How Afib Leads To Heart Failure
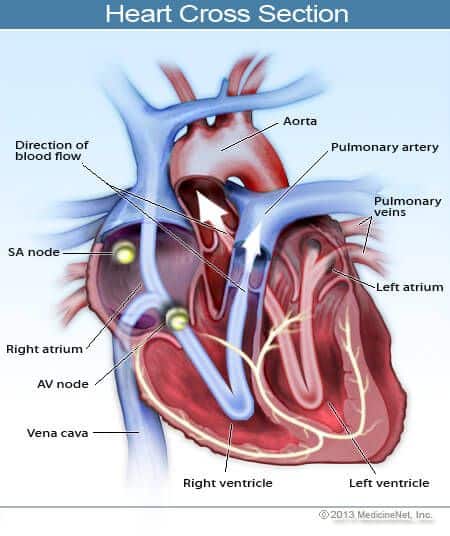
When you have AFib, your heart may beat faster than normal, even when you’re just resting. And since the heart’s doing more of a quiver than a strong push, it ends up sending out only some of the blood it normally would. It’s like the difference between a bunch of short, frantic bursts on a bike pump versus long, steady strokes.
AFib can also cause fluid buildup in your lungs. Your lungs fill your blood with oxygen before sending it back to your heart. So now, your heart doesn’t get enough oxygen-rich blood from the lungs, and even if it does, it’s beating too fast to do a good job of pumping it out.
And a rapid heartbeat — or just one that’s never regular — can damage the muscles of your heart.
All of that sets the stage for heart failure. Even though your heart’s working really hard — too hard — your body’s still not getting the oxygen it needs.
Afib And Congestive Heart Failure
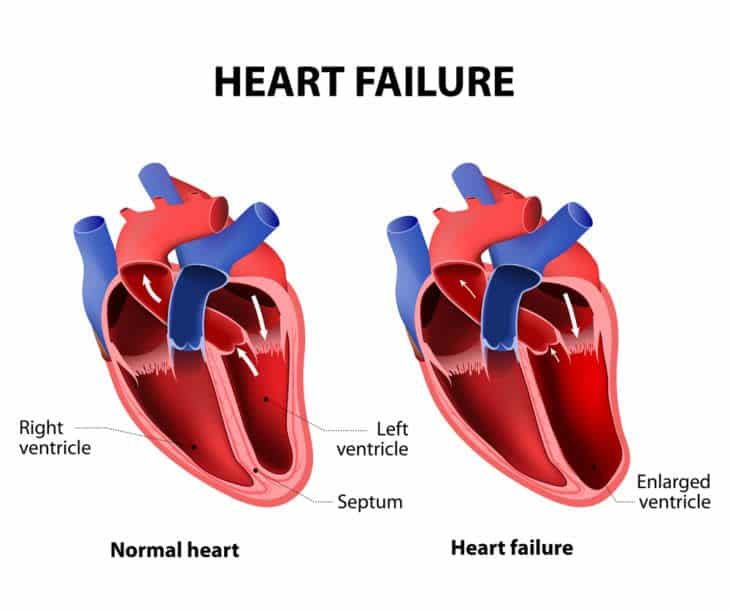
Considering overall heart health, there are often other heart issues that go along with atrial fibrillation. A common condition those living with AFib often face is congestive heart failure, commonly known as CHF. CHF often refers to a weak heart but can also signify a stiff heart, meaning it doesnt pump blood efficiently throughout the body.
This can lead to back-flow, causing fluid buildup in the lungs or swelling of the legs, which are the most common symptoms of congestive heart failure.
Focus Issue: Heart Failure Etiology And Outcomesstate
Optimal treatment strategies for patients with HF and AF are unclear.
-
Current rate and rhythm control pharmacotherapies present challenges however, randomized trials of catheter ablation have been promising.
-
Future research should focus on improving long-term outcomes in HF with AF and the effective primary prevention of HF in patients with AF.
