Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Nutritional deficiencies
Surgery And Percutaneous Procedures
Surgery may be appropriate when certain underlying disorders are present. Surgery in patients with advanced HF should be done in a specialized center.
Surgical closure of congenital or acquired intracardiac shunts can be curative.
If HF is primarily due to a valvular disorder Overview of Cardiac Valvular Disorders Any heart valve can become stenotic or insufficient , causing hemodynamic changes long before symptoms. Most often, valvular stenosis or insufficiency… read more , valve repair or replacement should be considered. Patients with primary mitral regurgitation are more likely to benefit than patients with mitral regurgitation secondary to LV dilation, in whom poor myocardial function is likely to continue postoperatively. Surgery is preferably done before myocardial dilation and damage become irreversible. More recently, percutaneous mitral valve repair procedure, in which a clip is applied to approximate the anterior and posterior mitral leaflets, has been shown to reduce death and HF hospitalization in carefully selected patients with symptomatic HF despite optimal medical management and moderate to severe or severe mitral regurgitation with preserved LV size is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal fluid… read more ).
Stage C Treatment Options
Treatment at this stage focuses on managing your symptoms, optimizing your heart function, and preventing worsening of your condition.
Medications to treat stage C heart failure include:
- Diuretics to reduce fluid retention
- Beta blockers to help make your heart work less hard
- SGLT2 inhibitors to reduce the risk of cardiovascular death and hospitalization for heart failure
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Entresto , which reduces the risk of death and hospitalization among patients with chronic heart failure
- Aldosterone antagonists
- Digoxin to help the heart beat stronger and more regularly
- Possible cardiac resynchronization therapy
- Possible implantable cardiac defibrillator therapy
In addition to the lifestyle changes for stages A and B, you may need to make the following changes:
- Reduce your sodium intake
- Restrict fluid intake
- Keep track of your weight daily
Remember that even if the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression of your condition to stage D.
You May Like: Why Is My Heart Palpitating
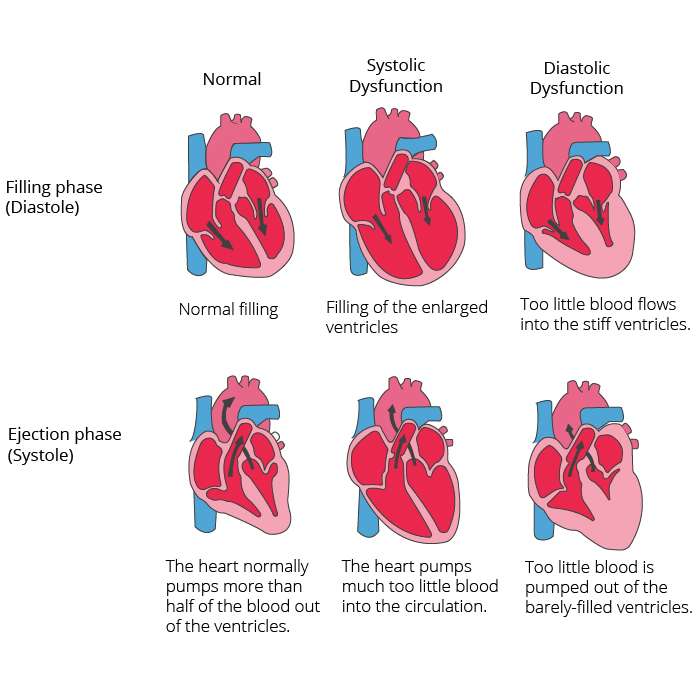
Heart Failure With Reduced Ejection Fraction
Systolic heart failure is also called heart failure with reduced ejection fraction .
Ejection fraction is the percentage of blood the left ventricle pumps out with every beat. A normal, healthy ejection fraction is 55% to 65%. If its higher or lower, that can indicate a heart problem.
With systolic heart failure, the ejection fraction is usually less than 50%.
Ps Matching And Covariate Balance
The distributions of baseline covariates between DHF and SHF patients before and after matching are displayed in Table 1 and Figure 1. After matching, standardized differences for all observed covariates were below 10% in absolute value, suggesting substantial improvement in covariate balance between DHF and SHF patients . Mean PS for unmatched and matched SHF and DHF patients and a graphical assessment indicate that patients excluded in the matching process were at the extremes of the PS distribution, as is usual.
