Palliative And Hospice Care
Someone living with a serious condition like heart failure can access palliative care at any stage of their condition. Palliative care is intended to support overall wellness and quality of life and can happen alongside other treatments.
With very severe heart failure, people may choose to access hospice care to receive supportive care at the end of life.
Acute Heart Failure Diagnostic Workup
The diagnostic workup for acute heart failure begins with a rapid assessment of the patients health history, including a detailed account of any symptoms, history of heart disease in the family, whether the patient smokes, what medications they take, and if they have any other medical conditions.
The physical examination should be comprehensive. Patients with acute decompensated heart failure will present a general appearance that includes anxiety, diaphoresis, and poor nutritional status.6
Physicians often use the Framingham Diagnostic Criteria for Heart Failure, which requires the presence of either two major criteria or one major and two minor criteria to make the diagnosis.5 The criteria are as follows:5
Description Of The Problem
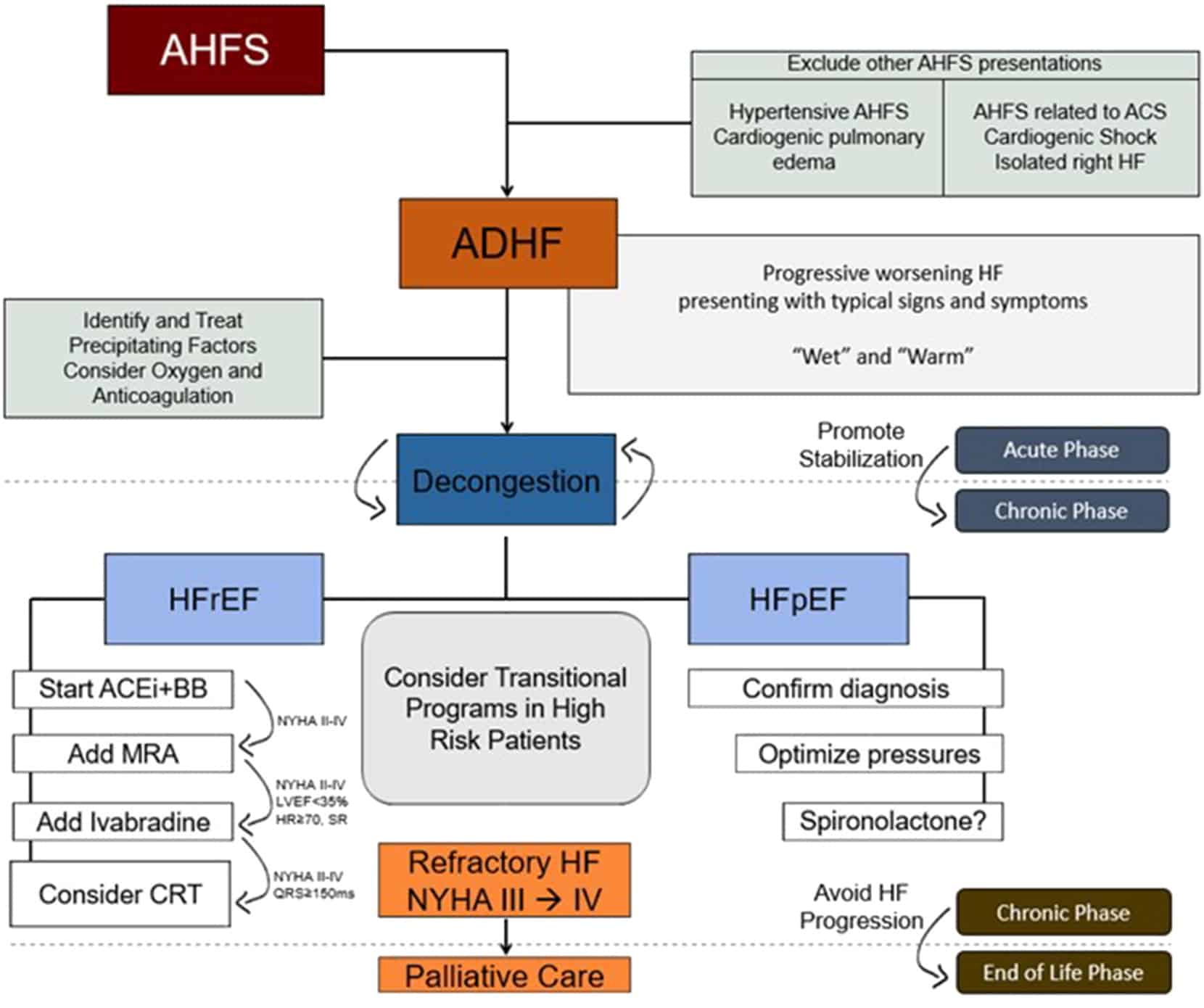
Acute heart failure is a complex clinical syndrome that results from the inability of the heart to meet the metabolic demands of the body. This disease is quite prevalent: over 5 million people have heart failure in the United States alone. There are nearly 300,000 deaths from heart failure annually, and well over 1 million hospitalizations for heart failure each year.Patients often present to their clinician with a variety of signs and symptoms. Most of these are related either to vascular congestion or impaired perfusion. Common signs and symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea , peripheral edema, nausea/vomiting, weight gain or weight loss, elevated jugular venous pressure, hepatomegaly, pulmonary rales, cardiac gallops , and pleural effusions, to name a few.The goal for managing a patient with acute decompensated heart failure is several-fold: 1) Identify an etiology for the decompensation, 2) Decongest the patient , 3) Ensure adequate perfusion to vital organs, and 4) Preserve hemodynamic stability.
You May Like: Apple Watch Heart Rate Zones
Summary Compensated Vs Decompensated Heart Failure
Adaptive changes in the cardiac tissues maintain an optimal cardiac output although the damages to the myocardium in heart failure is known as the compensated heart failure. Failure of these adaptive changes to maintain the cardiac output at the same optimal level with disease progression is known as the decompensated heart failure. In compensated heart failure, the patient remains either asymptomatic or minimally symptomatic whereas in decompensated heart failure the patient becomes severely symptomatic. This is the main difference between compensated and decompensated heart failure.
