Symptoms And The Severity Of Heart Failure
Once a diagnosis of heart failure has been established, symptoms may be used to classify the severity of heart failure and should be used to monitor the effects of therapy. However, as noted subsequently, symptoms cannot guide the optimal titration of neurohormonal blockers. The New York Heart Association classification is in widespread use . In other situations, the classification of symptoms into mild, moderate, or severe is used. Patients in NYHA class I would have to have objective evidence of cardiac dysfunction, have a past history of heart failure symptoms and be receiving treatment for heart failure in order to fulfil the basic definition of heart failure.
-
There is a poor relationship between symptoms and the severity of cardiac dysfunction., However, symptoms may be related to prognosis particularly if persisting after therapy.
In acute myocardial infarction, the classification described by Killip has been used to describe symptoms and signs. It is important to recognize the common dissociation between symptoms and cardiac dysfunction. Symptoms are also similar in patients across different levels of ejection fraction. Mild symptoms should not be equated with minor cardiac dysfunction.
What Are The Most Common Symptoms Of Congestive Heart Failure
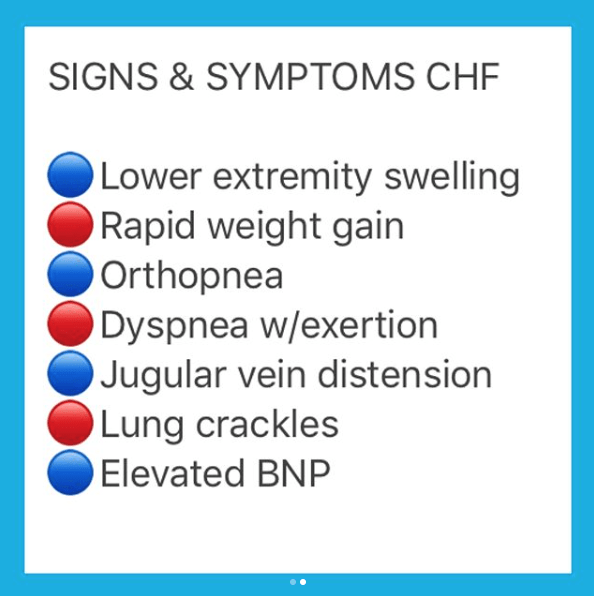
Swelling is the most common symptom of congestive heart failure. Often, swelling is most apparent in the extremities, especially in the legs and ankles, but it can occur in other parts of the body as well. Fluid collection in and around the lungs can cause shortness of breath , especially during physical activity or when lying down. Other common symptoms of heart failure include fatigue, loss of appetite, and weight gain.
Aspects Of The Pathophysiology Of The Symptoms Of Heart Failure Relevant To Diagnosis
The origin of the symptoms of heart failure is not fully understood. Increased pulmonary capillary pressure is undoubtedly responsible for pulmonary oedema in part, but studies conducted during exercise in patients with CHF demonstrate only a weak relationship between capillary pressure and exercise performance., This suggests either that raised pulmonary capillary pressure is not the only factor responsible for exertional breathlessness or that current techniques to measure true pulmonary capillary pressure may not be adequate. Variation in the degree of mitral regurgitation will also influence breathlessness.
Read Also: Does Arousal Increase Heart Rate
What Other Tests May Be Used To Assess Cardiac Risk
Some other tests that may be used to assess cardiac risk include:
- High-sensitivity C-reactive protein : Studies have shown that measuring CRP with a high sensitivity test can help identify risk of CVD. This test is different from the regular CRP test, which detects elevated levels of CRP in people with infections and inflammatory diseases. The hs-CRP test measures CRP that is in the normal range for healthy people. It can be used to distinguish people with low normal levels from people with high normal levels. High normal levels of hs-CRP in otherwise healthy individuals have been found to be predictive of the future risk of heart attack, stroke, sudden cardiac death, and peripheral arterial disease, even when lipid levels are within acceptable ranges. Several groups have recommended that this test be used for people with moderate risk of heart attack over the next 10 years. However, there is not a consensus on how the test should be used otherwise, nor on how frequently the test should be repeated.
