the end-of-life. Therefore, individuals with end-stage heart disease and congestive heart failure can benefit from hospice services.
Hospice of Southern Illinois focuses on comfort care for individuals with heart disease and CHF rather than curative treatment. Keeping in mind that your loved ones wishes are most important, our team including the medical director, pharmacist, nurse practitioner, nurses, social workers, counselors, hospice aides and volunteers will work together to create an individualized plan of care to reduce pain and keep symptoms managed, including but not limited to, chest pain, shortness of breath and fatigue. We will cover medications, equipment and services related to the patients terminal prognosis. Contact us today for more information on hospice for CHF, care for individuals with heart disease, and care for advanced heart failure. No one has to go through the dying process alone. Hospice of Southern Illinois is here to help.
Hospice Care For Heart Disease Patients
If you are reading this, it is likely you or someone you love has been waging a difficult physical and emotional battle against heart failure or some form of heart disease. Your search for comfort, support and answers does not stop when you accept that you must learn to live with heart disease. Thats when VITAS can help.
Hospice helps patients and their families deal with the significant impact of heart disease after curative treatment has stopped. On this page, weve provided answers to these questions:
- When is the right time to ask about hospice?
- What can hospice do for a person with heart disease?
- What can hospice do for the family of a person with heart disease?
- What are the overall benefits of hospice care?
- How can I approach my hospice discussion with family members and loved ones?
Don’t Miss: How Common Are Heart Attacks In Your 20s
Hospice For Heart Disease & End
If you are reading this, it is likely you or someone you love has been waging a difficult physical and emotional battle against heart failure or some form of heart disease. Your search for comfort, support and answers does not stop when you accept that you must learn to live with heart disease. Thats when VITAS can help.
Hospice helps patients and their families deal with the significant impact of heart disease after curative treatment has stopped. On this page, we’ve provided answers to these questions:
- When is the right time to ask about hospice?
- What can hospice do for a person with heart disease?
- What can hospice do for the family of a person with heart disease?
- What are the overall benefits of hospice care?
- How can I approach my hospice discussion with family members and loved ones?
When To Seek Help
Patients with a life expectancy shorter than six months are eligible for hospice care. A hospice provides additional aid and resources to assist the person in living comfortably and with the highest possible quality of life. Hospice caregivers can also help patients and their families plan for future needs and circumstances. They have a unique insight into how to assist those with these difficulties.
Patients with end-stage heart failure need medical continuity throughout outpatient programs. These are just some of the symptoms that hospice care might help with. Positive inotropic drug infusions, anxiolytics, and sleeping medicines are all viable treatments. Its challenging for patients, families, and doctors caring for patients with end-stage heart failure to identify when treatment goals shift from survival to quality of life, allowing for a peaceful and dignified death.
Read Also: How To Tell If Heart Attack Is Coming
Hospice And Congestive Heart Failure
When a heart failure patient has been diagnosed with six months or less to live, the added support of hospice care helps them remain in their home until end of life.
Crossroads Hospice & Palliative Care provides a team of nurses, aides, social workers, volunteers, and chaplains to support the patient and their family through the final stages of congestive heart failure symptoms. To learn more about referring your patient to hospice, please call Crossroads at 1-888-564-3405.
Living With Heart Failure
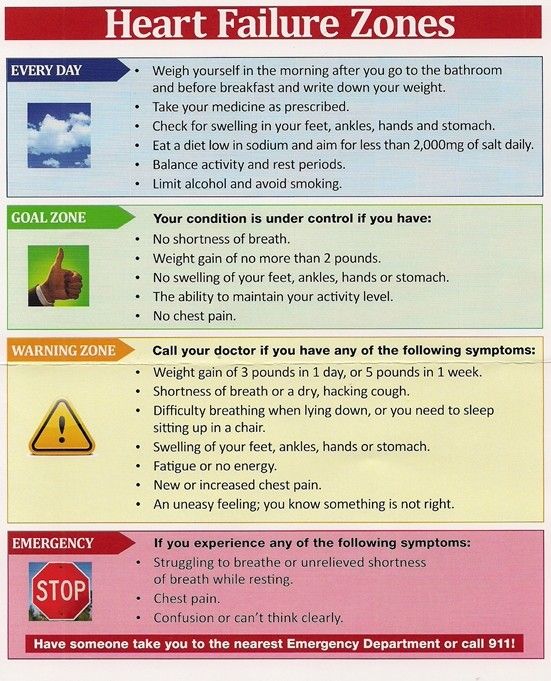
There are five things patients diagnosed with heart failure need to do every day at home to manage their heart failure. The following MAWDS acronym may help you remember and follow these basic steps:
- Medications: Take your medications as prescribed by your doctor and heart care team, let them know if you dont tolerate your medications and dont run out of them.