Reference:
1.Kumar, Parveen J., and Michael L. Clark. Kumar & Clark clinical medicine. Edinburgh: W.B. Saunders, 2009.
Image Courtesy:
1. Heart diagram-en By ZooFari Own work via Commons Wikimedia2. 1846050 via Pexels
Should You Avoid Taking Beta Blockers With Decompensated Heart Failure
While beta blockers have been a mainstay of therapy for many kinds of heart failure, they are not used during an episode of DHF. However, once a patient has been treated and stabilized, and shows no more signs of fluid retention, beta blockers are often recommended. Your healthcare provider will decide if beta blockers are right for you based on your health history.
Don’t Miss: Why Do Athletes Have Lower Heart Rate
Factors Associated With 2
Table 2 Comparison of survivors and non-survivors using age-adjusted Cox proportional hazards regression models
Age, sex, creatinine clearance, anaemia, systolic blood pressure, myocardial infarction, weight loss, body mass index, MNA-SF score, ADL score, Timed Get-Up-and-Go score, and MMSE score were available for the multivariable Cox model. Mobility impairment, lower body mass index, and MNA-SF category were not introduced into multivariable models, as they correlated with functional impairment and recent weight loss, respectively . Because of their association with other parameters, anaemia, myocardial infarction, and cognitive impairment were not independently associated with death in the multivariable model . No significant interactions were found between variables associated with 2-year mortality. By multivariable analysis , five factors were independently associated with 2-year mortality, namely, male sex, age older than 85 years, higher number of impaired ADL items, recent weight loss, and lower systolic blood pressure. A trend was noted for renal failure. The final model had good calibration and acceptable discrimination . The HRs estimated after bootstrap resampling were close to those of the original model, suggesting excellent internal validity. All five factors were also independently associated with 1-year mortality .
Table 3 Factors independently associated with 2-year mortality by multivariable analysis
Acute Decompensated Heart Failure
| Heart failure |
|---|
| Acute interstitial pulmonary edema. Note enlarged heart size, apical vascular redistribution , and small bilateral pleural effusions . |
| Cardiology |
Acute decompensated heart failure is a sudden worsening of the signs and symptoms of heart failure, which typically includes difficulty breathing , leg or feet swelling, and fatigue. ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart. An attack of can be caused by underlying medical illness, such as myocardial infarction, an abnormal heart rhythm, infection, or thyroid disease.