Read Also: What Heart Rate Is Tachycardia
Etiology Congestive Heart Failure
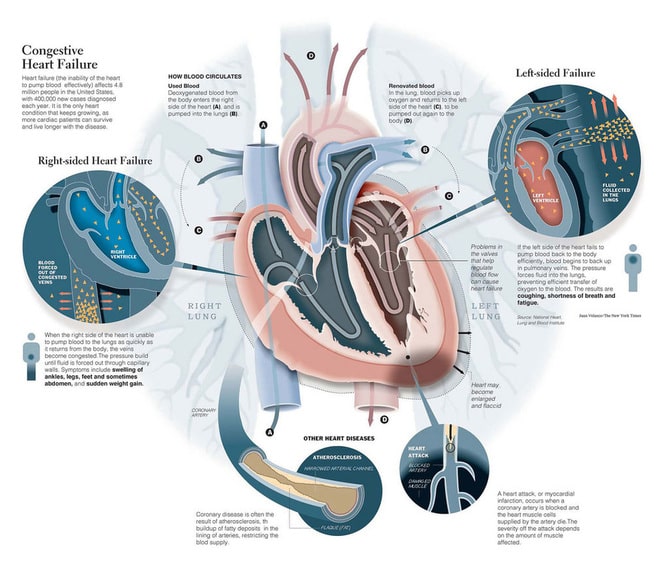
There are numerous causes for systolic heart failure, but the most common is related to coronary artery disease and prior myocardial infarctions. This entity is termed an ischemic cardiomyopathy and accounts for nearly half of systolic heart failure cases in the United States.
Dilated cardiomyopathy is the second leading cause of systolic HF. This can be idiopathic , a viral cardiomyopathy, peripartum and hypertensive heart disease . These include doxorubicin therapy, stress-induced , alcohol-related, selenium or thiamine deficiency, tachycardia-mediated, giant cell arteritis, hyperthyroidism, cocaine use, obstructive sleep apnea and familial cardiomyopathies.
The third leading cause of systolic HF is valvular heart disease. This includes aortic valve stenosis, aortic valve regurgitation, mitral valve stenosis and mitral regurgitation. In many developing nations, the most common cause of systolic HF is Chagas disease, which is related to Trypanosoma cruzi and transmitted by triatomine bugs.
Recall that right heart failure and diastolic heart failure are different entities from the left-sided systolic heart failure reviewed here. The most common cause of right HF is pressure overload related to left HF. Diastolic HF is most commonly caused by hypertension as a part of hypertensive heart disease. Aging of the heart contributes to diastolic HF as well.
Prognostic Significance Of Sleep Apnea In Heart Failure
Systolic heart failure is a complex disorder in which multiple pathophysiological processes are involved in and contribute to its progression. In the contemporary management of systolic heart failure, the identification and treatment of neurohormones and the use of angiotensin-converting enzyme inhibitors and -blockers have improved patients quality of life and survival. In spite of the many therapeutic triumphs, however, heart failure remains a major public health problem with considerable morbidity and mortality. Of utmost importance are the identification and treatment of residual comorbid factors that contribute to the progression of heart failure. One comorbid condition is sleep apnea results of studies, reviewed in the following discussion, strongly suggest that both OSA and CSA are associated with excess mortality in patients with heart failure and that effective treatment improves survival.
Multiple investigators have studied CSA and mortality most145-154 showed that CSA is associated with excess mortality among patients with systolic heart failure. Two studies156,157 yielded different results one156 revealed a tendency for excess mortality among patients with heart failure and CSA, but this finding was not significant, probably because of the small number of patients. In addition, patients with heart failure who exhibited periodic breathing while awake suffered excess mortality.
Chu-Pak Lau, … Hung-Fat Tse, in, 2017
Don’t Miss: Can Congestive Heart Failure Be Cured
Systolic Heart Failure Symptoms
The hallmark feature of systolic heart failure is shortness of breath, also called dyspnea.
A person with early systolic heart failure might get short of breath only when exercising. But a person with advanced systolic heart failure might have trouble breathing when simply walking across the room or even when resting.
Other signs of systolic heart failure are:
Medications For Systolic Heart Failure
Depending on the severity of systolic heart failure and its underlying cause, your doctor may prescribe medications. Some of the drug options for treating systolic heart failure include:
- Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers relax the blood vessels to lower blood pressure.
- Beta blockers make the heart beat more slowly and with less force.
- Aldosterone blockers help the body release sodium and water.
- Angiotensin receptorneprilysin inhibitors reduce excess fluid in the body and relax blood vessels, making it easier for your heart to pump blood.
