Data Sources And Search
We searched for randomized trials in CINAHL , the Cochrane Collaboration Central Register of Controlled Trials , Embase , Medline/PubMed , and Web of Science . We restricted our searches to human studies, clinical trials, and controlled or randomized trials. We used the keywords and medical subject headings adrenergic beta-antagonists, heart failure, and congestive, as well as additional text words in combination with an established search strategy for Medline/PubMed.1112 We also hand searched bibliographies of identified studies, recent meta-analyses of blockers in heart failure, heart failure guidelines, and 2008-11 conference proceedings of the American College of Cardiology, American Heart Association, and European Society of Cardiology scientific sessions. We restricted our search to publications in the English language.
Definition Of Heart Failure
Congestive heart failure is a broad term used to describe a clinical condition resulting from the inability of the heart to adequately pump blood and causing symptoms such as orthopnea, dyspnea on exertion and edema. In practice, congestive heart failure is used to describe these symptoms whether they result from diastolic dysfunction, which is a condition of impaired ventricular filling, or systolic dysfunction, which is a condition of impaired ventricular emptying.
As the understanding of heart failure has advanced, it has become important to separate systolic dysfunction from diastolic dysfunction because the etiology, treatment and prognosis of these disorders is quite different. The discussion in this article is limited to heart failure resulting from left ventricular systolic dysfunction, defined as an ejection fraction of less than 40 percent.
Withdrawal From Beta Blockers
All of the side effects mentioned above are reversible when discontinuing the drug. However, it is very important that if a beta-blocker needs to be discontinued, that it be gradually tapered. Stopping beta-blockers abruptly can cause withdrawal syndrome, leading to high heart rate and high blood pressure.
There have also been reports of heart attacks with abrupt discontinuation. For this reason, it is very important that if you need to discontinue therapy that you speak to your doctor about a taper schedule.5
Do you take a beta-blocker? Have you experienced any of the side effects mentioned above? Share your experiences below!
Read Also: Can Low Heart Rate Cause Dizziness
Initiation Of Beta Blocker Therapy
Appropriate candidates for beta blocker therapy should be evaluated thoroughly before treatment is initiated. The evaluation should include a comprehensive history and physical examination, with special emphasis on the assessment of functional capacity and the appropriateness of diuretic therapy. An electrocardiogram should be obtained to exclude the presence of high-degree heart block. An approach to the evaluation and treatment of patients with chronic heart failure is presented in Figure 1.14
Benefits Of Blockers In Patients With Heart Failure And Reduced Ejection Fraction: Network Meta
- Accepted 28 December 2012
You May Like: How Much Aspirin Should I Take To Prevent Heart Attack
Minor Risks Of Beta Blockers
Many people choose not to take beta-blockers due to concerns of depression and sexual dysfunction, which this class of medications has been linked to. However, studies have shown that the risk is very low. To summarize these trials:4
- Beta blockers do not increase the risk of depression.
- There is a small increase in the risk of sexual dysfunction. To put this risk into perspective, for every 200 people treated with a beta blocker, one person will experience sexual dysfunction.
If you are concerned about these side effects, it is a good idea to have a discussion with your doctor, as your underlying health factors can further predict these risks.
Strength And Limitation Of The Study
The strength of our study is the prospective collection of data, which enables for accurate evaluation of the data related to treatment, clinical and laboratory parameters. Our study is the first to have full report on treatment optimization of beta blockers in Ethiopia. Hence, this finding may enhance future intervention to optimize beta-blockers use in patients with chronic HF.
Although we have attempted to assess various factors that might influence the utilization of beta blockers, we did not assess the impact of health professionals level of knowledge on the utilization of beta blockers. This study may not provide adequate evidence regarding the cause-effect relationship of beta-blocker utilization and its risk factors due to the inherent characteristics of cross-sectional study. Our study is a single center study therefore, it might not be generalized to the general population. Moreover, as the findings of this study could be affected by the differences in participants characteristics, disease distribution, healthcare infrastructure, and methods employed, they should be extrapolated to other countries with caution.
Also Check: Can Beer Cause Heart Attack
What Is The Clinical Evidence Of Benefit From
Lancet.Br Heart J.
