Nursing Diagnosis For Cardiovascular Diseases
by Daisy Jane Antipuesto RN MN·August 4, 2009
Cardiovascular diseases are a group of disorders of the heart and blood vessels and include:
- Coronary heart disease disease of the blood vessels supplying the heart muscle
- Cerebrovascular disease disease of the blood vessels supplying the brain
- Peripheral arterial disease disease of blood vessels supplying the arms and legs
- Rheumatic heart disease damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria
- Congenital heart disease malformations of heart structure existing at birth.
- Deep vein thrombosis and pulmonary embolism blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Heart attacks and strokes are usually acute events and are mainly caused by a blockage that prevents blood from flowing to the heart or brain. The most common reason for this is a build-up of fatty deposits on the inner walls of the blood vessels that supply the heart or brain. Strokes can also be caused by bleeding from a blood vessel in the brain or from blood clots.
FACTS ABOUT CARDIOVASCULAR DISEASES
CAUSES OF CARDIOVASCULAR DISEASES
COMMON SYMPTOMS OF CARDIOVASCULAR DISEASES
POTENTIAL NURSING DIAGNOSIS FOR SEVERE HYPERTENSION:
Nursing Care Plan For Bradycardia 4
Nursing Diagnosis: Activity Intolerance related to bradycardia secondary to syncope as evidenced by fatigue, feeling weak, abnormal blood pressure or heart rate in response to activity, ECG changes reflecting arrhythmias or ischemia, and exertional dyspnea.
Desired Outcomes:
- The patient will participate in desired and compulsory activities.
- The patient will demonstrate fewer physiological signs of activity intolerance.
- The patient will demonstrate a measurable rise in activity tolerance.
Congestive Heart Failure Chf Nursing Care Plans Diagnosis And Interventions
Congestive Heart Failure CHF NCLEX Review and Nursing Care Plans
CHF can affect either both sides of the heart or just one side. The three types of CHF are biventricular, left-sided, and right-sided heart failure. In left-sided heart failure, the left ventricle becomes enlarged and becomes dilated together with the left atrium in order to compensate for the increased pressure.
Right-sided heart failure usually happens after left-sided heart failure. Pooling of blood in the left heart chambers causes an increase in pressure, impairing the normal blood drainage from the lungs to the left atrium. The pressure in the pulmonary veins increases, causing the right ventricle to compensate by pumping more vigorously.
In time, the cardiac muscles of the right chambers wear down, causing right-sided heart failure. Failure of both sides of the heart is called biventricular heart failure.
Congestion is one of the common features of heart failure, thus the term congestive heart failure is still used by many medical professionals.
Also Check: Why Do Athletes Have Lower Heart Rate
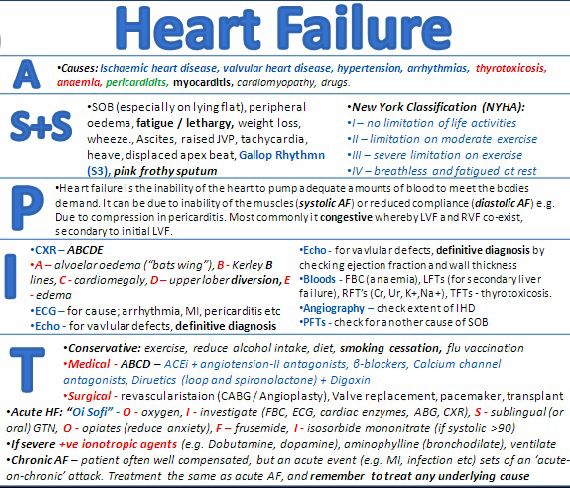
Causes Of Heart Failure
Ineffective Cerebral Tissue Perfusion
May be related to:tissue ischemia, reduction or interruption of blood flow, vasoconstriction, hypovolemia, shunting, depressed ventricular function, dysrhythmias, conduction defects.