Treatment consists of reducing the fluid level with diuretics and improving heart function with nitrates, or levosimendan other treatments such as aquapheresis ultra-filtration may also be required.
Read Also: Abnormally High Heart Rate
Esc Clinical Practice Guidelines
The aim of this ESC guideline is to help health professionals manage people with heart failure according to the best available evidence. Fortunately, we now have a wealth of clinical trials to help us select the best management to improve the outcomes for people with HF for many, it is now both preventable and treatable. This guideline provides practical, evidence-based recommendations. The format of the previous 2016 ESC HF Guidelines was revised to make each phenotype of HF stand-alone in terms of its diagnosis and management. The therapy recommendations mention the treatment effect supported by the class and level of evidence and are presented in tables. In this guideline, we have decided to focus on the diagnosis and treatment of HF, not on its prevention.
Guidelines and related materials are for use by individuals for personal or educational purposes. No commercial use is allowed. Re-use permission must be correctly obtained .
Types Of Heart Failure
The chambers where your blood is pumped out of the heart are called ventricles. These may stiffen so that they no longer fill properly. Or, if your heart muscle becomes weak, the ventricles can fail to pump hard enough.
Heart failure can begin on either the left or right side of your heart. Sometimes, both sides may fail at the same time. The different types of heart failure correspond to where the heart is failing:
Don’t Miss: Congestive Heart Failure Sudden Death
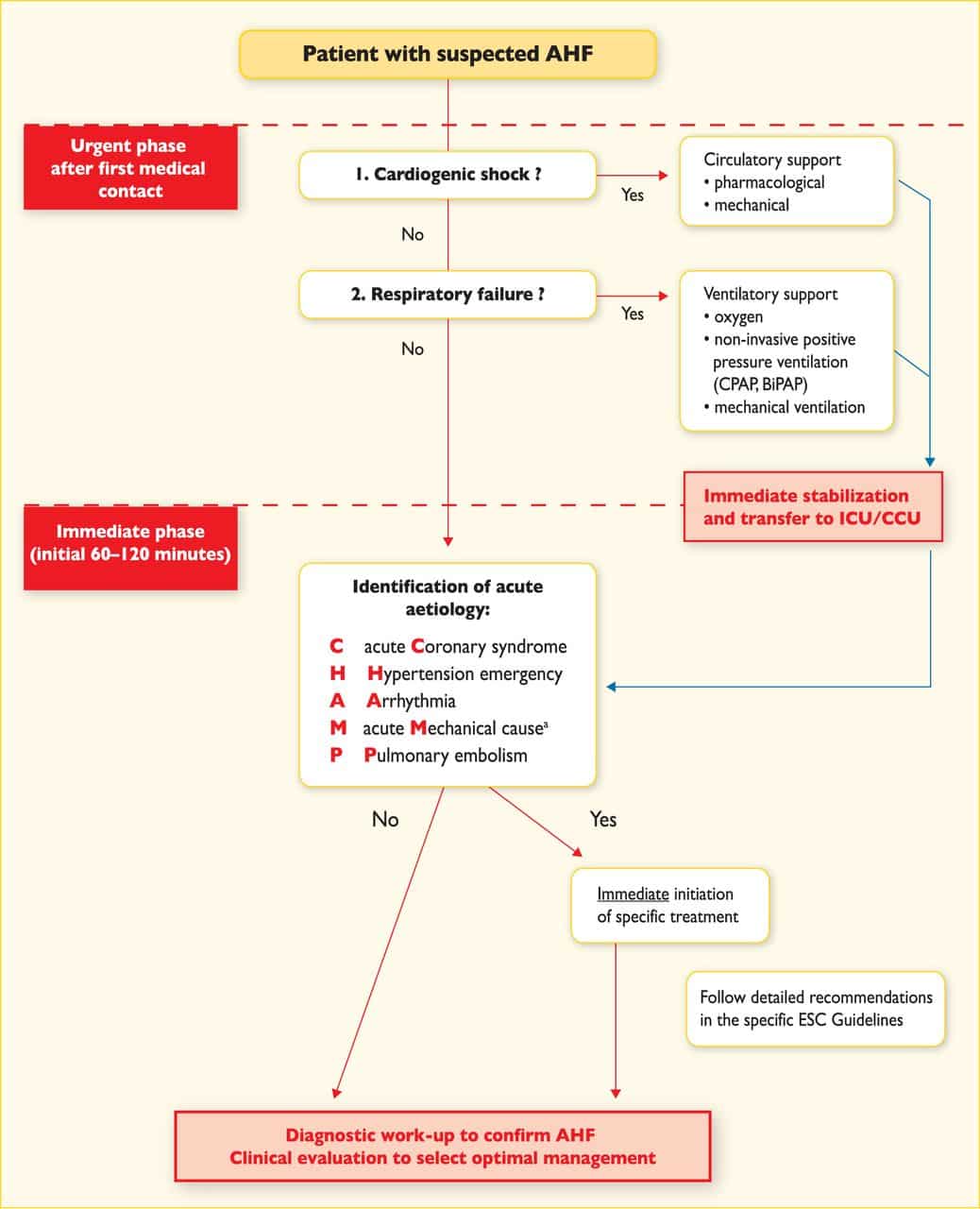
Classification Of Acute Heart Failure
The definition of AHF presented here is broad and there have been many attempts to stratify this further . Although characterised by a distinctive set of signs and symptoms, a major challenge in classifying AHF as a single entity is that the patient population is not uniform. Patients admitted with HF exhibit a wide spectrum of disease and range from those with severe LV systolic dysfunction and low cardiac output to those with severe hypertension and normal or near-normal LV systolic function. The majority of patients with AHF lie between these extremes and therefore also demonstrate a distribution of underlying pathology and precipitants, leading to the common endpoint of fluid overload.