- Activity: Stay active every day, do what you can to keep your body strong.
- Weight: Weigh yourself each day, recognize when changes in your weight mean you are retaining more fluid.
- Diet: Follow your die, that means low salt and limit fluid intake .
- Symptoms: Recognize your symptoms and know when to call for help.
Recommended Reading: How Does A Heart Attack Affect The Body
What To Do If Your Cat Has Stage D Congestive Heart Failure
There are medications your vet can use to help your cat feel more comfortable and to treat these early symptoms. Stage D Stage D indicates moderate congestive heart failure, and long-term treatment is necessary. Medications are prescribed to reduce fluid retention and inflammation of the veins that are both common in stage D.
Congestive Heart Failure: Prevention Treatment And Research
Congestive heart failure is a serious condition in which the heart doesnt pump blood as efficiently as it should. Despite its name, heart failure doesnt mean that the heart has literally failed or is about to stop working. Rather, it means that the heart muscle has become less able to contract over time or has a mechanical problem that limits its ability to fill with blood. As a result, it cant keep up with the bodys demand, and blood returns to the heart faster than it can be pumped outit becomes congested, or backed up. This pumping problem means that not enough oxygen-rich blood can get to the bodys other organs.
The body tries to compensate in different ways. The heart beats faster to take less time for refilling after it contractsbut over the long run, less blood circulates, and the extra effort can cause heart palpitations. The heart also enlarges a bit to make room for the blood. The lungs fill with fluid, causing shortness of breath. The kidneys, when they dont receive enough blood, begin to retain water and sodium, which can lead to kidney failure. With or without treatment, heart failure is often and typically progressive, meaning it gradually gets worse.
More than 5 million people in the United States have congestive heart failure. Its the most common diagnosis in hospitalized patients over age 65. One in nine deaths has heart failure as a contributing cause.
Also Check: What Should Heart Rate Variability Be
What To Do If Your Cat Has Stage B Heart Disease
In stage B, the heart problem has been detected, but the cat is not yet showing symptoms. Sometimes medications like beta blockers are prescribed, but often the animal is just observed carefully for signs of progression. Stage C During stage C heart disease, there are obvious symptoms that suggest congestive heart failure in your cat.
Systolic And Diastolic Failure
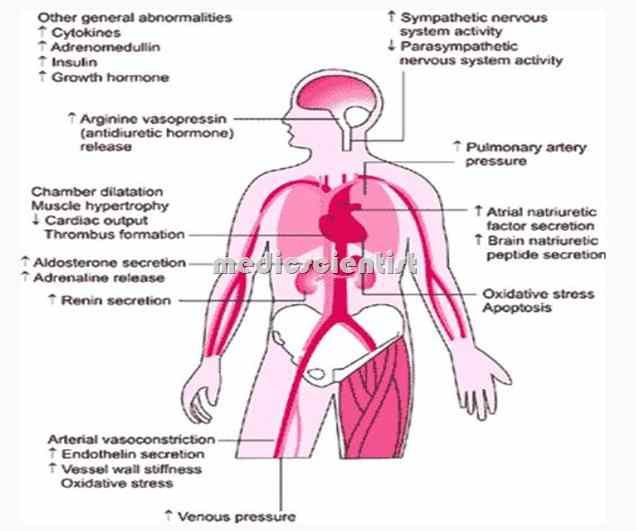
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.