Recommended Reading: Symptoms Of Heart Failure Getting Worse
Systolic Heart Failure Signs And Symptoms
Systolic heart failure symptoms may come on gradually or start suddenly. Systolic heart failure signs and symptoms of systolic heart failure may include:
- Shortness of breath during exertion or which causes you to wake up
- Sudden weight gain from fluid retention
- Swelling of the abdomen
- Swelling in your legs, ankles, and feet
Chronic Systolic Heart Failure
- 20162017201820192020202120222023Billable/Specific Code
- I50.22 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2023 edition of ICD-10-CM I50.22 became effective on October 1, 2022.
- This is the American ICD-10-CM version of I50.22 – other international versions of ICD-10 I50.22 may differ.
- Applicable To annotations, or
Also Check: What Does A Heart Attack Look Like On An Ecg
Stage A Treatment Options
Treatment options in stage A mainly focus on promoting your overall health and disease prevention. If you meet the stage A criteria, your doctor will recommend lifestyle changes to slow or stop disease progression.
Heart Failure Doctor Discussion Guide
Surgery For Systolic Heart Failure
In advanced cases of systolic heart failure, surgery may be a good treatment option. Your doctor will recommend surgery based on your exact symptoms and the cause of your condition. Surgical options include:
- Corrective surgery to fix an underlying problem, such as heart valve repair or replacement or coronary bypass surgery
- Pacemaker to regulate the heartbeat
- Implantable cardioverter defibrillator to monitor the heart for fast rhythm and deliver an electrical shock to reset the heart when necessary
- Left ventricular assist device , which takes over the pumping action of the heart
- Heart transplant to replace the heart with a donated heart from a person who has died
Don’t Miss: Heart Rate Jumps When Standing
Outlook For Heart Failure
Heart failure is a serious long-term condition that will usually continue to get slowly worse over time.
It can severely limit the activities you’re able to do and is often eventually fatal.
But it’s very difficult to tell how the condition will progress on an individual basis.
It’s very unpredictable. Lots of people remain stable for many years, while in some cases it may get worse quickly.
Diagnosis Congestive Heart Failure
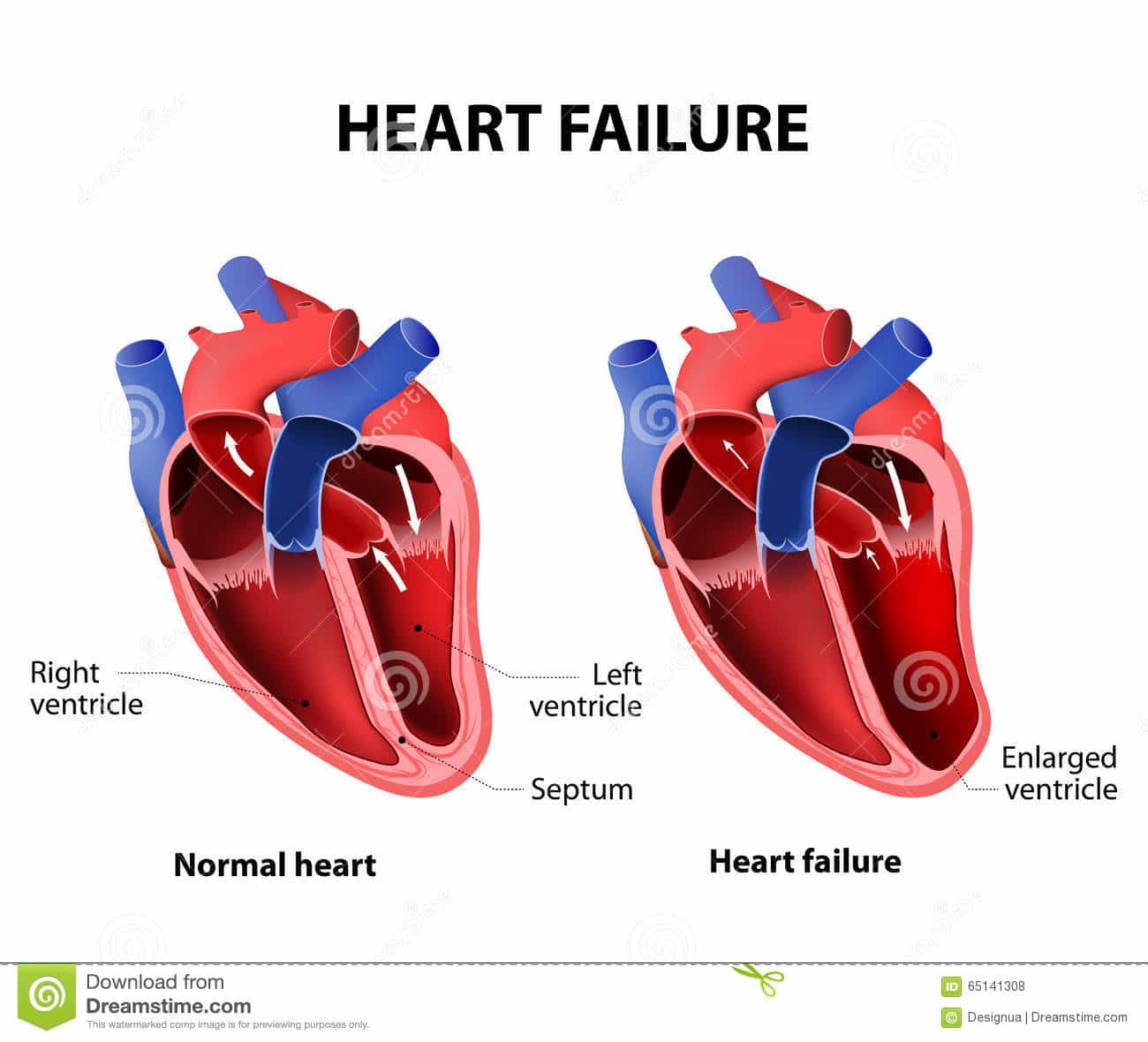
The diagnosis of congestive heart failure is predominantly by history and physical, though echocardiography and cardiac catheterization can be beneficial.
Physical examination during systolic congestive HF will reveal a S3 heart sound if significant left ventricular dilation is present. A S4 heart sound can be present in diastolic HF. The point of maximal impulse, or PMI, will be laterally displaced and, at times, the S3 can even be palpable. Cardiac murmurs will be present if valvular heart disease is present, contributing to the HF such as aortic stenosis or mitral regurgitation.
