Find Alternative Thirst Quenchers
Its tempting to guzzle a bunch of water when youre thirsty. But sometimes, just moistening your mouth can do the trick.
The next time youre tempted to gulp down some water, try these alternatives.
- Swish water around your mouth and spit it out.
- Suck on sugar-free candy or chew sugar-free gum.
- Roll a small ice cube around the inside of your mouth.
Studies Evaluating Fluid Restriction In Patients With Hf
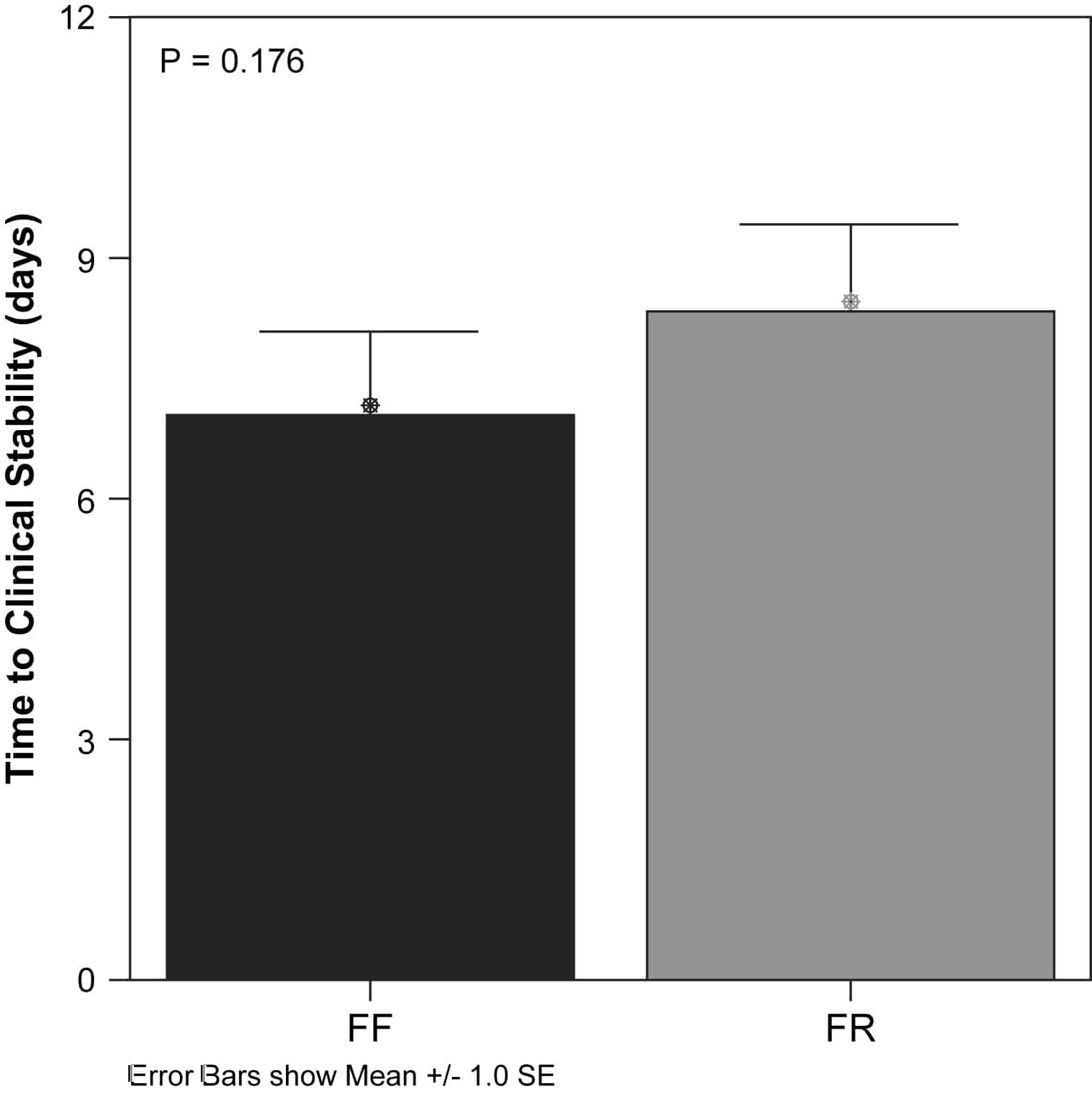
There is a limited number of randomised controlled trials evaluating the effects of fluid restriction in HF patients, most of which only include a small number of patients . One study included 410 patients. The challenge in interpreting these studies is that only two studies evaluated the effect of fluid restriction alone., In the other studies, fluid restriction was a component of an intervention, for example fluid restriction combined with sodium restriction, or in combination with sodium restriction and dietary recommendations.,, The other challenge is that the amount of fluid prescribed in the interventions varied between 800 and 2000 ml/day, and one study restricted fluid in patients to 30 ml/kg body weight/day .