Also Check: Medicine For Congestive Heart Failure
Risk Factors For Heart Failure
Health conditions that left unrecognized or untreated will increase the lifetime risk of developing heart failure. Some of these diseases include:
- Coronary heart disease and heart attacks
- High blood pressure
Unhealthy behaviors can also increase your risk for heart failure, especially for people who have one of the diseases listed above. Unhealthy behaviors include:
- Smoking or using tobacco
- Use of illegal drugs, like methamphetamines or even excessive alcohol intake
- Eating foods high in fat, cholesterol, and sodium
- Not getting enough physical activity
Life Expectancy Of Heart Failure In Dogs
Unfortunately, there is no cure for congestive heart failure in dogs.
Medical management can be effective in offering a dog more time, and making their life more comfortable as their disease progresses.
Though there is no known cure for CHF, daily medication and lifestyle changes can add significant time to their life.
If your dog has been diagnosed in the early stages of their heart failure, they may have anywhere from 1 to 3 years.
Early detection along with proper medical care can significantly improve a dogs prognosis.
However, if your dog is diagnosed with CHF when they have begun to display serious symptoms, their time may be limited.
These pups typically have a life expectancy of 1-6 months, and will need to be monitored closely for any sign of suffering.
Recommended Reading: Why Does Alcohol Increase Heart Rate
You May Like: Right And Left Side Heart Failure
What Are The Main Causes Of Heart Failure
Heart failure can have many causes. The most common causes are:
- Coronary heart disease this is where the arteries that supply blood to the heart become clogged up with fatty substances called atherosclerosis which may cause symptoms of chest discomfort called angina or heart damage from a heart attack.
- Hypertension high blood pressure can put extra strain on the heart, which over time can lead to heart failure.
- Cardiomyopathy conditions affecting the heart muscle and can be hereditary or acquired condition that causes the changes in the heart muscle tissue leading to failure of function.
- Arrhythmias heart rhythm problems such as atrial fibrillation which impairs the contraction strength of the heart by the persistent fast heart rate is one of the many rhythm disturbances causing the heart to pump less efficiently.
- Heart valve disease valve defects and damage will increase volume and strain on the heart and weaken it.
- Congenital heart disease birth defects that affect the normal workings of the heart.
- Metabolic hyperthyroid with overactive thyroid and diabetes are endocrine causes of heart failure.
- Toxicity alcohol and certain chemotherapy drugs can be toxic to the muscle cells and damage their function.
Caring For Someone With Heart Failure Towards The End Of Life
Please be aware this information is for healthcare professionals.
You can use our My Learning form to reflect on how this page has helped with your continuing professional development.
If youre a patient, or a family member or friend, you can find more information on heart failure from the British Heart Foundation .
Heart failure means the heart is not pumping blood around the body as well as it should. People with heart failure may have symptoms such as fatigue, breathlessness and oedema . Here, well talk about knowing when a patient with heart failure is near the end of life, and how to support them.
This information is about supporting adults with advanced heart failure.
On this page:
Also Check: How Long Does A Heart Attack Take
Also Check: Dog Diuretic Congestive Heart Failure
What Are The Stages Of Congestive Heart Failure In Cats
In stage A, a cat has heart disease, but doesnt have any symptoms. Stage B is when heart disease is present, but there arent any occurring symptoms. In stage C, heart disease symptoms have manifested themselves. Stage D is when a cat is experiencing congestive heart failure and treatment is necessary.