As evidenced by:abnormal hemodynamic readings, dysrhythmias, decreased peripheral pulses, cyanosis, decreased blood pressure, shortness of breath, dyspnea, cold and clammy skin, decreased mental alertness, changes in mental status, oliguria, anuria, sluggish capillary refill, abnormal electrolyte, hypoxia, ABG changes, chest pain, ventilation perfusion imbalances, changes in peripheral resistance, impaired oxygenation of myocardium, ECG changes in S-T segment, T wave, U wave, palpitations.
Recommended Reading: Target Heart Rate For Stress Test
Read Also: What Is A Normal.resting Heart Rate
Treatment For Heart Failure
- Angiotensin-converting enzyme inhibitors promotes vasodilation of the blood vessels, lowering the pressure and improving the blood flow .
- Beta blockers reduces heart rate and blood pressure .
- Angiotensin II receptor blockers similar to ACE inhibitors and can be used if the patient does not tolerate ACE inhibitors .
- Digitalis or digoxin improves the contraction of heart muscles, regulate heart rhythm and reduces heartbeat.
- Inotropes to improve the function of the heart to pump blood in severe heart failure.
- Diuretics to facilitate elimination of excess fluid in the body through urination .
- Inotropes. These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
2. Surgical interventions. These include coronary bypass surgery, heart valve repair or replacement, and heart transplant. It may also involve the insertion of medical devices such as implantable cardioverter-defibrillators , cardiac resynchronization therapy , and ventricular assist devices .
3. Lifestyle changes. A crucial part of the treatment plan for a patient with heart failure is to change several habits that are linked to the disease. These include smoking cessation, blood pressure control, diabetes management, dietary changes, stress management, exercise and increase in physical activity.
Imbalanced Nutrition: More Than Body Requirements
May be related to:poor dietary habits, lack of exercise, excessive eating compared to nutritional needs, eating in response to emotional cues or external stimuli, poor dietary habits, lack of knowledge about appropriate portion size and food preparation.
As evidenced by:increased BMI, undesirable eating patterns, and sedentary lifestyle.
Don’t Miss: Heart Rate Svt
Nursing Interventions For Excess Fluid Volume
| Interventions | Rationale |
| Inform the patient and his/her relatives regarding fluid restriction. Advice to take fluid as per order. | Taking a low amount of fluid reduces extracellular volume. In advanced heart failure, fluid restriction is done around 1 litre/day. |
| Instruct the patient to take diuretics as prescribed. | Diuretics facilitates the excretion of excess body fluids. The patient could not maintain normal life due to an increase in the frequency of urination. So compliance with medication becomes difficult. For that, taking diuretics after work, or later in the day can increase compliance. |
| Instruct the patient to avoid a sodium-containing diet or take a low sodium diet. | Sodium retains water in the body. Restriction of sodium reduces excess fluid volume. |
| Instruct the patient to discuss with the physician regarding all the medication he/she is taking. | The patient may have comorbidities for which he/she may have taken some drugs. These drugs may counteract each other. So its better to discuss the medication taken by the patient. |
| Instruct the patient to contact the physician about any symptoms like weight gain, leg swelling, or change in breathing sounds. | Early recognition of symptoms can prevent readmission of the patient in the hospital. The patient can consult a doctor or nurse through telephone. |
| For severe fluid volume, excess considers the patient for hemofiltration or ultrafiltration. | It is an invasive procedure that draws out excess fluid in a short period. |
Excess Fluid Volume Nursing Care Plan 3
Nursing Diagnosis: Fluid Volume Excess related to high sodium intake and chronic hypertension as evidenced by a serum sodium level of 149 mEQ/L and blood pressure of 180/98 mmHg
Desired Outcome: The patient will restore normal fluid balance through interventions to normalize sodium level and blood pressure.
| Nursing Interventions Fluid Volume Excess | Rationales |
| Start patient on a strict fluid balance chart. | A record of the patients fluid intake and output will help identify the main source of fluid excess. It will also help staff and the patient if the fluid output is enough in comparison to fluid intake. |
| Monitor vital signs. | The patients blood pressure and heart rate may indicate fluid volume. It will also help in the evaluation of progress from the treatment. |
| Monitor patients electrolyte levels, particularly the serum sodium levels. | Sodium is a major extracellular fluid electrolyte partly responsible for fluid balance. |
| Review intravenous fluid orders. | |
| Diuretics help in the excretion of excess fluid build-up. |
Don’t Miss: Hole In Heart Surgery Risks
Impaired Gas Exchange Related To Ventilation/perfusion Imbalance As Evidenced By Breath Sounds Crackling Sounds Coughing Up Mucus And/or Blood Use Of Accessory Muscles Dyspnea
Breathing problems may be a sign of heart failure. As the heart gets weaker, it cant pump blood well enough to support your lungs and other organs. The amount and quality of blood flowing through your lungs may be reduced or cut off entirely because the heart has lost its ability to pump blood effectively.