Don’t Miss: What Mimics A Heart Attack
Specific Implications In Chf
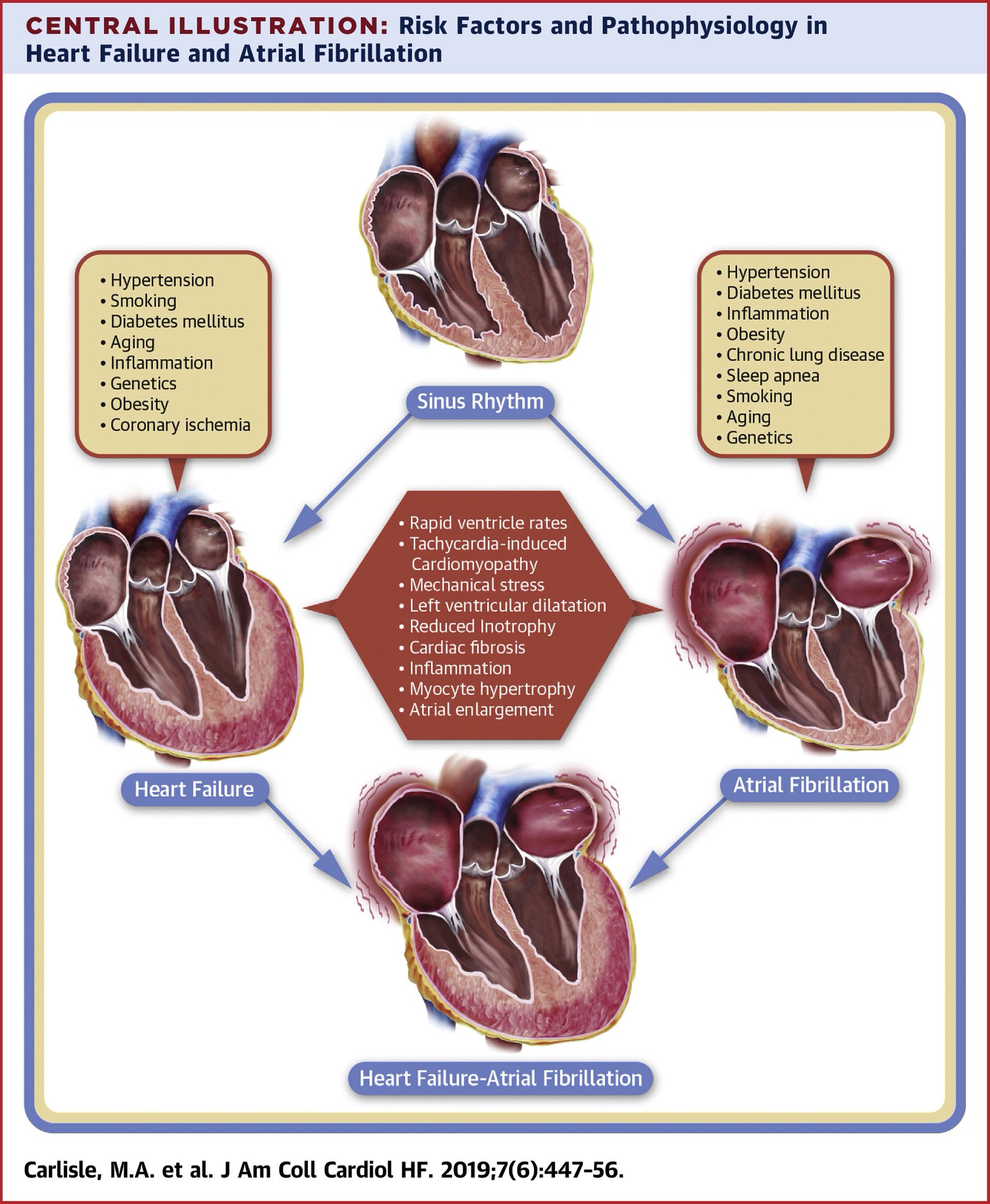
Thus it is clear that electrical triggers, susceptible substrate, and modulating factors are important for the promotion of AF. Genetic factors may promote AF by increasing susceptibility to reentry, triggered activity, disrupting cell-to-cell communication, and through other currently as yet undefined mechanisms. Several of the discussed pathophysiological mechanisms are of particular importance in patients with CHF .
Elevations in left atrial and pulmonary venous pressure present in CHF promote AF as well. Myocyte stretch increases firing from ectopic foci such as the pulmonary veins through mechanoelectrical feedback . Additionally, increased fibrosis results from myocyte stretch. Gross evidence of structural remodeling includes left atrial enlargement, which predisposes to AF . Although increased atrial refractoriness has been observed clinically in patients with CHF, shortening of the atrial refractory period has been reported in experimental models of left atrial stretch, suggesting that many competing processes may be occurring simultaneously in these patients .
Can Taking Too Many Medications Impact Older Adults With Heart Failure
Yes. As we age, the body doesnt handle the medicine in the same way. It metabolizes medicines differently, which is why taking too many medications can be a problem for older patients with heart failure. As we age, the liver and kidneys dont work as well, so drugs can sometimes build up in the system. Older people on medicines for their heart might be on five, six or 10 other drugs. So theyre taking a whole cocktail of medicines that might not work well together and could have side effects. Its helpful to re-prioritize medications with your doctor. Over-the-counter pain medications can sometimes be very dangerous in older people because they can raise blood pressure and harm the kidneys. They can also have a sedative effect on people and cause delirium.