Physical examination in states of right heart failure may reveal elevated jugular venous pressure including hepatojugular reflux, lower extremity pitting edema and ascites. Pleural effusions may be present and more prominent on the right compared to the left.
Echocardiography is indicated in all patients with a new diagnosis of congestive HF to help determine the etiology. The LV systolic function can be measured, including ejection fraction. Diastolic function assessment can help determine the left heart pressures. The cardiac valves can be interrogated for significant regurgitant or stenotic lesions.
Also Check: Why Am I Getting Heart Palpitations
Chronic Treatment Of Hfref
The goals of HF therapy are clinical improvement followedby stabilizing, slowing, or even reversing deterioration in myocardial function, and ultimately a reduction in risk of morbidity and mortality.
-
Produce both venous and arterial vasodilation acutely, thereby reducing both preload and afterload.
- 3.
-
Potential mechanism of long-term benefit is attenuation of RAAS activation and decreased myocardial remodeling and fibrosis.
- 4.
-
Used as first-line therapy for asymptomatic LV dysfunction and symptomatic systolic HF .
- 5.
-
Therapy should be initiated at low doses to prevent hypotension and rapidly titrated to higher doses as tolerated.
- 6.
-
Contraindications to the use of ACE inhibitors are renal insufficiency , bilateral renal artery stenosis, hyperkalemia, hypotension, or adverse reactions .
-
Receptor antagonists to the angiotensin II receptor.
- 2.
-
Clinical trials have not shown any superiority compared to ACE inhibitors in patients with systolic HF .
- 3.
-
Reserved for patients who are ACE inhibitor intolerant.
- 4.
-
Combination therapy with ARBs and ACE inhibitors is generally not recommended.
- 5.
-
Have a similar contraindication profile to ACE inhibitors. Routine combined use of an ACE inhibitor, ARB, and aldosterone antagonist is potentially harmful for patients with HFrEF.
Tasneem Z. Naqvi, in, 2012
Anemia And Iron Deficiency
Anemia is common among patients with chronic heart failure and is frequently multifactorial. Anemia is associated with worse symptoms and outcomes in HF and so reversible causes should be sought and treated. Iron deficiency Iron Deficiency Anemia Iron deficiency is the most common cause of anemia and usually results from blood loss malabsorption, such as with celiac disease, is a much less common cause. Symptoms are usually nonspecific… read more is among the most common causes of anemia in HF, and iron replacement therapy should be considered once treatable causes such as blood loss have been excluded. Oral iron replacement is often less effective due to poor absorption and other reasons, thus intravenous iron replacement is preferred.