Eur Heart J.
absolute
- MERIT-HF Study Group
- et al.
JAMA.
- Sackner-Bernstein JD
- et al.
Circulation.
- Goldsmith RL
- et al.
Circulation.Am J Cardiol.Circulation.
Double-blind, placebo-controlled study of the long-term efficacy of carvedilol in patients with severe chronic heart failure.Circulation.1995 92: 1499-1506 |
| Multicenter Oral Carvedilol Heart Failure |
Assessment
Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure.Circulation.1996 94: 2807-2816 |
Double-blind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure: the PRECISE Trial.Circulation.1996 94: 2793-2799 |
| Australia/New Zealand Heart Failure Research Collaborative GroupRandomised, placebo-controlled trial of carvedilol in patients with congestive heart failure due to ischaemic heart disease.Lancet.1997 349: 375-380 |
A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure.N Engl J Med.2001 344: 1659-1667 |
Beneficial effects of metoprolol in idiopathic dilated cardiomyopathy.Lancet.1993 342: 1441-1446 |
Adverse Effects Of Beta
- Reactions 0 reactions
If you have been diagnosed with Heart Failure , you may have been prescribed a beta-blocker. A beta-blocker is a class of medications commonly used to treat HF, high blood pressure, heart attacks, and arrhythmias. While these drugs are life-saving, they come equipped with adverse effects. Knowing and understanding how to manage these side effects will help you navigate your new treatment.
You May Like: What Does Low Resting Heart Rate Mean
Why Beta Blockers Work
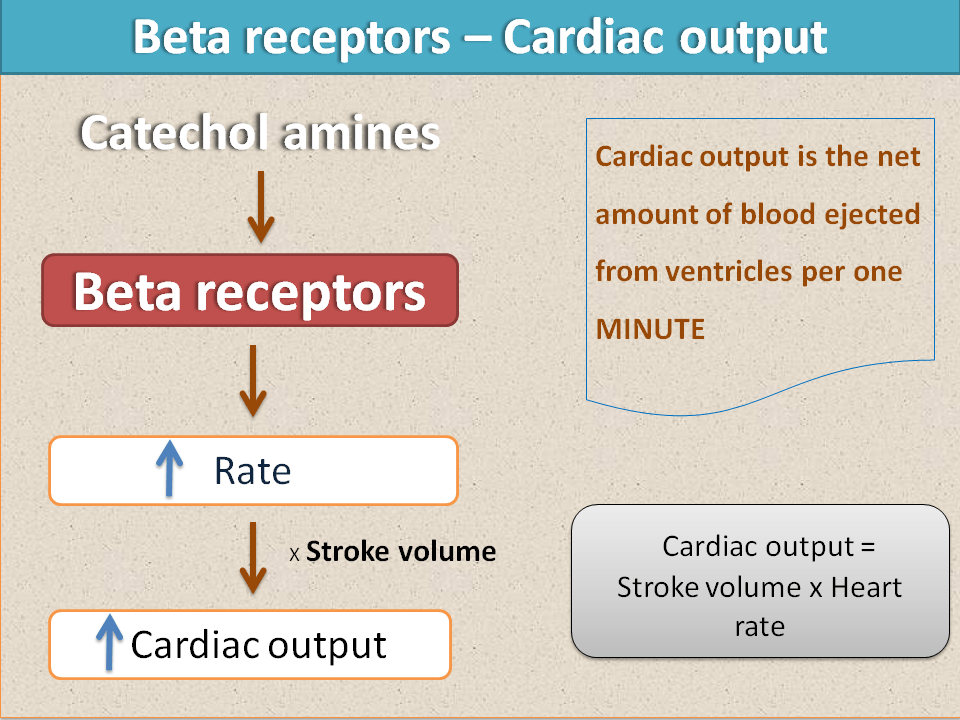
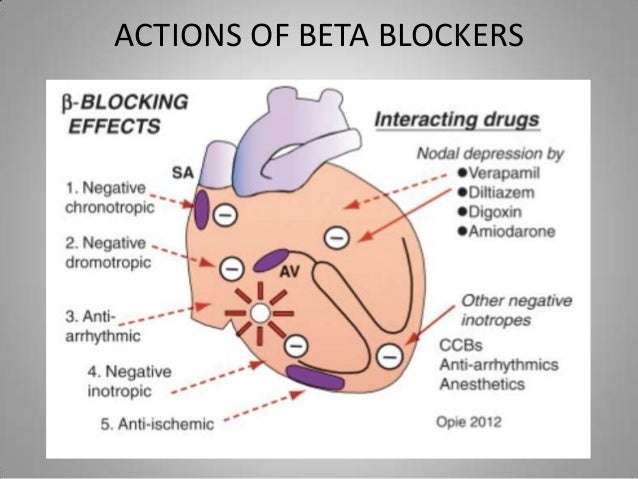
Left ventricular systolic dysfunction is associated with activation of a host of interconnected neurohormonal adaptive mechanisms, most notably the sympathetic and renin-angiotensin-aldosterone systems. Chronic activation of these mechanisms exerts deleterious hemodynamic and direct cardiotoxic effects and contributes to the progressive deterioration of ventricular function. Attenuation of these mechanisms is associated with improvement in survival. This has been demonstrated for angiotensin-converting enzyme inhibitors,912 beta blockers18 and spironolactone,13 and is suggested for other classes of drugs under evaluation.
Comparison With Other Studies
A previous retrospective study attempted to compare different blockers in clinical use by using data from an administrative database.53 The authors concluded that atenolol and acebutolol were superior to metoprolol in reducing mortality in patients, whereas carvedilol and bisoprolol were not superior to metoprolol in improving survival. The population studied in that analysis was quite different from the population of randomized trials assessed in our studythe mean age of the population of that study was 77 years, whereas the mean age of the population in our analysis was 61 years, and the percentage of male patients was 49% in