Read Also: How To Help Heart Palpitations
Prognosis Of Patients With Atrial Fibrillation And Heart Failure
Despite the knowledge of the association between atrial fibrillation and heart failure, the data regarding the joint prognosis of these two conditions are conflicting.14 A retrospective study of 390 patients with advanced heart failure found that patients with atrial fibrillation had significantly higher mortality rates than those in sinus rhythm, despite similarities in heart failure etiologies, pulmonary capillary wedge pressures, left ventricular ejection fractions, and the presence of
What You Need To Know About Heart Failure Treatment For The Elderly
Heart failure is a cardiac condition where the heart does not pump blood as efficiently as it should, resulting in a lack of oxygen and nutrients throughout the body. Though it affects people of all ages, heart failure is the leading cause of hospitalizations in people older than 65. Elderly patients who experience heart failure are likely to already have a chronic cardiovascular condition, but it can also be caused by physical decline due to aging and poor cardiovascular management throughout life. Other risk factors include obesity, a family history of heart failure, hypertension and diabetes.
Early signs of heart failure in the elderly are similar to those found in other age groups, which include worsening or shortness of breath, fatigue, bloating, lack of appetite, persistent cough, lack of appetite and nausea. Other symptoms may include a mental decline or depression.
You May Like: Can Heart Failure Get Better
Read Also: Do Heart Palpitations Make You Cough
What Causes Atrial Fibrillation
Sometimes the cause of AFib is unknown. Other times, it is the result of damage to the hearts electrical system from other conditions, such as longstanding, uncontrolled high blood pressure or coronary artery disease. AFib is also the most common complication after heart surgery.
Learn about the important connection between atrial fibrillation, high blood pressure and stroke.
Left Ventricular Systolic Function
-
In patients carefully screened to exclude coronary artery disease and hypertension, there is little change in left ventricular systolic function with increasing age, although cardiac output may decrease in parallel with a reduction in lean body mass.w7 The determinants of cardiac output which may be influenced by age include heart rate, preload and afterload, muscle performance, and neurohormonal regulation.
-
Increases in heart rate in response to exercise or stress caused by non-cardiovascular illnesses, particularly infections, are attenuated with increasing age.w8 Stroke volume increases only by moving up the Frank Starling curve.w9w10 Thus end diastolic volume increases. These age related changes in cardiac response to exercise are mimicked by adrenergic blockade,w11 but adrenergic agonists do not reverse this aging process.w12 The decline in exercise performance with age may additionally relate to peripheral factors, blood flow, and muscle mass rather than being solely the consequence of cardiac performance changes.
Recommended Reading: What Is Your Max Heart Rate
Recommended Reading: What Is A Normal Heart Rate
Atrial Fibrillation And Congestive Heart Failure Trial
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : January 17, 2008Last Update Posted : February 8, 2008 |
| Phase | ||
|---|---|---|
| Atrial FibrillationCongestive Heart Failure | Other: Rate vs rhythm control strategies for atrial fibrillationOther: Rate vs rhythm control strategies in atrial fibrillation | Phase 4 |
Congestive heart failure and atrial fibrillation are two important and growing problems in medicine and cardiology. Both conditions often co-exist and complicate each others management. Two therapeutic strategies are available for patients with AF and CHF: the first aims at restoring and maintaining sinus rhythm, whereas, the second focuses exclusively on optimizing ventricular rate. The primary objective of the Atrial Fibrillation and Congestive Heart Failure trial is to compare these two widely-used treatment strategies with respect to cardiovascular mortality.
Hypothesis: Restoring and maintaining sinus rhythm reduces cardiovascular mortality compared to a rate control treatment strategy in patients with AF and CHF.
Prognosis Of Comorbid Af And Chf
Whereas substantial morbidity and mortality is attributable to each of these individual conditions, the concomitant presence of AF and CHF identifies individuals with a higher risk for death than with either condition alone. The prognostic impact of incident AF or CHF among individuals diagnosed with the other comorbid condition was assessed by investigators from the Framingham Heart Study . The development of AF in individuals with CHF was associated with a hazard ratio for death of 1.6 in men, and 2.7 in women, during follow-up of 4.2 years. Similarly, the development of CHF among individuals with AF was associated with a hazard ratio for death of 2.7 in men, and 3.1 in women, over a follow-up of 5.6 years.