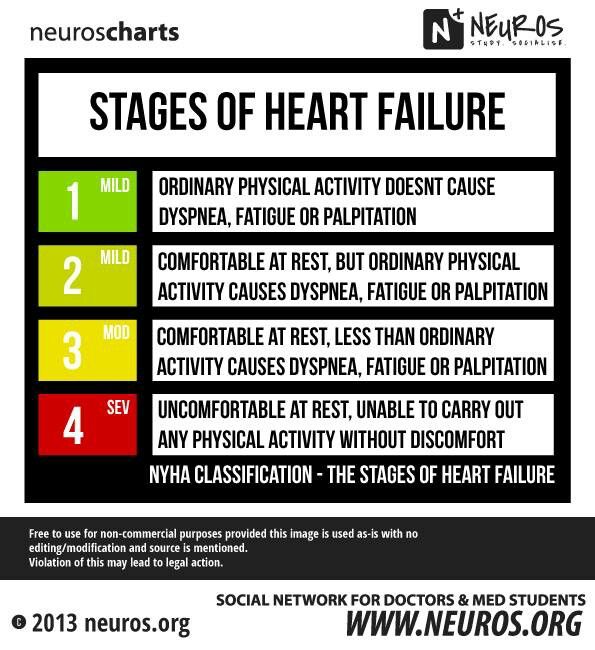
Stage 3 Of Congestive Heart Failure
Its not uncommon for congestive heart failure to be accompanied by other heart conditions. If you are diagnosed with stage three CHF, along with another heart condition, its likely that youll have difficulty performing regular tasks. Small bouts of exercise or minimal doses of physical activity will cause the same symptoms mentioned in stage two fatigue, shortness of breath, and heart palpitations. In stage three, lifestyle changes are not as effective, and a surgical procedure may be necessary. However, its never too late to talk to a doctor about your heart condition and what the future may look like.
Don’t Miss: What Is The Normal Heart Rate For Pregnant Woman
What Do Symptoms Of End Stage Congestive Heart Failure Look Like
Dyspnea
Dyspnea or shortness of breath can occur both during activity and rest. This is the symptom that often sends patients racing to the hospital late at night. Work with your hospice or palliative care team to manage symptoms at home and avoid these stressful hospital trips.
Chronic Cough
When the heart cannot keep up with the supply of blood moving between it and the lungs, fluid can build up in the lungs. This results in a chronic cough or wheezing that can produce white or pink mucus.
Edema
As the hearts ability to pump slows down, fluid can build up in the body. This creates swelling in the extremities particularly the feet, ankles, legs, or abdomen.
Lack of Appetite
As the digestive system receives less blood, patients may feel full or nauseous. Not wanting to eat is a natural part of the body shutting down, but families often find this distressing. Learn more about why it is okay for your loved one to stop eating and drinking at end of life.
High Heart Rate
In response to a loss in pumping capacity, the heart begins to beat faster. The patient experiences this as a racing or throbbing heartbeat.
Confusion
When the heart stops working effectively, it can change sodium levels in the blood. This leads to memory loss, confusion, and a general feeling of disorientation.
Both Are Chronic And Have Periodic Flare
Each of these conditions is chronic and cannot be cured. But you can have periods of relative stability when symptoms are not too bothersome. At times, though, the symptoms can worsen or flare-up. This is called an exacerbation.
The difference is what causes these exacerbations. With COPD, triggers are often environmentally-related:
- Exposure to germs that cause respiratory infections
- Breathing in cold dry air
- Exposure to air pollution
- Inhaling strong fumes or smoke
With CHF, factors that cause flare-ups are often more related to lifestyle or other health issues.
- Eating the wrong foods, for example, too many salty foods
- Drinking too much water
- Having a heart attack or stroke
In both cases, exacerbations can also occur when medications are not taken as prescribed.
Read Also: Treatments Of Congestive Heart Failure
How Can Hospice Help Heart Disease And Heart Failure Patients
Many patients will have lived with congestive heart failure for a long time before reaching the point where hospice is considered. It is important to understand that even though treatment can no longer be given to lengthen a persons life significantly, there are still ways that their quality of life and comfort can be increased, and that is where hospice can prove valuable.
Hospice care is given to patients who are expected to live for six months or less. Although it may be difficult to determine just how long patients with this condition will live, worsening symptoms and deliberately turning down the opportunity to get life-extending treatment are both signs it is time to give hospice serious consideration.
It is important not to wait too long to contact hospice most families report that they wish they had started it sooner after seeing how much it helps. If you suspect your loved one is ready for hospice, talk to your doctor and request a hospice evaluation.