- Crackling sound : This happens when fluid builds up in the lungs and gets pushed out with each breath you take. The fluid in your lungs produces raspy sounds as it passes through them when you breathe out.
- Coughing up mucus: Mucus buildup in the throat causes coughing as it tries to clear itself out when you swallow or move around too much during sleep this is known as dyspnea .
Managing Acute Decompensated Heart Failure
Approximately 5 million Americans have heart failure and at least 550,000 more are newly diagnosed each year. HF is the most common Medicare diagnosis-related group. In 2006, direct costs associated with the condition reached nearly $30 billion.
Although HF incidence hasnt declined in the past 20 years, overall survival has improved. Better risk factor identification, early intervention, and appropriate long-term care management have contributed to improved survival.
Heart failure definedHF is a progressive syndrome diagnosed from both clinical findings and structural and functional cardiac changes. Most people with symptomatic HF have some degree of left ventricular dysfunction, as from hypertension, myocardial infarction, myocardial infection, or genetic abnormalities.
Left ventricular ejection fraction is the percentage of blood pumped by the left ventricle with each heart beat. The Heart Failure Society of America describes two broad types of HFone with reduced LVEF and one with preserved LVEF. Measured by echocardiography, ejection fraction normally is 55% or higher. Patients with an EF of 35% or lower may not have HF signs and symptoms right away and at times may compensate fairly well. In the past, the term congestive heart failure was used to denote EF below 35%.
Also assess for signs and symptoms of:
American Heart Association. Heart Disease and Stroke Statistics2008 Update. www.americaheart.org/presenter.jhtml?identifier=3054076. Accessed December 29, 2008.
You May Like: How Much Does Open Heart Surgery Cost With Medicare
Excess Fluid Volume Nursing Care Plans Diagnosis And Interventions
Fluid Volume Excess NCLEX Review and Nursing Care Plans
Fluid volume excess also known as hypervolemia, refers to the excessive accumulation of fluid in the extracellular fluid compartment.
It may occur due to a variety of factors. Excess fluid volume is mainly associated with sodium regulation. A normal fluid volume is important in the balanced functioning of cells and sodium helps make this happen.
Sodium is a major extracellular electrolyte. It maintains fluid balance through the concept of tonicity. The tonicity of a solution is related to whether the fluid will influence the cells or not.
A solution that does not change the volume of the cell is called isotonic. While a hypotonic solution causes cells to swell, a hypertonic solution on the other hand makes cells shrink.
Sodium moves around intracellularly and extracellularly to keep body fluids isotonic and not affect cells and their function.
Restricting sodium and fluid intake is one of the effective treatment options to regain normovolemia or balanced fluid volume in the body.
If left untreated, fluid volume excess can put a strain on the major organs in the body such as the heart, liver, and kidneys.