Thus, AF and CHF commonly coexist, share a similar risk factor profile, and have adverse hemodynamic effects. The simultaneous presence of both diseases identifies individuals at substantially increased risk of cardiovascular events and death.
Recommended Reading: How Do I Know If I M Having Heart Attack
Atrioventricular Nodal Ablation And Pacemaker Placement
While the ablate and pace approach achieves rate control, it does not restore sinus rhythm and necessitates permanent implantation of a mechanical pacemaker. AV nodal ablation with biventricular pacing was compared to AF ablation in a pilot study of 35 subjects with CHF and systolic left ventricular dysfunction . In the Pulmonary Vein Isolation Versus AV Nodal Ablation With Biventricular Pacing for Patients With Atrial Fibrillation With Congestive Heart Failure study, pulmonary vein isolation was associated with greater improvement in symptoms and ejection fraction as compared with the ablate and biventricular pacing group.
Definitive trials assessing the effectiveness of AF ablation as compared with an ablate and ventricular pacing strategy are warranted. In the meantime, atrioventricular node ablation and ventricular pacing remains a reasonable option for the management of patients in whom the achievement of adequate rate control with pharmacologic therapy is inadequate .
Temporal Relation Of Af And Chf
In a large cohort of patients from the Framingham Heart Study, at first diagnosis of AF, 26% of patients had a prior or concurrent diagnosis of CHF, and 16% of the remaining patients developed the condition during the follow up period of 5.6 years . Among patients who developed CHF, 24% had a prior or concurrent diagnosis of AF, and 17% developed AF during the follow up period of 4.2 years . Patients with a previous diagnosis of AF were found to develop CHF at a rate of 3.3% per year, and the ones with previous CHF developed subsequent AF at a rate of 5.4% year. The coexistent presence of AF and CHF worsens both symptoms and mortality than either disorder alone in most large studies., There are conflicting data as to whether AF is an independent predictor of mortality in patients with CHF, with the largest experience coming through subset analyses of the SOLVD , CHARM and V-HeFT trials.,,
Also Check: How Long Can A Heart Attack Last Before Death
Clinical Presentation Of Af In Hf
Key elements in diagnosing HF are signs and symptoms of HF and reduced LVEF. It, however, is often difficult to diagnose HFpEF in patients with AF. This is due to a large overlap in signs and symptoms. For example, breathlessness and fatigue are important symptoms in HF but may also be found in AF without diagnosed or recognised HF. A recent white paper suggested some signs and investigations to use in clinical practice.
Prevalence Of Comorbid Af And Chf
As both AF and CHF occur frequently, the simultaneous presence of these two conditions is common. The prevalence of AF in patients with systolic left ventricular dysfunction and CHF ranges from 6% for asymptomatic patients or for those with minimal symptoms , to between 15% and 35% for patients with New York Heart Association class IIIV symptoms . In two large epidemiologic studies , the prevalence of AF was greater in CHF patients with preserved ejection fractions than in those with left ventricular systolic dysfunction, though the rates of AF were similar in patients with systolic as compared to diastolic CHF in one clinical trial .
The concomitant presence of both AF and CHF in many patients may be explained by shared underlying risk factors and mechanisms, or a causal relation between the entities. Indeed, many risk factors for AF have been recognized as leading risk factors for CHF . The shared risk factors include hypertension, diabetes mellitus, ischemic heart disease, and valvular heart disease . Additionally, evidence of myocarditis, one potential cause of dilated cardiomyopathy and CHF, has also been implicated in the genesis of AF . In one series, AF was directly attributable to CHF in 5% of cases .
You May Like: Sign Of Heart Failure
Temporal Relations Of Af And Chf
The temporal relations of AF and CHF were examined in a study of 1470 patients with new onset AF or CHF from the Framingham Heart Study . The average follow-up was 5.6 years after the development of AF, and 4.2 years after the development of CHF. Among patients who developed AF, 26% had a prior or concurrent diagnosis of CHF, and 16% of the remaining patients subsequently developed CHF during the follow-up period. Among patients who developed CHF, 24% had a prior or concurrent diagnosis of AF, and 17% developed AF during the subsequent follow-up period. For patients diagnosed with AF, the incidence of developing CHF was 33 per 1000 person-years. Conversely, among individuals diagnosed with CHF, the incidence of developing AF was 54 per 1000 person-years.