Tips For Reducing Sodium Consumption
Your body is constantly trying to strike the perfect balance between electrolytes, including sodium, and water. When you consume a lot of sodium, your body hangs on to extra water to balance it. For most people, this just results in some bloating and mild discomfort.
However, people with CHF already have extra fluid in their bodies, which makes fluid retention a more serious health concern. Doctors generally recommend that people with CHF limit their sodium intake to about 2,000 milligrams per day. This is slightly less than 1 teaspoon of salt.
While this might seem like a hard amount to limit yourself to, there are several easy steps you can take to eliminate extra salt from your diet without sacrificing flavor.
Don’t Miss: Nursing Care Plan For Heart Failure
Fluid Restriction In Patients With Heart Failure
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| Verified October 2020 by Luis Eduardo Paim Rohde, Hospital de Clinicas de Porto Alegre. Recruitment status was: RecruitingFirst Posted : November 2, 2020Last Update Posted : November 2, 2020 |
| Heart Failure, SystolicHeart Failure With DecompensationPulmonary Congestion | Behavioral: Fluid restriction | Not Applicable |
Inclusion Criteria:
- Hospital admission for primary diagnosis of acutely decompensated heart failure, regardless of etiology, according to the criteria of the American College of Cardiology
- Diagnosis on echocardiography of heart failure with reduced ejection fraction
- Presence of pulmonary congestion defined as at least 2 pulmonary fields with more than 3 B lines in each field on pulmonary ultrasound at the time of hospital discharge.
Exclusion Criteria:
- Pulmonary fibrosis or other severe disease that changes the image acquisition
- Factors that could hinder follow-up
- Disability or refusing to understand and adhere to the protocol
- Refusal to sign consent form.
Experiment With Alternative Seasonings
Salt, which is about 40 percent sodium, might be one of the more common seasonings, but its definitely not the only one. Try swapping salt for savory herbs, such as:
Pepper and lemon juice also add a good amount of flavor without any added salt. For extra convenience, you can also purchase salt-free seasoning blends.
Read Also: Congestive Heart Failure Labs
Managing All Types Of Heart Failure
When managing pharmacological treatment, follow the recommendations in the NICE guidelines on medicines adherence and medicines optimisation.
Pharmacological treatment
Diuretics
1.6.1 Diuretics should be routinely used for the relief of congestive symptoms and fluid retention in people with heart failure, and titrated according to need following the initiation of subsequent heart failure therapies.
1.6.2 People who have heart failure with preserved ejection fraction should usually be offered a low to medium dose of loop diuretics . People whose heart failure does not respond to this treatment will need further specialist advice.
Calcium-channel blockers
1.6.3 Avoid verapamil, diltiazem and short-acting dihydropyridine agents in people who have heart failure with reduced ejection fraction.
Amiodarone
1.6.4 Make the decision to prescribe amiodarone in consultation with a specialist.
1.6.5 Review the need to continue the amiodarone prescription at the 6monthly clinical review.
1.6.6 Offer people taking amiodarone liver and thyroid function tests, and a review of side effects, as part of their routine 6monthly clinical review.