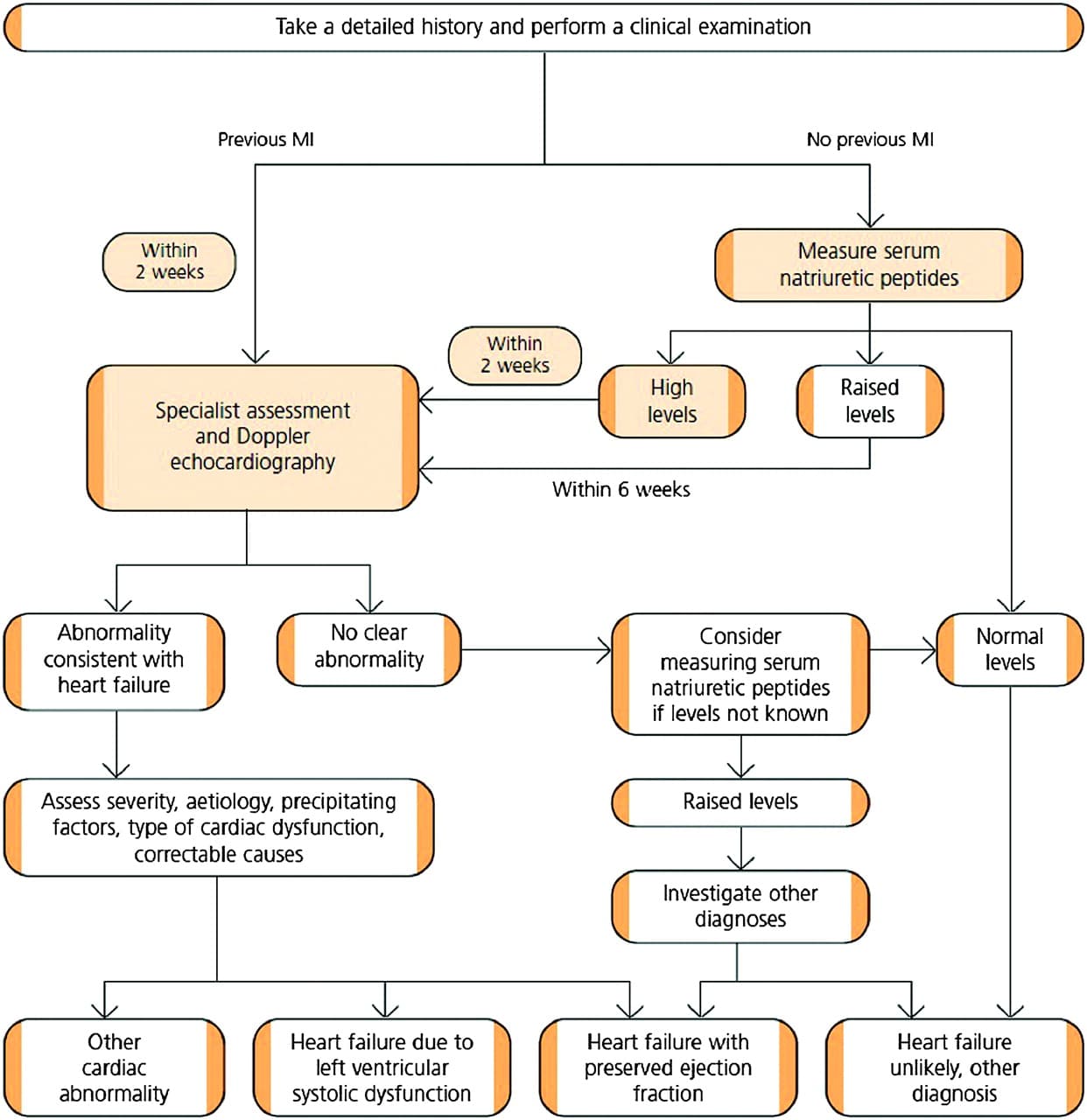
Diagnostic Tests For Heart Failure
Read Also: Can You Have High Blood Pressure And Low Heart Rate
Nursing Assessment For Deficient Knowledge
| Assessment | Rationale |
| Assess the patients knowledge regarding causes, treatment, and follow up care to heart failure. | This information provides data regarding knowledge of the patient about heart failure. It helps to plan educational sessions for the patient and family members. |
| Discuss with the patient and relatives about the disease and find out the existing misconceptions regarding treatment and care. | Finding out misconceptions and Clearing them out from the mind also guide future interventions. |
Excess Fluid Volume Nursing Care Plan 2
Chronic Kidney Disease
Nursing Diagnosis: Fluid Volume Excess related to renal insufficiency secondary to CKD as evidenced by bilateral leg edema, as well as a positive balance in the fluid balance chart.
Desired Outcome: The patient will understand measures to maintain normovolemia in the presence of CKD.