- Lipoprotein A ): Lp is a lipoprotein consisting of an LDL molecule with another protein ) attached to it. Lp is similar to LDL-C but does not respond to typical strategies to lower LDL-C such as diet, exercise, or most lipid-lowering drugs. Since the level of Lp appears to be genetically determined and not easily altered, the presence of a high level of Lp may be used to identify individuals who might benefit from more aggressive treatment of other risk factors.
Third And Fourth Heart Sounds
A double apical impulse can represent an auscultated third heart sound . Just as with the displaced point of maximal impulse, a third heart sound is not sensitive for heart failure, but it is highly specific .14 Patients with heart failure and left ventricular hypertrophy can also have a fourth heart sound . The physician should be alert for murmurs, which can provide information about the cause of heart disease and also aid in the selection of therapy.
Recommended Reading: Why Do Nsaids Increase Risk Of Heart Attack
How Will I Find Out If I Have Heart Failure
Your doctor will diagnose heart failure based on your medical history, a physical exam, and test results. Bring a list of your symptoms to your appointment, including how often they happen and when they started. Also, bring a list of any prescription and over-the-counter medicines you take. Let your provider know if you have any risk factors for heart failure.
You may also be referred to a cardiologist for these tests and treatment. A cardiologist is a doctor who specializes in diagnosing and treating heart diseases.
How Can I Prevent Heart Failure
You can prevent heart failure by preventing coronary heart disease and heart attack. The best way to do this is to reduce or eliminate the risk factors that lead to heart failure. You could:
- drink alcohol in moderation
- reduce stress and look after your mental wellbeing
If you have had a heart attack, its even more important to manage your risk factors and follow your treatment plan. Make sure you check in frequently with your healthcare team.
Some risk factors such as your age, whether you have other health conditions, or your genes may be outside your control. Speak with your doctor if you have concerns about developing heart failure, and how you can manage it.
Don’t Miss: How Do You Calculate Your Heart Rate
What Causes Heart Failure
Although the risk of heart failure doesnt change as you get older, youre more likely to have heart failure when youre older.
Many medical conditions that damage the heart muscle can cause heart failure. Common conditions include:
- Tobacco and recreational drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
Biomarkers Indications For Use
Abbreviations:ACC: American College of Cardiology, AHA: American Heart Association, ADHF: acute decompensatedheart failure, BNP: B-type natriuretic peptide, COR: Class of Recommendation, ED: emergency department, HF: heart failure, NT-proBNP: N-terminal pro-B-type natriuretic peptide, NYHA: New York Heart Association, pts: patients
Other biomarkers of injury or fibrosis include soluble ST2 receptor, galectin-3, and high-sensitivity troponin.
Read Also: Icd 10 Code Congestive Heart Failure
What Are The Types Of Heart Failure
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure
Heart failure with reduced left ventricular function The lower left chamber of your heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of your body.
Heart failure with preserved left ventricular function Your heart contracts and pumps normally, but the bottom chambers of your heart are thicker and stiffer than normal. Because of this, your ventricles can’t relax properly and fill up all the way. Because there’s less blood in your ventricles, your heart pumps out less blood to the rest of your body when it contracts.
Right-sided heart failure
Heart failure can also affect the right side of your heart. Left-sided heart failure is the most common cause of this. Other causes include certain lung problems and issues in other organs.
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Also Check: What Supplies Blood To The Heart
Angiotensin Ii Receptor Blockers
For patients with left ventricular systolic dysfunction:In NYHA class III patients remaining symptomatic despite therapy with diuretics, ACE-inhibitors, and beta-blockers, there is no definite evidence for the recommendation of next addition an ARB or an aldosterone antagonist to reduce further heart failure hospitalizations or mortality.
-
Angiotensin II receptor blockers can be used as an alternative to ACE inhibition in symptomatic patients intolerant to ACE-inhibitors to improve morbidity and mortality .
-
ARBs and ACE-inhibitors seem to have similar efficacy in CHF on mortality and morbidity . In acute myocardial infarction with signs of heart failure or left ventricular dysfunction ARBs and ACE-inhibitors have similar or equivalent effects on mortality .