Anticoagulants
1.6.7 For people who have heart failure and atrial fibrillation, follow the recommendations on anticoagulation in the NICE guideline on atrial fibrillation. Be aware of the effects of impaired renal and liver function on anticoagulant therapies.
Vaccinations
See NICE’s guidance on smoking and tobacco and alcohol.
Air travel
Driving
Monitoring Treatment For All Types Of Heart Failure
Clinical review
1.7.1 All people with chronic heart failure need monitoring. This monitoring should include:
-
a clinical assessment of functional capacity, fluid status, cardiac rhythm , cognitive status and nutritional status
-
a review of medication, including need for changes and possible side effects
-
an assessment of renal function. Note: This is a minimum. People with comorbidities or co-prescribed medications will need further monitoring. Monitoring serum potassium is particularly important if a person is taking digoxin or an MRA.
1.7.2 More detailed monitoring will be needed if the person has significant comorbidity or if their condition has deteriorated since the previous review.
1.7.3 The frequency of monitoring should depend on the clinical status and stability of the person. The monitoring interval should be short if the clinical condition or medication has changed, but is needed at least 6-monthly for stable people with proven heart failure.
1.7.4 People with heart failure who wish to be involved in monitoring of their condition should be provided with sufficient education and support from their healthcare professional to do this, with clear guidelines as to what to do in the event of deterioration.
Measuring NT-proBNP
1.7.5 Consider measuring NT-proBNP as part of a treatment optimisation protocol only in a specialist care setting for people aged under 75 who have heart failure with reduced ejection fraction and an eGFR above 60 ml/min/1.73 m2.
Read Also: Energy Drinks And Heart Attacks
What If You Need Extra Calories And Nutrients
In severe heart failure, more calories are often needed because of the increased workload of the heart and lungs. But calorie requirements will vary, based on your current nutritional status.
If you are underweight or malnourished, you will need to increase your intake to obtain sufficient calories and protein to prevent the loss of muscle tissue, maintain or gain weight, and achieve a healthy level of protein in the blood.
In people whose activity is very limited , it is important to obtain sufficient calories and protein to prevent the development of pressure injuries . Increased food intake is often difficult for individuals who have moderate to severe heart failure because of the congestion, poor appetite, shortness of breath, and nausea that are often caused by this condition or by the medicines used to treat it.
The bodys increased energy demands along with the obstacles to sufficient intake can often lead to malnutrition in people who have heart failure. The following is a list of suggestions to help you boost your appetite and to help you increase your calories and protein with as little volume and discomfort as possible.
Tips for increasing your calorie and protein intake
Team Working In The Management Of Heart Failure
1.1.1 The core specialist heart failure multidisciplinary team should work in collaboration with the primary care team, and should include:
-
a lead physician with subspecialty training in heart failure who is responsible for making the clinical diagnosis
-
a specialist heart failure nurse
-
a healthcare professional with expertise in specialist prescribing for heart failure.
1.1.2 The specialist heart failure MDT should:
-
diagnose heart failure
-
give information to people newly diagnosed with heart failure
-
manage newly diagnosed, recently decompensated or advanced heart failure
-
optimise treatment
-
start new medicines that need specialist supervision
-
continue to manage heart failure after an interventional procedure such as implantation of a cardioverter defibrillator or cardiac resynchronisation device
-
manage heart failure that is not responding to treatment.
1.1.3 The specialist heart failure MDT should directly involve, or refer people to, other services, including rehabilitation, services for older people and palliative care services, as needed.
1.1.4 The primary care team should carry out the following for people with heart failure at all times, including periods when the person is also receiving specialist heart failure care from the MDT:
Care after an acute event
For recommendations on the diagnosis and management of acute heart failure, see the NICE guideline on acute heart failure.
Writing a care plan
additional sources of information for people with heart failure.
Recommended Reading: Prayers For Heart Surgery
Giving Information To People With Heart Failure
1.3.1 When giving information to people with heart failure, follow the recommendations in the NICE guideline on patient experience in adult NHS services.
