Anemia And Iron Deficiency
Anemia is common among patients with chronic heart failure and is frequently multifactorial. Anemia is associated with worse symptoms and outcomes in HF and so reversible causes should be sought and treated. Iron deficiency Iron Deficiency Anemia Iron deficiency is the most common cause of anemia and usually results from blood loss malabsorption, such as with celiac disease, is a much less common cause. Symptoms are usually nonspecific… read more is among the most common causes of anemia in HF, and iron replacement therapy should be considered once treatable causes such as blood loss have been excluded. Oral iron replacement is often less effective due to poor absorption and other reasons, thus intravenous iron replacement is preferred.
High Output Versus Low Output Heart Failure
- Low Output Failure: The cardiac output is reduced, and the systemic vascular resistance is high. In low output failure, there is an inadequate supply of blood flow to meet normal metabolic demands.
- High Output Failure: The cardiac output is increased, and the systemic vascular resistance is low. Rather than an inadequate supply of blood flow to meet normal metabolic demands as occurs in low output failure, in high output failure there is an excess requirement for oxygen and nutrients and the demand outstrips what the heart can provide. Causes of high output heart failure include severe anemia, Gram negative , beriberi , thyrotoxicosis, Paget’s disease, arteriovenous fistulae, or arteriovenous malformations.
Enhancing Healthcare Team Outcomes
Heart failure is a leading cause of hospitalization and represents a significant clinical and economic burden. The long-term goal of treatment is to avoid exacerbation of HF and decrease hospital readmission rates. It needs an interprofessional approach involving patients, physicians, nurses, pharmacists, families, and caretakers. Those strategies include early identification of high-risk patients, patient education, improving medication and dietary compliance, assuring close follow up, introducing end-of-care issues, and tele-home monitoring if available. Primary care and emergency department providers often are the first to make this diagnosis. Referal to cardiologists is often appropriate. Cardiology, medical/surgical, and critical care nurses administer treatment, provide education, monitor patients, and communicate with the rest of the team so that everyone on the healthcare team operates from the same data set. The managing clinician would do well to consult with a board-certified cardiology pharmacist when initiating pharmaceutical care in HF cases. Pharmacists also review medicines, check the dosages, detect drug-drug interactions, and stress to patients and their families the importance of compliance. In end-stage cases, hospice care and hospice nurses can work with the patient and their family to provide comfort care. These interprofessional collaborations will optimize patient outcomes in HF cases.
Don’t Miss: Heart Attacks In Teens
Acute And Chronic Heart Failure
People with acute heart failure have no previous signs and symptoms of heart failure. AHF can present with rapid swelling and fluid retention characterized by sudden weight gain. Coughing, wheezing, and shortness of breath, as well as an irregular heartbeat, could be symptoms of acute heart failure. In some cases, it is related to pre-existing cardiomyopathy.6-7 AHF often requires unexpected hospital admission. It can also be associated with a poor prognosis and a high risk of readmission and death post-discharge.8 Treatment options include medication, surgery, and implanted medical devices, as well as recommended lifestyle modifications.
Chronic heart failure describes the heartâs inability to pump enough blood through the body and provide a sufficient supply of oxygen. This is caused by a weaker than a normal heart. CHF is most common in men and risk factors include age, high blood pressure, being overweight and the presence of metabolic disorders like diabetes. CHF is as its name describes – it is a long-term condition that can get worse over time. It generally cannot be cured but it can be medically managed.7
Acc/aha Stages Of Heart Failure
American Heart Association and the American college of cardiology worked together to create another classification system that complements the NYHA approach. The American college of cardiology and the American heart association staging system describes four stages.
Recommended Reading: What Is Low Heart Rate
Classification Of Heart Failure
A panel of medical experts open a discussion surrounding heart failure and its prevalence in health care.