the study, whereas male patients comprised 76% of the population in our analysis. Also, ejection fraction was not accounted for in the analysis of the retrospective study, whereas the mean ejection fraction of the population in our analysis was 26%. Hence, the difference from our study, which pooled data from randomized trials only, can likely be explained by differences in the population studied and differences in the analytic methods.
Also Check: How To Stop Symptoms Of Heart Attack
Data Synthesis And Analysis
We report categorical outcomes as numbers and continuous outcomes as median . We derived the raw event rates from individual studies and constructed 2×2 tables with raw number of events and total population of the trial. In trials that did not report raw event rates, investigators reported the percentage or proportion of patients having the event under consideration, which we rounded off to whole numbers by using the sample size of the population we then calculated the risk difference by using the formula 1/, where OR=odds ratio. We calculated number needed to treat and corresponding absolute risk reduction from the 2×2 tables. We abstracted data in duplicate, and the inter-rater agreement was good . Considering different lengths of follow-up for individual trials, and to account for censored data, we obtained the rates of outcomes for all trials with follow-up longer than 12 months and calculated the log hazard ratios from the event rates reported and mean duration of follow-up. We did standard pair-wise meta-analysis comparing blockers with comparators, with 95% confidence intervals. We also used a random effect model to calculate prediction intervals for all cause mortality, using RevMan v5.1 and Stata version 11. We assessed and quantified heterogeneity with the help of the I2 statistic computed with the Cochran Q test.
Optimizing The Use Of
- Peripheral congestion: -Blockers should not be initiated in patients with moderate to severe fluid retention . Because HFrEF is a progressive disease, it is likely that, during its course, many patients will develop signs and symptoms related to fluid retention. The initial approach to these patients is based on fluid management, often increasing the dose or adding a second diuretic . In the presence of congestion, initiation of therapy or increase in -blocker dosage should be deferred until euvolemia is achieved . In general, discontinuation or dose reduction of a -blocker is not indicated in the presence of congestion unless it is associated with hypoperfusion .
- Asymptomatic hypotension: This is common in patients with HFrEF and is not a contraindication to -blocker therapy . It is essential to consider whether hypotension is caused by an inadequate preload related to aggressive use of diuretics or vasodilators . In such cases, it may be necessary to reduce or suspend these therapies.