Don’t Miss: How Long Can You Have Heart Attack Symptoms
Acute Systolic Heart Failure Versus Chronic Systolic Heart Failure
Systolic heart failure can be classified as acute or chronic:
- Acute: You have active symptoms of heart failure with a new diagnosis or a long-term condition.
- Chronic: You have a history of heart failure, but are relatively stable.
Acute systolic heart failure is a medical emergency. Depending on the cause, some cases can be reversed with prompt treatment. Chronic systolic heart failure is a lifelong condition, and treatment aims to slow the disease and minimize symptoms.
What Causes Heart Failure
Heart failure is most often related to another condition. The most common cause of heart failure is coronary artery disease , a disorder that causes narrowing of the arteries that supply blood and oxygen to the heart. Other conditions that may increase your risk of developing heart failure include:
- cardiomyopathy, a disorder of the heart muscle that causes the heart to become weak
- congenital heart disease
Heart failure can occur in either the left or right side of your heart. Its also possible for both sides of your heart to fail at the same time.
Heart failure is also classified as either diastolic or systolic.
Read Also: How Long Is Open Heart Surgery Take
Treatment Of Patients With Left Ventricular Dysfunction And Current Or Prior Symptoms
Fig. 25G.1 andTable 25G.3 summarize the 2017 ACC/AHA/HFSA recommended approach to the treatment of stages C and D HFrEF.5 Application of the same measures recommended for preventing or minimizing progression of LV dysfunction for stage A and B patients is supported for stage C patients, who have current or prior symptoms attributable to LV dysfunction . Physical activity and cardiac rehabilitation are recommended for stage C patients. The updated guidelines also reflect the results of the recent HF-ACTION trial , in which exercise training did not have a favorable impact on all-cause mortality or HF hospitalization. Maximal exercise testing with or without measurement of respiratory gas exchange to facilitate an appropriate exercise program, which was a class IIa indication in 2009, is not recommended in the 2013 ACC/AHA guidelines, although it is still recommended in the 2016 ESC guidelines.
A.M. McDivit, … E.D. Adler, in, 2014
Pathophysiology Congestive Heart Failure
Congestive HF results in the activation of multiple compensatory mechanisms in an attempt to increase cardiac output. These frequently work in the short term however, the long-term effects can be detrimental to the heart via negative remodeling. The two primary mechanisms considered the neurohormonal response are activation of the sympathetic nervous system and activation of the renin-angiotensin-aldosterone system. Medical therapy is aimed at reducing the activity of these two systems. A third compensatory response occurs via B-type natriuretic peptide and A-type natriuretic peptide. See the summary image below.
When the carotid baroreceptors sense a low blood pressure, one response is to activate the SNS. This increases epinephrine and norepinephrine levels, which act to increase heart rate, contractility and afterload via peripheral vasoconstriction. In the short term, this will work to increase cardiac output and relieve HF symptoms however, chronically this has deleterious effects and causes further left ventricular systolic decline. Beta-blockers are the primary therapy to reduce this SNS activation.
Endothelin has negative effects in regards to remodeling and vasoconstriction however, clinical trials of endothelin inhibitors have never shown a benefit, and thus its role remains unclear.
Don’t Miss: Man Heart Attack Symptoms
Medications To Lessen Symptoms Of Systolic Heart Failure
Many of the symptoms of systolic heart failure are uncomfortable, and may limit the amount and type of activities you can participate in. Your doctor may recommend medications that treat the symptoms of systolic heart failure to make you more comfortable. Some of these options include:
- Diuretics reduce the amount of fluid in the body.
- Vasodilators dilate the blood vessels and reduce the hearts workload.
- Digoxin helps the heart beat stronger with a more regular rhythm.
- Anti-arrhythmics control arrhythmia and maintain normal heart rhythm.
Acute On Chronic Systolic Heart Failure
- 2016201720182019202020212022Billable/Specific Code
- I50.23 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM I50.23 became effective on October 1, 2021.
- This is the American ICD-10-CM version of I50.23 – other international versions of ICD-10 I50.23 may differ.
- Applicable To annotations, or
Don’t Miss: Silent Heart Attacks In Women
Diagnosis Of Heart Failure Of Acute Onset
|
Data from Ponikowski P, Voors AA, Anker SD, et al: 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology Developed with the special contribution of the Heart Failure Association of the ESC. European Heart Journal 37:2129-2200, 2016. doi: 10.1093/eurheartj/ehw128 |