This is a neat classification system and focusses the treating physician towards the management of the underlying cause of AHF. However, given patients often present with a range of co-morbidities, the reasons for decompensation may not be apparent at initial presentation or indeed, there may be multiple contributing factors. Practically speaking, therefore, it may be more prudent to stratify patients with AHF based on their initial clinical presentation. This allows the attending physician to identify those most at risk in order to direct specific interventions such as instituting ionotropic agents and/or mechanical circulatory support.
Pathophysiological Mechanisms Of Ahf
An underlying structural or functional cardiac condition is a prerequisite for AHF and includes a multitude of different acute or chronic cardiac pathologies. The underlying cardiac disease leads to the activation of several pathophysiological pathways that counter the negative effects of HF on oxygen delivery to the peripheral tissues, but such pathways can also eventually cause systemic congestion, ventricular remodelling and organ dysfunction. Furthermore, some acute diseases can act as precipitating factors and trigger AHF either by directly impairing cardiac diastolic and/or systolic function or by further promoting systemic congestion. Systemic congestion has a major effect on the clinical presentation in the majority of patients with AHF and is a relevant determinant of multi-organ dysfunction occurring in AHF . The pathophysiology of AHF is heterogeneous, as it is greatly affected by the nature of the underlying cardiac disease. It is perhaps not surprising, therefore, that the responses to treatment may vary and that different patients may respond best to distinct treatment strategies that depend on the underlying pathophysiology.
Fig. 1: Schematic representation of possible pathophysiological mechanisms in AHF.
LV systolic and diastolic dysfunction
Fluid retention
Aug 29, 2021 | Supriya Shore, MD
The following are key points to remember from the 2021 European Society of Cardiology Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure :
Don’t Miss: Recipes For Congestive Heart Failure And Diabetes
How Is Acute Heart Failure Diagnosed
Healthcare providers perform a rapid assessment that includes:
- Your health history, including your personal or family history of heart disease. Theyll want to know about other health conditions like whether you use tobacco products and any medications you take.
- A physical exam to learn more about your symptoms and how severe they are. This includes listening to your heart and checking for signs of edema.
Will I Need Other Treatments
After you leave the hospital, you may need medications, like beta blockers or water pills, to maximize heart health. Other treatments may be necessary to prevent future episodes of acute heart failure.
These treatments may include surgery to:
- Stent placement or coronary bypass surgery for coronary artery disease.