The association between AF and the development of CHF was also analyzed in a study of 3288 patients diagnosed with AF at the Mayo Clinic . Twenty-four percent developed CHF during a mean follow-up of 6.1 years, with an incidence of 44 per 1000 patient-years. A spike in the incidence of CHF was seen early after the diagnosis of AF, with 7.8% of cases occurring within the first 12 months, and approximately 3% per year thereafter. Patients with lone AF fared well, as only about 2% developed CHF within 5 years of being diagnosed with AF .
What You Can Do
Some risk factors of heart failure, like age, cant be modified. Still, people with CHF can take steps to improve the long-term prognosis. The first thing to do is to be familiar with any family history of heart disease. You’ll also want to learn about all the possible symptoms. Don’t ignore any symptom that you think is cause for concern. Tell your healthcare provider about them right away.
Regular exercise, along with managing any other health issues you may have, can also help to keep CHF under control.
Don’t Miss: Exercise After Heart Surgery
Causes Of Heart Failure
Heart failure is often the result of a number of problems affecting the heart at the same time.
Conditions that can lead to heart failure include:
- coronary heart disease where the arteries that supply blood to the heart become clogged up with fatty substances , which may cause angina or a heart attack
- high blood pressure this can put extra strain on the heart, which over time can lead to heart failure
- conditions affecting the heart muscle
- heart rhythm problems , such as atrial fibrillation
- damage or other problems with the heart valves
- congenital heart disease birth defects that affect the normal workings of the heart
Sometimes obesity, anaemia, drinking too much alcohol, an overactive thyroid or high pressure in the lungs can also lead to heart failure.
Will Atrial Fibrillation Make My Life Harder
You might find it harder when getting used to a new routine. AF is a manageable condition and with the right treatment you can carry on as you were before you were diagnosed.
Talking to people about your condition can be hard. Dealing with stress and anxiety is also common after being told you have a heart condition. Visit our emotional support hub for advice and support if youre struggling with the change of pace.
You might have to think about practical matters, like driving, going on holiday or travel insurance after being diagnosed with AF. Again, your GP can help with any queries you might have.
Recommended Reading: Do Heart Attack Symptoms Come And Go Over Weeks
Pathophysiology Of Af In Chf
The pathophysiologic basis of AF is complex and incompletely understood . Initial mechanistic explanations for AF cited reentry as a principal factor . The multiple wavelet hypothesis, proposed by Moe and Abildskov, stated that the development of AF depended on the perpetuation of a sufficient number of randomly wandering wavelets created as a normal occurrence due to heterogeneous repolarization. The hypothesis maintained that adequate atrial mass, short refractory periods, and conduction velocities slow enough to permit temporal disparities in depolarization and repolarization in the atria favored the development of these reentrant wavelets.
This argument is predicated on the concept that the wavelength of an electrical signal also represents the minimal pathway length that must be present to sustain a reentrant circuit. If a pathway is shorter, then a reentrant electrical stimulus will encounter refractory tissue upon completing the circuit and terminate. In contrast, if the pathway is longer then the electrical signal may encounter excitable tissue upon completing the circuit, thereby perpetuating the previous cycle. The wavelength, and thus the pathway length, is proportional to both the refractory period of the tissue, as well as the conduction velocity. This model explains precipitants of AF that shorten the atrial effective refractory period or decrease conduction velocity.
Mechanisms promoting atrial fibrillation in congestive heart failure.
Current Therapeutic Options For Heart Failure In Elderly Patients
F. Guerra
1Cardiology and Arrhythmology Clinic, Department of Biomedical Sciences and Public Health, University Hospital Ospedali Riuniti, Marche Polytechnic University, Ancona, Italy
Academic Editor:
Abstract
Heart failure is a major and growing public health problem with high morbidity and mortality . It affects 1-2% of the general population in developed countries, and the average age at diagnosis is 76 years. Because of a better management of acute phase and comorbidities, HF incidence is increasing in elderly patients, with a prevalence rising to 10% among people aged 65 years or older . Therefore, a substantial number of elderly patients need to be treated. However, because of clinical trial exclusion criteria or coexisting comorbidities, currently recommended therapies are widely based on younger population with a much lower mean age. In this review, we will focus on available pharmacological, electrical, and mechanical therapies, underlining pros, cons, and practical considerations of their use in this specific patient population.
1. Drug Therapy
To date, limited evidence has investigated the effects of the recommended systolic HF therapies in aged patients . However, data from small observational studies and substudies suggest that elderly patients derive similar benefits as younger patients .
2. Anemia and Iron Deficiency
3. Implantable Cardioverter-Defibrillator
5. Left Ventricular Assist Device
7. Conclusions
Read Also: Resting Heart Rate Age Chart