-
ARBs can be considered in combination with ACE-inhibitors in patients who remain symptomatic, to reduce mortality and hospital admissions for heart failure .,,
Concerns raised by initial studies about a potential negative interaction between ARBs and beta-blockers have not been confirmed by recent studies in post-myocardial infarction or CHF .,
Dosing
Initiation and monitoring of ARBs, which are outlined in Table , are similar to procedures for ACE-inhibitors. Available ARBs and the recommended dose levels are shown in Table .
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Recommended Reading: What Happens With Congestive Heart Failure
Rest Exercise And Exercise Training
Rest
In acute heart failure or destabilization of CHF, physical rest or bed rest is recommended.
Exercise
Exercise improves skeletal muscle function and therefore overall functional capacity. Patients should be encouraged and advised on how to carry out daily physical and leisure time activities that do not induce symptoms. Exercise training programs are encouraged in stable patients in NYHA class IIIII. Standardized recommendations for exercise training in heart failure patients by the European Society of Cardiology have been published.
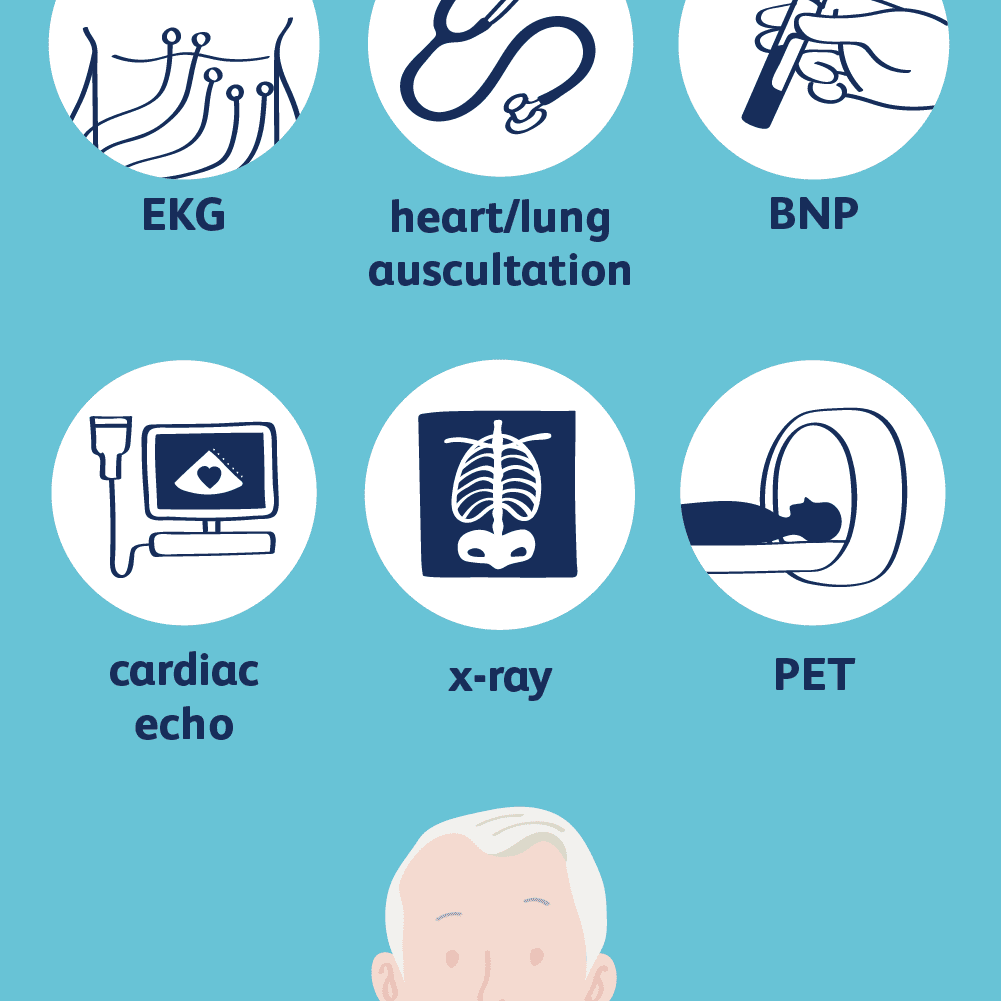
How Is Congestive Heart Failure Diagnosed
Diagnosis of congestive heart failure is achieved through a comprehensive assessment of the heart muscle, including evaluation of its pumping action and thickness of its walls. This testing also helps to determine the underlying cause of heart failure. Diagnostic tests for congestive heart failure may include:
- Resting or exercise electrocardiogram
- Biopsy or catheterization of the heart and arteries
Recommended Reading: Do Heart Attacks Go Away
Risk Factors And Symptoms
Risk factors for cardiomyopathy and heart failure include a family history of coronary artery disease, a previous heart attack, excessive alcohol consumption, drug abuse, and obesity. Certain conditions can also increase risk, including high blood pressure, diabetes, thyroid disorders, a buildup of iron in the heart muscle, and sarcoidosis, which causes inflammation in the bodys organs. Cancer treatments, including radiation and certain types of chemotherapy, may also increase a persons risk.