- Symptomatic bradycardia: -Blockers may be used in patients with asymptomatic, mild bradycardia, particularly when the heart rate increases with exercise . The possibility of drug interactions that may lower the heart rate should also be considered . Given the substantial benefits of -blockers in HFrEF, asymptomatic bradycardia during -blocker therapy is not a reason to discontinue it, and cardiac pacing should be considered on an individual basis .
Recommended Reading: How Many Types Of Heart Bypass Surgery
Beta Blocker Side Effects
Before prescribing a beta-blocker, your doctor will ensure that the medication is safe and indicated. Some potential risks and unwanted side effects of beta-blockers are outlined below.
- Weight gain: Fat accumulation is more likely with the older agents, such as metoprolol and atenolol. Weight gain usually occurs in the first initial months of treatment, but stops and reaches a plateau thereafter. The average weight gain is 1.2 kg.1
- Low blood sugars: This drugs class can worsen or extend a period of hypoglycaemia, or low blood sugar levels. This is especially concerning for people with diabetes. Beta-blockers can also mask the symptoms of low blood sugar, which may be problematic if people rely on symptoms alone to determine whether their sugars are low.2
- Worsening asthma and COPD: Some beta-blockers are not recommended for people with severe asthma or COPD, as they may cause narrowing of the respiratory tract and worsen respiratory symptoms. However, it was found that medications commonly used for asthma and COPD such as inhaled steroids are protective against this side effect3.
Effect Of Dose On Mortality And Hospitalization
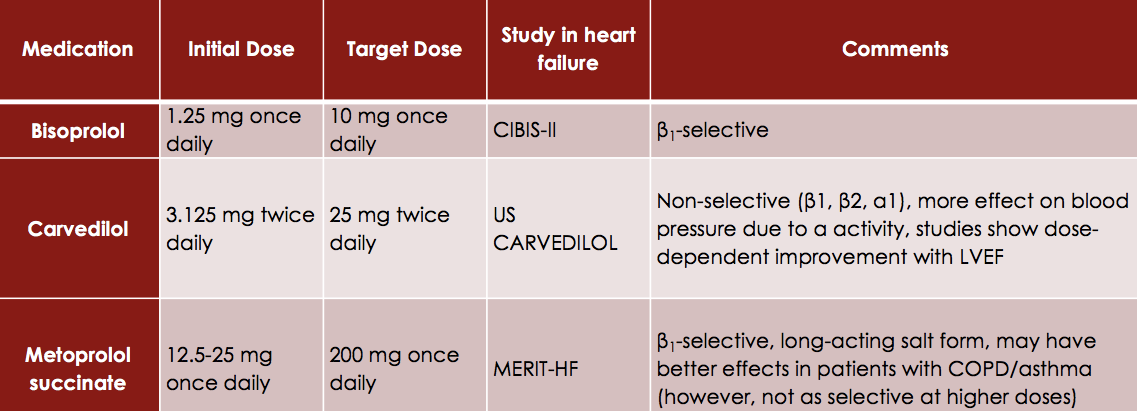
The importance of achieving target doses of beta-blockers in CHF is controversial. CIBIS III data reveal that a higher dose of either bisoprolol or enalapril was independently associated with substantial improvements in the primary endpoint , in survival and in mortality/cardiovascular hospitalization. The association between dose and mortality appeared to be particularly marked for bisoprolol, with patients who received at least half the target dose being 66% less likely to die than those who received lower doses. Dose-related differences in outcome cannot simply be explained by patients who received low doses being sicker at baseline than those who received high doses, as the multivariate analysis was adjusted for 19 baseline characteristics including NYHA class, ejection fraction, age, sex, other drug use, and concomitant disease.
Also Check: How To Calculate Heart Rate From Ecg
Study Design And Study Setting
We conducted a prospective observational study at ambulatory care clinic of Jimma University Medical Center. Jimma University medical center is a teaching and referral hospital that provides service for both outpatient and inpatient. It is a major public hospital in southwest Ethiopia that serves for about 15 million people in the catchment area.