1.3.2 Discuss the person’s prognosis in a sensitive, open and honest manner. Be frank about the uncertainty in predicting the course of their heart failure. Revisit this discussion as the person’s condition evolves.
1.3.3 Provide information whenever needed throughout the person’s care.
1.3.4 Consider training in advanced communication skills for all healthcare professionals working with people who have heart failure.
First consultations for people newly diagnosed with heart failure
1.3.5 The specialist heart failure MDT should offer people newly diagnosed with heart failure an extended first consultation, followed by a second consultation to take place within 2 weeks if possible. At each consultation:
-
discuss the person’s diagnosis and prognosis
-
explain heart failure terminology
-
address the risk of sudden death, including any misconceptions about that risk
-
encourage the person and their family or carers to ask any questions they have.
Drink The Right Amount Of Fluids
When your heart failure is not very bad, your health care provider may not place you on a fluid restriction. As your heart failure becomes worse, your health care provider may limit your fluids to 6-9 cups a day. Having other conditions like kidney disease may factor into their decision, too. If you are not sure how much you should drink per day, ask your health care provider.
Most of your hydration should come from water .
Other examples of fluids are:
- Sparkling water
Also Check: What Is A Normal Heart Rate For A Pregnant Woman
Don’t Miss: Which Side Of The Heart Has Oxygenated Blood
Treating Heart Failure With Reduced Ejection Fraction
When managing pharmacological treatment, follow the recommendations in the NICE guidelines on medicines adherence and medicines optimisation.
First-line treatment
1.4.1 Offer an angiotensin-converting enzyme inhibitor and a betablocker licensed for heart failure to people who have heart failure with reduced ejection fraction. Use clinical judgement when deciding which drug to start first.
ACE inhibitors
1.4.2 Do not offer ACE inhibitor therapy if there is a clinical suspicion of haemodynamically significant valve disease until the valve disease has been assessed by a specialist. See the section on referral for echocardiography and specialist assessment in the NICE guideline on heart valve disease.
1.4.3 Start ACE inhibitor therapy at a low dose and titrate upwards at short intervals until the target or maximum tolerated dose is reached.
1.4.4 Measure serum sodium and potassium, and assess renal function, before and 1 to 2 weeks after starting an ACE inhibitor, and after each dose increment.
1.4.6 Once the target or maximum tolerated dose of an ACE inhibitor is reached, monitor treatment monthly for 3 months and then at least every 6 months, and at any time the person becomes acutely unwell.
Alternative treatments if ACE inhibitors are not tolerated
1.4.7 Consider an ARB licensed for heart failure as an alternative to an ACE inhibitor for people who have heart failure with reduced ejection fraction and intolerable side effects with ACE inhibitors.
Beta-blockers
Ivabradine
Nutrition Guide For Heart Failure
Following a low-sodium diet and drinking less fluid can help you feel better and allow your heart failure medicines to work better. A low-sodium diet may even keep you out of the hospital. It is not an easy diet to follow. You may find eating with heart failure is a bit of a balancing act. While you dont want to eat too much of high sodium foods, you have to be sure to eat enough to maintain good nutrition.
Nutrition and Heart Failure
The recommended salt intake is 2,000 mg of sodium per day.
Salt is a mineral that is made of sodium and chloride. It is found in food, table salt and sea salt. Sodium acts like a sponge and makes the body hold water.
Eating too much sodium when you have heart failure can cause fluid buildup in your legs, stomach and lungs and force you heart to work harder.
Most of the sodium we eat is hidden in foods. Even food that does not taste salty can contain a lot of sodium.
You should restrict the amount of sodium you eat to 2,000 mg or less each day. Try to keep the sodium content of each meal to less than 600 mg. This helps spread out your sodium intake over the day to prevent excessive fluid retention.