Ryan Haumschild, PharmD, MS, MBA: Hello, and welcome to this AJMC® Peer Exchange program titled, A Population Health Approach to Managing Heart Failure. Im Dr Ryan Haumschild, the director of pharmacy services at Emory Healthcare in the Winship Cancer Institute. Joining me today in this discussion are my colleagues, Dr Jim Januzzi, a cardiologist at the Massachusetts General Hospital and trustee at the American College of Cardiology Dr Rohit Uppal, the chief clinical officer of hospitalist services at TeamHealth Dr Jaime Murillo, the senior vice president and chief cardiometabolic health officer at UnitedHealth Group and Dr John Anderson, practicing internal medicine and diabetes at TriStar Centennial Medical Center. Our panel of experts will explore opportunities for treating heart failure and evaluating the application of the newly updated guidelines. Thank you and lets begin.
Transcript edited for clarity.
New York Heart Association Classification
Doctors usually classify patients’ heart failure according to the severity of their self-reported symptoms. The classification system used most often is the New York Heart Association Functional Classification. Four levels of clinical classification are used to classify people according to symptoms and limitations experienced during physical activity. Symptom severity is compared to normal breathing, shortness of breath, and/or angina .1 Classification of heart failure based on function during physical activity, often called exertion, is often an important indicator of prognosis.1,2
- Class I: No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF.
- Class II: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF.
- Class III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF.
- Class IV: Symptoms occur even at rest discomfort with any physical activity. Unable to carry on any physical activity without symptoms of HF.
Class I and II are typically considered mild heart failure, while class III and IV are considered more severe or advanced heart failure. A person can move back and forth between these classes as they are based on symptoms. When a patient has a heart failure exacerbation, they will have more symptoms and likely be a higher class, but when their symptoms are better controlled, they will be a lower class.
Recommended Reading: Heart Shaped Lips Surgery
Clinical Manifestations Of Heart Failure
The clinical manifestation of heart failure is largely influenced by the primary side of dysfunction as left sided, right sided or biventricular. Left ventricular dysfunction increases pulmonary pressure and consequently pulmonary congestion occurs leading to dyspnoea and tachypnoea . As the peripheral circulation is reduced , renal dysfunction, peripheral malperfusion and malabsorption of nutrition with the signs of cardiac cachexia develop. In a chronic state, the permanent activation of neurohumoral systems lead to further volume overload , peripheral vasoconstriction , increased heart rate at rest and during exercise, and to a further deterioration of the cardio-renal system. Anemia , increased pulmonary pressure and muscle fatigue deteriorate the symptoms of dyspnoea as well. Overload of the heart leads to enlargement of the heart itself and as a measure the cardiothoracic index increases with leftward shift of the palpable cardiac pulsation. Mostly in volume overload situations filling volume of the ventricle increases periodically and a typical 3rd or 4th heart sound as protodiastolic gallop occurs . In consequence, heart failure influences almost all organ systems and thus heart failure is a systemic disease or a syndrome with a broad clinical spectrum.
Overproduction Of Reactive Oxygen Species
Activated oxidative stress has been demonstrated in animal studies as well as in human studies to cause heart failure also lowered antioxidant activity in failing human hearts promotes oxidative stress . Furthermore, some risk factors for the development of heart failure also show increased oxidative stress i.e., hypertension, diabetes, obesity. Also in myocardial hypertrophy parameters of the redox-sensitive signaling pathways and transcription factors are activated . However, the complete mechanism is not understood yet . There are several factors activated via ROS which may influence contractility: proinflammatory mediators, periods of ischemia, auto-oxidation of catecholamines.
Read Also: Symptoms For Heart Attack In Woman
De Novo Acute Heart Failure
Acute heart failure is broadly defined as a rapid onset of new or worsening signs and symptoms of HF . It is often a potentially life-threatening condition, requiring hospitalisation, and emergency treatment is aimed predominantly at managing fluid overload and haemodynamic compromise. This umbrella term includes patients presenting for the first time with typical symptoms and signs of heart failure and also those with worsening of their pre-existing cardiomyopathy .