While Pregnant Or Breastfeeding
Beta-blockers may affect a growing baby by slowing its heart rate and lowering its blood sugar level and blood pressure. These drugs can also pass to an infant through breast milk, causing low blood pressure, trouble breathing, and a slow heart rate.
You should tell your doctor if you’re trying to get pregnant or you become pregnant while on beta-blockers or are breastfeeding.
Don’t Miss: What Arm Hurts With Heart Attack
Cibis Iii: Could Beta
It is clear that, for optimum protection, CHF patients should be receiving both a beta-blocker and an ACE inhibitor as early as possible. However, uptitrating the two agents simultaneously is not currently recommended. In the outpatient setting, it is questionable. The question therefore arisescould starting the beta-blocker before the ACE inhibitor be a reasonable approach? This question was addressed by the CIBIS III trial, the first trial examining the optimum order of initiating treatment for CHF. CIBIS III compared starting with the beta1-selective beta-blocker bisoprolol or the ACE inhibitor enalapril, followed by addition of the other agent . It included 1010 patients , who were clinically stable in NYHA class II or III, with an LVEF 35%. They were randomized to bisoprolol or enalapril for 6 months, followed by combination therapy for 624 months. CIBIS III was an open study, but with blinded endpoint evaluation .
Systolic Dysfunction In Heart Failure: Neurohormonal Theory
Left ventricular systolic dysfunction is a mechanical defect that results in the heart’s inability to pump oxygenated blood to peripheral tissues. The impact of this dysfunction is manifested in hemodynamic and physiologic abnormalities, including decreased cardiac output, elevated pulmonary capillary wedge pressure and decreased exercise tolerance. Historically, interventions to treat patients with heart failure have been directed at improving these hemodynamic end points. However, clinical trials found a lack of correlation between hemodynamic improvement and clinical improvement, and new strategies were sought.
Recent studies have revealed a correlation between prognosis in heart failure and plasma levels of such neurohormones as endothelin,14 norepinephrine15 and renin,16 among others. Neurohormones have also been shown to stimulate necrosis, fibrosis and apoptosis in the heart. As a result, a neurohormonal hypothesis has evolved to describe how activation of these neurohormonal systems may cause progression of heart failure.16,17
Don’t Miss: How Do I Find My Heart Rate
Beta Blockers: Use As Directed
When you start taking beta-blockers, your symptoms may become slightly worse for about two to three weeks as your heart adjusts to them. You might feel more tired or dizzy. Thats normal. However, youll need to check your blood pressure and heart rate to make sure they dont drop too low.
Its critical to take beta-blockers as directed. Even if you think they arent working or arent making you feel better, theyre helping prevent your heart disease from getting worse.
Its especially important to continue beta-blockers if youve been taking them long-term. Studies show that abruptly stopping them can cause chest pain and increase your risk of sudden cardiac death.
So, dont stop taking your beta-blockers unless you discuss it with your physician even if theyre causing side effects such as:
- Dizziness or lightheadedness.
- Slow, fast or irregular heartbeat.
- Swelling of feet and lower legs.
- Chest pain but contact your doctor or nurse right away.
If any of these side effects are severe or dont go away, talk to your doctor about how to control them. Sometimes your doctor can:
- Lower your beta-blocker dosage.
- Recommend alternate ways to take your beta-blocker so it doesnt interact with other medications.
Ethics Approval And Informed Consent
Approval for this study was obtained from the institutional review board of Jimma University, College of Health and Medical Sciences. We fully explained the purpose and protocol of the study to all participants included in the study and written informed consent was obtained from each participant. The personal information was entirely confidential and protected. All methods were performed in accordance with the approved institutional guidelines.
You May Like: How To Get Your Resting Heart Rate
Trial Characteristics And Study Quality
As shown in Table , we identified 30 randomized controlled trials of beta-blocker for inclusion in this meta-analysis, which enrolled a total of 24,779 patients . The mean follow-up duration was 11.51 months and all trials are placebo controlled except the trial of Anderson et al. which used standard therapy. Using the Jadad score , all studies were estimated with score of 35 and qualified as high quality. All trials were analyzed according to the intention-to treat paradigm.
Table 1 Randomized trials of beta blockers for the prevention of sudden cardiac death