- Repair or replace worn-out heart valves .
- Implant a pacemaker or implantable cardioverter defibrillator to help you maintain a regular heartbeat and help treat dangerous heart rhythms.
- Replace your heart with a healthy one from a donor .
- Give your heart extra help with a ventricular assist device until you can have a transplant.
Read Also: Does Arousal Increase Heart Rate
Treatment Options For Acute Heart Failure In Advanced Development Stage
Despite a considerable effort, few clinical trials have demonstrated significant improvements in long-term outcomes for patients with ADHF. Mortality remains high and patients are likely to experience frequent hospital readmissions therefore, the development of new therapies is warranted. Below, we review the currently available data for several promising investigational agents in advanced stages of clinical development for the management of ADHF.
Chronic Decompensated Heart Failure
Doctors may prescribe diuretics to eliminate excess fluid buildup in people with chronic decompensated heart failure. Another common name for these drugs is water pills. They can also treat high blood pressure.
A person should inform a doctor of any other medications they are taking. Some medications, including thiazide diuretics or cyclosporine, can interact with heart medications such as digoxin .
Vasodilators are another class of medications that people with chronic decompensated heart failure may take. The explains that these widen the blood vessels and reduce blood pressure.
Don’t Miss: Can Blood Pressure Show Signs Of Heart Attack
Acute Decompensated Heart Failure National Registry Algorithm
Inpatients with acute decompensated heart failure.
- The ADHERE Algorithm estimates in-hospital mortality in admitted patients with acute decompensated HF.
- This model uses 3 variables to classify patients, but it does not allow more precise characterization of individual risk.
- The ADHERE Algorithm can NOT predict intermediate- and long-term mortality risks.
- The analysis of the ADHERE cohort also identified heart rate and age as significant independent predictors of risk according to the regression model, but these variables were omitted from the algorithm in order to simplify the model as a bedside tool.
- The data used reflect individual hospitalization episodes, not individual patients, and multiple hospitalizations of the same patient may be entered into the registry as separate records.
- Study results were based on a registry, the accuracy of which can be influenced by differences in disease assessment, treatment, and documentation patterns at participating institutions.
Risk stratification, triage and optimization of medical management.
Please fill out required fields.
Dr. Gregg Fonarow
A History Part I: Pattern Recognition:
The cardinal manifestations of ADHF are dyspnea, fluid retention, and fatigue. Fluid retention, commonly leads to pulmonary congestion and peripheral edema in patients with ADHF.
Patients may present with progressive weight gain, lower extremity edema, increasing dyspnea on exertion, or dyspnea at rest. Patients may report orthopnea and/or paroxysmal nocturnal dyspnea.
Patients may note abdominal bloating or a decrease in appetite. Some patients may present with fatigue or even altered mental status. Some patients may present with sudden onset of dyspnea.
Common factors that precipitate ADHF may include noncompliance with medical regimen, sodium and/or fluid restriction, acute coronary syndromes, uncorrected high blood pressure, atrial fibrillation and other arrhythmias, pulmonary embolus, use of NSAIDs, excessive alcohol or illicit drug use, endocrine abnormalities, exacerbation of pulmonary diseases, or concurrent infections such as pneumonia.
Common causes of ADHF
Lack of compliance with HF medications
New medication
Substance abuse
You May Like: What Does Heart Attack Feel Like
Acute Decompensated Heart Failure: History And Biologic Markers
However, although NT-proBNP performs well in an unselected population with dyspnea, the marker may have limited utility to distinguish increased pressure from increased permeability edema. In a prospective cohort study of patients with ARDS or ARDS risk factors, NT-proBNP was reported at a median value greater than 3000 pg/mL, well above the value to exclude heart failure only one-third of ARDS subjects had normal NT-proBNP values.129 Furthermore, although the NT-proBNP values observed in ARDS were numerically lower than those observed in the ADHF subjects from the PRIDE study, the difference between them was not statistically significant.127,129 A few smaller studies have assessed the ability of BNP to distinguish ARDS from cardiogenic pulmonary edema, using clinician judgment as the gold standard to determine edema type, and reported limited discriminative utility.130132
Nicholas Ioannou, … David Treacher, in, 2014
What Is The Prognosis For People With Heart Failure
The prognosis for heart failure varies widely and depends on the underlying cause and whether it can be treated.