De novo AHF occurs when there is a sudden increase in intracardiac filling pressures and/or acute myocardial dysfunction which can lead to decreased peripheral perfusion and pulmonary oedema. The most common aetiology is cardiac ischaemia where -total coronary occlusion leads to decreased contractility in myocardium subtended by the affected coronary artery. In this case, management is focussed not only on haemodynamic compromise but also on reperfusion with the aim of restoring myocardial contractile function.
In addition to myocardial dysfunction, AHF can be precipitated by acute valvular incompetence. This most commonly occurs in an ischaemic context leading to acute mitral regurgitation but can also occur without ischaemia per se as is the case with infective and non-bacterial thrombotic endocarditis. Extra-cardiac pathologies may also precipitate AHF as is the case with pulmonary embolism or pericardial effusion causing tamponade, both of which reduce LV output and therefore reduce peripheral perfusion
Acute Decompensated Heart Failure
The large majority of patients presenting with AHF do so in the context of pre-existing cardiomyopathy, a situation described as acute decompensated heart failure . There are a number of key differences between this group of patients and those presenting with de novo AHF that have implications for how haemodynamic compromise is assessed and how the condition is managed.
Unlike with de novo AHF, patients with ADHF tend to present with signs and symptoms of congestion and fluid retention rather than with pulmonary oedema or cardiogenic shock that characterise acute LV systolic dysfunction. This is the result of the chronic, often dysregulated, neuro-humoral compensatory mechanisms which act to maintain a haemodynamic status quo despite worsening LV function. Decompensation occurs when the balance tips towards fluid overload as the compensatory mechanisms prove inadequate or indeed fail all together. This is borne out by data from the IMPACT-HF registry which shows that acute decompensated heart disease takes a more insidious course and patients present to hospital in extremis following reported symptoms of congestion predating their admission by days or even weeks .
Patients with ADHF present with a more insidious onset complicated by multiple medical co-morbidities and often with congestion as their predominant clinical feature. Management is aimed at treating intercurrent precipitants and encouraging adherence to disease-modifying therapy.
Recommended Reading: How To Stop Symptoms Of Heart Attack
Deterrence And Patient Education
Emphasizing diet and medical compliance to patients with HF is important as one of the most common causes of HF readmission is the failure to comply either with diet or medications. A single session intervention could be beneficial as a randomized control trial of 605 patients with HF found that the incidence of all-cause hospitalization or mortality was not significantly reduced in patients receiving multisession self-care training compared to those receiving a single-session intervention.
Heart Failure Classification In Brief
Heart failure is one of the most complex syndromes caused by the heart not functioning properly. A doctor determines the patients heart failure classifications based on their symptoms and functional limitations.
The severity of heart failure depends on how well the patients heart can pump blood to the body. There are multiple types of Heart failure classification, but the two main ones are the following:
You May Like: Congestive Heart Failure Swollen Feet Treatment
Chronic Heart Failure Classification And Treatment
| Chronic Therapy by Heart Failure Stage | |||
| AHA/ACC Stage | Pt characteristics | ||
| High risk for HF. No structural heart disease. Asymptomatic. | HTN, DM, CAD, cardiotoxin exposure. FHx of CMP | Tx focuses on reducing modifiable risk factors, including mgt of HTN, HLD, DM, SVT, Stop smoking, decr. alcohol incr. exercise. | |
| B | Structural heart disease present. Asymptomatic. | Prior MI, decreased EF, LVH or asx valvular disease | Do everything as for stage A, PLUSACEI/ARB & BB if MI/CAD or decr. EF. ?ICD. |
| C | Structural heart disease present. Symptomatic: Pt has CHF symptoms . | Overt HF | Everything as for stage A, PLUS-ACEI, BB, Diuretics, Sodium restriction.Consider aldosterone antagonist, ICD, CRT.Consider nitrates/hydralazine, digoxin |
| Refractory HF requiring specialized interventions | Sx despite max med tx.4-year mortality > 50% | Everything as for stages A-C, PLUSIV inotropes, VAD, transplant. End of life care. |
*Stage A& B, there is no HF yet.BB=Beta blockers ICD = Implantable Cardiac Defibrillator CRT = Cardiac Resynchronization Therapy.