You can take a few basic steps to reduce the amount of sodium in your diet:
- Dont add salt when you cook or at the table
- Learn to read food labels
- Choose more foods that are lower in sodium
- Limit high sodium foods
Reading a Food Label for Sodium
Follow these easy steps to read the label:
Low-Sodium Foods
Don’t Miss: How Does Music Affect Your Heart Rate
Study Design And Centers
This is a randomized, parallel trial with blinded outcome assessment. The study population will comprise patients with a diagnosis of HF-PEF who have presented to hospital with HF decompensation. The study will be carried out at Hospital de Clínicas de Porto Alegre , Brazil, and take place at the Emergency Department or other inpatient units.
Fluid Restriction In Heart Failure
If your heart has stopped beating, then there is no stopping fluid from coming back up. So you simply need to make sure that fluid doesnt get back into your lungs. Fortunately, fluid restriction therapy can help a lot in this regard. The fluid is the liquid which is kept in the lungs. The more fluid in the lungs, the more likely you are to get fluid in your lungs.
In my opinion, the best way to do this is to take a look at your diaphragm. This is a muscle on the front of your body that is responsible for breathing. It can be very hard to keep the diaphragm from moving. So a lot of folks are recommended to wear a lung mask to try and keep it from moving. This however, is a very uncomfortable method of controlling fluid.
In fact, it is a very painful method. Not only is it uncomfortable, but it is also a lot of stress to your lungs. In fact, it can lead to them becoming inflamed which is why I recommend the lung mask method in the first place.
Ive read that if you have heart failure your diaphragm may be very sensitive to any movement of the chest. To prevent this from happening, you can add a layer of fluid to your chest by inserting a tube of fluid into your chest. This tube of fluid can be made from any of a variety of materials that are easily available. For example, a medical grade silicone tube is a common choice.
Read Also: Energy Drinks And Heart Attacks
You May Like: Natural Ways To Reverse Congestive Heart Failure
Restricting Water Intake: Necessary Or Not
Dr Vega: That is great advice. It is important to think about water intake, too. Again, a common recommendation to patients is a fluid restriction to less than 2 L a day of free liquids. Again, we are not sure how effective that might be. A meta-analysis of randomized trials that examined liberal fluid intake versus a more restricted intake found no difference in terms of mortality or readmission. Is fluid restriction for everyone, or should you reserve it for certain patients? Patients can get very frustrated with fluid restriction.
Dr Piña: I do not restrict fluids at all. If patients follow the reasonable sodium diet you and I have just discussed, the water follows. A lot of the thirst has to do with the disease and the central mechanism of angiotensin II, which causes thirst, and patients think that they need more fluid. If you neurohormonally block that mechanism well, patients will not have that thirst. So I do not restrict fluid at all unless the patient is hyponatremic. That is when you get into trouble, and that is the hardest one to do. Patients who are not neurohormonally blocked, which is usually the reason behind the hyponatremia, are usually undermedicated. Once you medicate them, the thirst gets better. But until then, it is very hard to restrict fluids. These folks will drink from the faucet. They will drink from the bathroom. There is a huge drive to drink that fluid. Those patients need to be handled very carefully.
What About Supplements?
Tables
Importance Of The Study
It is possible that this study will show benefits of one treatment regimen over the other in some respects and neutral or opposite effects with regard to other variables. This may obviously make the interpretation of the study result difficult. We, however, feel that the most important variable is the quality of life and, accordingly, this is the primary efficacy variable. If one treatment regimen shows benefit over the other in terms of one or more of the secondary variables, but is less efficacious with regard to quality of life, the main conclusion must be based on the quality of life result. However, the effects on quality of life should be equal for the two regimens, secondary variables may have an important impact on the interpretation of the study result. Of course, the effects on hospitalisation are of importance. Thus, if one intervention is superior with regard to quality of life but inferior in terms of hospitalisation, this must affect the conclusion.
If no differences between the two regimens can be detected with regard to the quality of life, physical function or morbidity, can we then assume that the body adjusts to whatever fluid intake we have? We will probably not be able to answer that question. However, with such a study result the interpretation may be that the patients should be able to enjoy the benefits of a less strict fluid restriction, if any such benefits are shown.
Don’t Miss: How To Prevent A Heart Attack In 10 Seconds