Your outlook depends on a variety of factors, including:
- Heart failure cause and severity.
- How quickly you receive care.
- Your overall health and response to treatment.
- Commitment to heart-healthy living.
You May Like: Does Aspirin Increase Heart Rate
Diagnosis Of Acute Heart Failure
The diagnosis of acute heart failure in critically ill patients can be more difficult than is commonly recognised. Although the underlying pathology in most patients with acute heart failure on intensive care will be coronary artery disease, other diagnoses must be considered .
It is also important to reassess critically the patient referred with a diagnosis of acute heart failure to decide whether this is indeed the primary problem. The history, examination and initial investigations with routine blood tests, electrocardiogram and chest X-ray may be compatible with this diagnosis but many such patients are elderly with multiple co-morbidities, and deciding whether the patient is suffering from a primary myocardial pathology as opposed to a pulmonary problem or indeed systemic sepsis6 can be difficult. Equally, patients believed to have a primary respiratory problem may fail to wean from ventilatory support because of a failure to realise that they have left ventricular failure with a high left atrial pressure and incipient pulmonary oedema, causing a reduction in pulmonary compliance, an increased work of breathing and respiratory distress when ventilatory support is withdrawn.
Further investigations that can help to confirm or refute an initial diagnosis of acute heart failure are echocardiography and the measurement of biomarkers such as natriuretic peptides and cardiac troponins.
Peter S. Pang, Marco Metra, in, 2020
D Physical Examination Findings

The physical exam should focus on several key features including vital signs, the cardiopulmonary examination, neck veins, and extremities. Patients may be tachycardic and have blood pressure derangements.
Hypertensive patients are more likely to have preserved systolic function, whereas hypotensive patients are more likely to be in a low-cardiac output state carrying a worse prognosis. Pulmonary examination often reveals crackles, consistent with interstitial pulmonary edema, or wheezing.
Examination of the neck veins provides diagnostic and prognostic information. Elevation of jugular venous pressure is indicative of elevated right-sided filling pressures, which in patients with advanced heart failure, predicts elevated left-sided filling pressures in 80% of cases.
Cardiac auscultation may reveal either a third and/or a fourth heart sound suggestive of cavitary dilation or decreased compliance of the left ventricle respectively. A new or changed murmur usually represents valvular abnormalities, which may reflect altered ventricular geometry.
Abdominal examination may reveal hepatomegaly as a result of passive congestion, hepatojugular reflux or ascites. Extremity examination may reveal peripheral edema, particularly in the dependent portions of the body. Perfusion may be assessed by capillary refill time and physicians perception of skin temperature .
Donât Miss: Why Does My Resting Heart Rate Fluctuate
Recommended Reading: What Is The Closest Thing To A Magic Bullet Against Heart Disease
Congestion And Organ Dysfunction
In the heart, elevated ventricular filling pressures lead to increased ventricular wall tension, myocardial stretch and remodelling, contributing to a progressive worsening in cardiac contractility, valvular regurgitation and systemic congestion. In response to the increased wall tension, circulating natriuretic peptides are physiologically released by atrial and ventricular cardiomyocytes as a compensatory mechanism, and often high-sensitivity cardiac troponins are detectable in a large proportion of patients with AHF, revealing nonischaemic myocyte injury or necrosis. Increases in left atrial pressure and mitral valve regurgitation will increase the hydrostatic pressure in the pulmonary capillaries, thereby increasing fluid filtration rate from the capillaries to the pulmonary interstitium, causing lung stiffness and dyspnoea. Notably, the relationship between hydrostatic pressure and interstitial fluid content is rather complex, as other mechanisms are involved in fluid homeostasis. For example, the lymphangiogenic factor VEGF-D has been found to regulate and mitigate pulmonary and systemic congestion in patients with HF or renal failure,,. Indeed, in the early stage of lung congestion, the lymphatic system can cope with the large volume of interstitial fluid, but eventually, the drainage capacity is exceeded. Hence, fluid moves to pleural and intra-alveolar spaces causing pleural effusion and pulmonary oedema.
You May Like: Scars From Heart Surgery