In its earliest stages, cardiomyopathy and heart failure may not cause noticeable symptoms. However, as the condition progresses, a person may experience fatigue or shortness of breath, especially with physical exertion. They may also have swelling of the legs, feet, and abdomen, which occurs when the body overproduces fluid in response to a reduction in blood pumped from the heart. Other symptoms include heart palpitations or lightheadedness caused by irregular heartbeats, or arrhythmias.
When Should I Call An Ambulance
If you have any of the symptoms below, call triple zero immediately and ask for an ambulance. If calling triple zero does not work on your mobile phone, try calling 112.
- chest pain thats severe or worsening, or has lasted longer than 10 minutes
- chest pain that feels heavy, crushing or tight
- other symptoms, such as breathlessness, nausea, dizziness or a cold sweat
- pain in your jaw or down your left arm
Don’t Miss: How To Lower My Resting Heart Rate
Heart Replacement Therapies: Heart Transplantation Ventricular Assist Devices And Artificial Heart
Heart transplantation
Patients who should be considered for heart transplantation are those with severe symptoms of heart failure with no alternative form of treatment and with a poor prognosis. The introduction of new treatments has probably modified the prognostic significance of the variables traditionally used to identify heart transplant candidates i.e. VO2 max . The patient must be willing and capable to undergo intensive medical treatment, and be emotionally stable so as to withstand the many uncertainties likely to occur both before and after transplantation. The contraindications for heart transplantation are shown in Table .
-
Heart transplantation is an accepted mode of treatment for end stage heart failure. Although controlled trials have never been conducted, it is considered to significantly increase survival, exercise capacity, return to work and quality of life compared with conventional treatment, provided proper selection criteria are applied .
Besides shortage of donor hearts, the main problem of heart transplantation is rejection of the allograft, which is responsible for a considerable percentage of deaths in the first postoperative year. The long-term outcome is limited predominantly by the consequences of immuno-suppression .
Ventricular assist devices and artificial heart
Physical Exam For Heart Failure
First, your doctor will want to know if you:
- Have other conditions such as diabetes, kidney disease, angina, high blood pressure, or other heart problems
- Smoke
- Drink alcohol, and how much
- Take medications, and which ones
Your doctor will also do a physical exam. They’ll look for signs of heart failure as well as other illnesses that may have weakened your heart.
During your visit, your doctor will:
- Listen to your heart
- Check your blood pressure
Theyâll also look at your appearance while you sit, do mild activity, and lie flat. People with mild or moderate heart failure may appear comfortable at rest, but when active, they often become short of breath. Those with heart failure may be uncomfortable if they lie flat for a few minutes.
Your doctor may check for fluid in your lungs with a stethoscope. People with heart failure may also have neck veins that are larger than normal, swelling of the legs or abdomen, or an enlarged liver.
Read Also: What’s My Resting Heart Rate
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
Point Of Maximal Impulse
The point of maximal impulse of the left ventricle is usually located in the midclavicular line at the fifth intercostal space. With the patient in a sitting position, the physician uses fingertips to identify this point. Cardiomegaly usually displaces the cardiac impulse laterally and downward.
At times, the point of maximal impulse may be difficult to locate and therefore loses sensitivity . Yet the location of this point remains a specific indicator for evaluating the size of the heart.14
Don’t Miss: How Do You Lower Your Heart Rate