VAD = Ventricular Assist Device.CRT is one of the last devices you use before you get to VAD and heart transplant. Watch this video.
From AAFP
| NYHA Classification | |
| Severe limitation | Symptoms at rest |
Systolic Versus Diastolic Heart Failure
- Systolic Dysfunction: The left ventricular ejection fraction is reduced in systolic dysfunction and there is depressed contractility of the heart.
- Diastolic Dysfunction: The left ventricular ejection fraction is preserved in diastolic dysfunction and there is an abnormality in myocardial relaxation or excessive myocardial stiffness. Systolic and diastolic dysfunction commonly occur in conjunction with each other.
Recommended Reading: How To Get Target Heart Rate
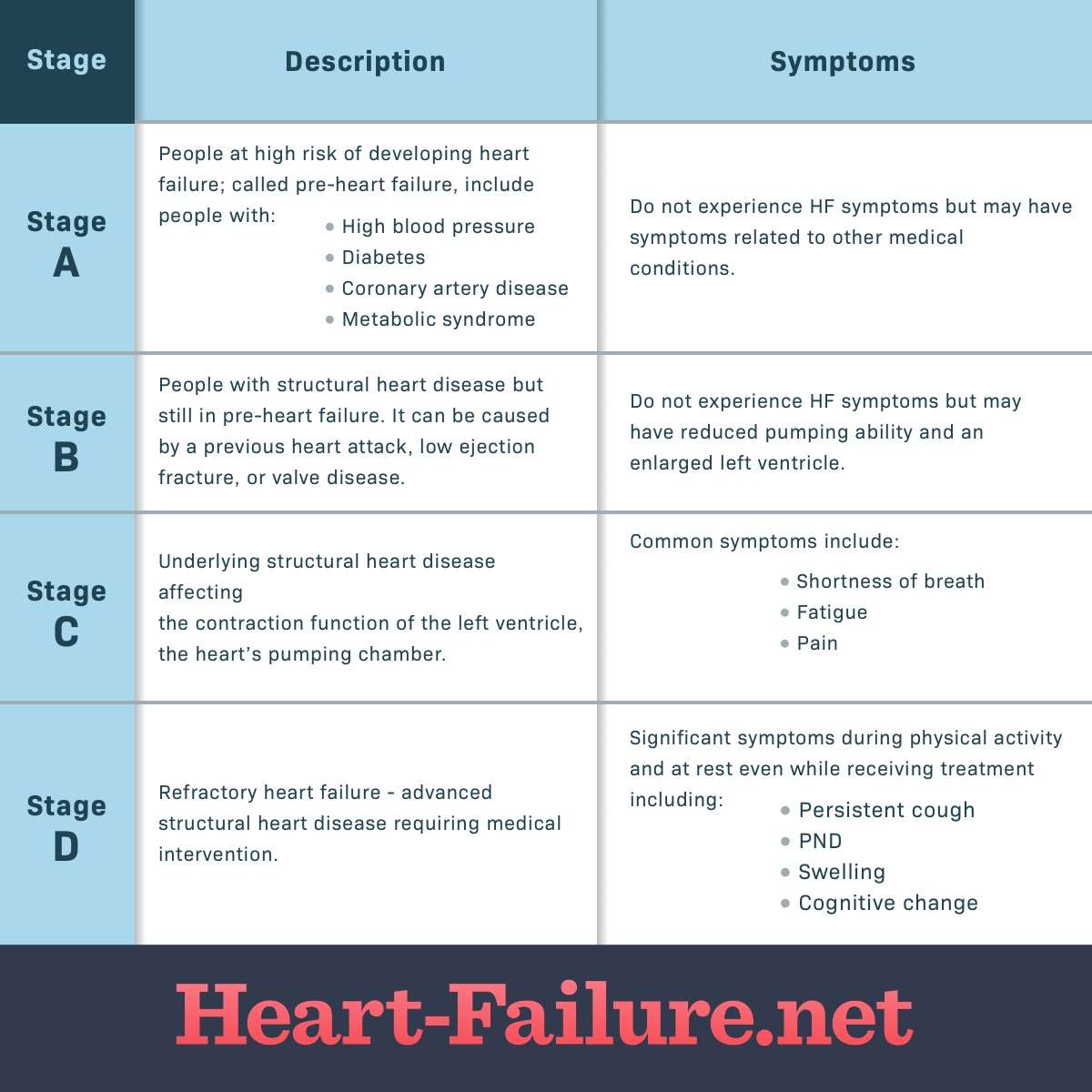
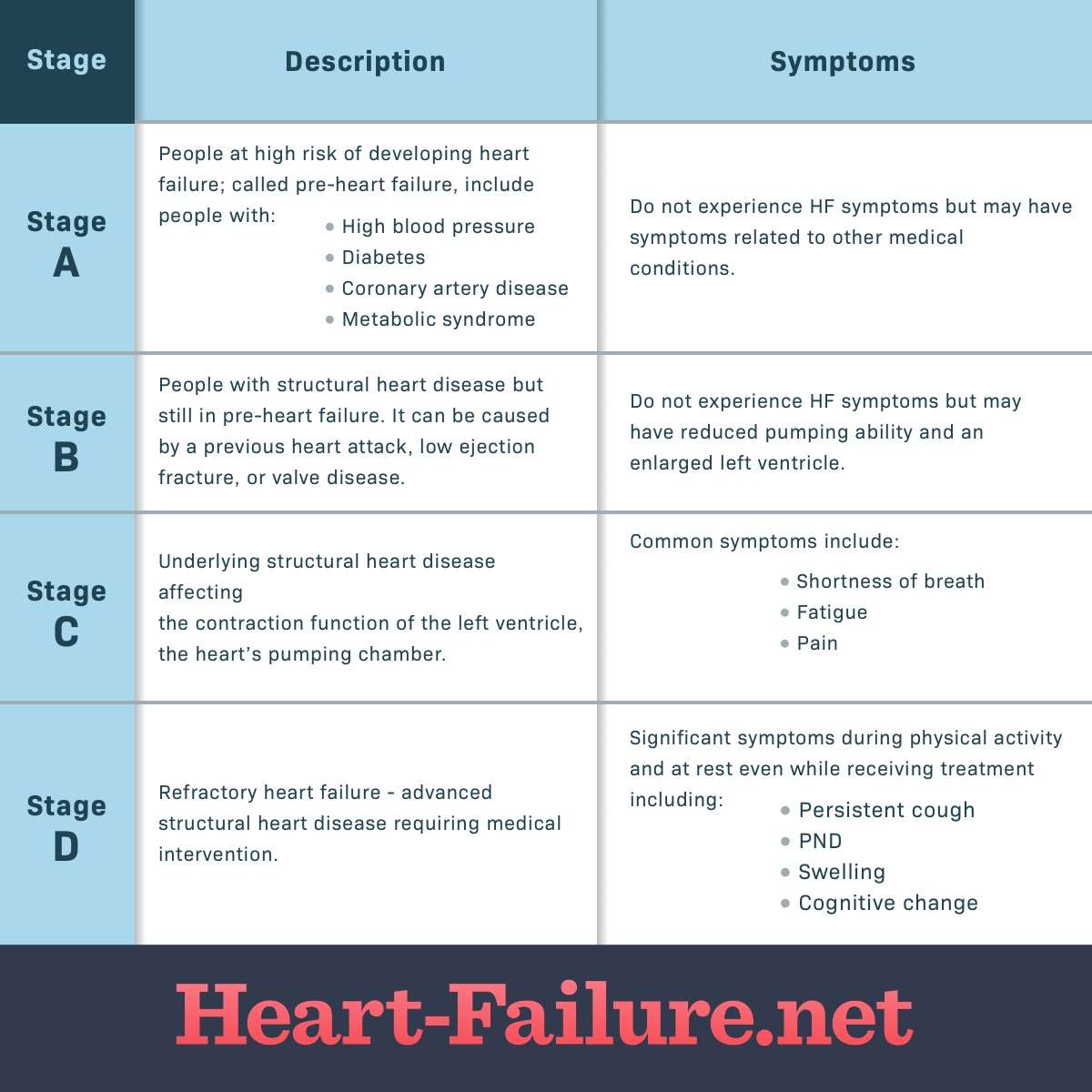
American College Of Cardiology/american Heart Association Classification
The American College of Cardiology/American Heart Association classification of heart failure stages focus more on the condition’s structural impact on the heart, such as the measurement of ejection fraction:
- Stage A: You do not have any structural disorder of the heart, but are at high risk for developing congestive heart failure due to a family history of heart failure or a personal history of hypertension, diabetes, coronary artery disease, alcohol abuse, viral infections, or use of drugs that are toxic to the heart.