Recommended Reading: Can Antibiotics Cause Heart Palpitations
Ongoing Monitoring And Management
The ongoing monitoring of response to treatment and cardiopulmonary status also necessitates close monitoring of key haemodynamic parameters. In the immediate period of stabilisation, overly aggressive management with diuretics and vasodilators may lead to hypotension. Equally, patients may be undertreated or their underlying condition may deteriorate. Early warning scores allocate and weight points to vital signs outside pre-agreed ranges. These points are then summed to provide a single composite score. An increase in score will identify those patients who will benefit from escalation of monitoring or treatment. For example, they may benefit from an increased frequency of observationor ugent medical review. Escalation of treatment and alterations in management are then made in line with the score. To provide standardisation and limit misunderstanding the UK has adopted the National Early Warning Score for use in routine recording of clinical data, replacing traditional observation charts. Such tools have been reported to improve the ability of ward staff to identify and respond to indicators of clinical change.
Example Observation Chart Using Early Warning Scoring System
Recommended Reading: How Dangerous Is Open Heart Surgery
Nursing Diagnosis & Care Plan
Care Plan
Nursing Diagnosis: Activity Intolerance
Goal: Participate in a desired activity, meets the needs of self-tolerance achieving increased activity can be measured, evidenced by a decrease in fatigue and weakness and vital signs during exercise7.
Nursing Interventions:
Nursing Diagnosis: Excess Fluid Volume related to excess glomerular filtration rate
Goal: Balance fluid intake and output, clean breath sounds, vital signs within an acceptable range, stable weight, no oedema. Patient educated in maintaining proper fluid balance.
Nursing Interventions:
Recommended Reading: What Heart Surgery Is Most Dangerous
Excess Fluid Volume Nursing Care Plan 1
Nursing Diagnosis: Fluid Volume Excess related to compromised regulatory mechanism secondary to heart failure as evidenced by the presence of crackles and shortness of breath
Desired Outcome: The patient will regain a balanced fluid volume as evidenced by ease of breathing and clear lung sounds.
| Nursing Interventions Fluid Volume Excess | Rationales |
| Commence fluid balance chart. | Heart failure can compromise the fluid balance mechanism of the body. A record of the patients intake and output will help direct medical management by identifying how much fluid excess there is and where most of the fluid is coming from. |
| Assess the patients vital signs regularly. | The measurement of the patients vital signs will help evaluate the progress of management. It will also indicate if the patients breathing is improving. |
| Weigh the patient on a daily basis Use the same scale.Use the same clothing. | |
| Diuretics are effective in excreting excess fluid through the urine. | |
| Encourage the use of anti-embolic stockings. | Anti-embolic stockings prevent fluid accumulation in the extremities. |
| Refer to chest physiotherapy as needed. | Chest physiotherapists can help control fluid build-up in the lungs through breathing techniques. |
Chf Nursing Care Plan 7
Nursing Diagnosis: Ineffective Breathing Pattern related to pulmonary congestion secondary to CHF as evidenced by shortness of breath, SpO2 level of 85%, cough, respiratory rate of 25 bpm, and frothy sputum
Desired Outcome: The patient will achieve effective breathing pattern as evidenced by normal respiratory rate, oxygen saturation within target range, and verbalize ease of breathing.
| CHF Nursing Interventions | |
| Assess the patients vital signs and characteristics of respirations at least every 4 hours. | To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment. |
| Administer supplemental oxygen, as prescribed. Discontinue if SpO2 level is above the target range, or as ordered by the physician. | To increase the oxygen level and achieve an SpO2 value within the target range at least 96% |
| Administer the prescribed bronchodilators, steroids, or combination inhalers / nebulizers, as prescribed. | Bronchodilators: To dilate or relax the muscles on the airways. Steroids: To reduce the inflammation in the lungs. Inhalers or nebulizers To facilitate relaxation of the airway. |
| Elevate the head of the bed. Assist the patient to assume semi-Fowlers position. | Head elevation and semi-Fowlers position help improve the expansion of the lungs, enabling the patient to breathe more effectively. |
Don’t Miss: How Do Congestive Heart Failure Patients Die