- Stage B: You have a structural disorder of the heart, but no symptoms of heart failure .
- Stage C: You have a structural disorder of the heart and you have currently or previously displayed symptoms of heart failure.
- Stage D: People in this final stage of heart failure do not get better with treatment.
Stages Of Heart Failure
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Stage A
Presence of heart failure risk factors but no heart disease and no symptoms
Stage B
Heart disease is present but there are no symptoms
Stage C
Structural heart disease is present AND symptoms have occurred
Stage D
Presence of advanced heart disease with continued heart failuresymptoms requiring aggressive medical therapy
You May Like: Sign Of Congestive Heart Failure In Dogs
Funding Support And Author Disclosures
Dr. Lam has received research support from Boston Scientific, Bayer, Roche Diagnostics, AstraZeneca, Medtronic, and Vifor Pharma serves as a consultant or on the Advisory Board/Steering Committee/Executive Committee for Abbott Diagnostics, Amgen, Applied Therapeutics, AstraZeneca, Bayer, Biofourmis, Boehringer Ingelheim, Boston Scientific, Corvia Medical, Cytokinetics, Darma Inc., Us2.ai, JanaCare, Janssen Research & Development LLC, Medtronic, Menarini Group, Merck, MyoKardia, Novartis, Novo Nordisk, Radcliffe Group Ltd., Roche Diagnostics, Sanofi, Stealth BioTherapeutics, The Corpus, Vifor Pharma, and WebMD Global LLC and serves as cofounder and nonexecutive director of Us2.ai. Dr. Solomon has received grants paid to his institution for chairing PARAGON-HF from Novartis has received grants paid to Brigham and Womens Hospital from Alnylam, Amgen, AstraZeneca, Bayer, Bellerophon, Bristol Myers Squibb, Celladon, Cytokinetics, Gilead, Celladon, Eidos, GlaxoSmithKline, Ionis, Lone Star Heart, Mesoblast, MyoKardia, the National Institutes of Health/National Heart, Lung, and Blood Institute, Novartis, Sanofi Pasteur, and Theracos and has received consulting fees from Alnylam, Amgen, AoBiome, AstraZeneca, Bayer, Bristol Myers Squibb, Cardiac Dimensions, Corvia, Cytokinetics, Daichi-Sankyo, Gilead, GlaxoSmithKline, Ironwood, Janssen, Merck, MyoKardia, Novartis, Quantum Genomics, Roche, Takeda, Tenaya, and Theracos.
Nyha Classification For Chronic Heart Failure
Last reviewed 01/2018
New York Heart Association classification is used to grade the severity of functional limitations in a patient with heart failure :
- class I no limitation of physical activity
- ordinary physical activity does not cause fatigue, breathlessness or palpitation
According to a study conducted, the following criteria were used by cardiologists to determine the NYHA class of a patient :
- self reported walking distance – 70%
- difficulty in climbing stairs – 60%
- ability to walk to local landmarks – 30%
- breathlessness interferes with daily activities – 23%
- breathless when walking around the house – 23%
- no specific questions – 13%
This study has also pointed out that NYHA classification system is subjective and poorly reproducible since there are no clear standard criteria for assigning an NYHA class .
Note:
Reference:
Don’t Miss: Reversing Congestive Heart Failure
