Avoiding Flu And Pneumonia With Vaccinations
Flu and pneumonia pose greater dangers for people who have heart failure than for healthy people.
Pneumonia is a lung infection that keeps your body from using oxygen as efficiently as it should. Your heart has to work harder to pump oxygenated blood through the body. If you have heart failure, you should avoid putting this extra stress on your heart.
Ask your doctor or another healthcare professional about getting a yearly influenza vaccine and a one-time pneumococcal vaccine.
Both vaccines are generally safe and seldom cause any severe reactions. Its much riskier not to be vaccinated against flu and pneumonia.You might have some pain or swelling at the site of the shot , but this will go away after a few days.
Read more about flu and pneumonia.
These 3 Types Can Make Heart Stronger
Isaac Gonzalez, 38, knows the power of exercise, along with eating well and sticking to medications. The California man lives with heart failure because of a problem he was born with. Gonzalez stretches and does pull-ups every morning before heading to work.
Stretching gets his blood moving and keeps him flexible for his job working with high-voltage electrical cables, so he protects himself from injury.
A good goal for most people is at least 30 minutes a day of activity on most days of the week, Steinbaum says.
Three types of exercise work together to make your heart and body stronger.
Flexibility. These workouts can improve balance, loosen your joints, and help with range of motion. Exercises like yoga use meditation, breathing exercises, and slow movements. This adds flexibility, improves breathing, and lessens stress.
The ancient Chinese practice of tai chi is often called meditation in motion. It uses slow dance-like movements that can lower blood pressure, ease stress, and give you more energy. One study of people with heart failure found that it improved their quality of life.
Cardio . Regular cardio exercise strengthens the heart muscle and gets your blood moving to improve circulation. Hereâs how to get started:
You might enjoy group fitness classes because they can help you to stick to a routine. But they donât allow much wiggle room, since theyâre usually âone size fits all.â They may not meet your individual needs for rest or water breaks, Ferri adds.
Association Between Changes In Physical Activity And Heart Failure Risk
Pandey et al.,14 evaluating Cooper Center Longitudinal Study and Centers for Medicare & Medicaid Services data, demonstrated that individuals who increased their fitness levels had a lower rate of HF hospitalization. Furthermore, longitudinal changes in cardiorespiratory fitness, but not body mass index, were found to be associated with HF risk.13 Moreover, in young adults evaluated in the CARDIA Study,17 the decline in cardiorespiratory fitness over followup was a significant predictor of subclinical systolic dysfunction and elevated diastolic filling pressure in middle age independent of baseline cardiorespiratory fitness levels. These data were confirmed in HFpEF: low cardiorespiratory fitness could be not only considered as an early stage marker but also a target for prevention, owing to the impact of exercise training on risk factor profile, on left ventricle structure and function, on myocardial strain pattern, and on vascular stiffness.19 It was calculated that 1 MET improvement in physical activity was associated with 17% reduction of HFpEF risk at a later age21 and that daily dynamic exercise for > 30 min four or five times weekly over the course of a lifetime preserves left ventricle diastolic function.22
Also Check: Aortic Aneurysm Open Heart Surgery
Can I Continue Working
If you’re well enough, you can keep working for as long as you feel able. With the right support, staying in work can make you feel better and give you financial security.
Talk to your employer as soon as you feel your heart failure is affecting your ability to do your job so you can find a solution that suits both of you. For example, it may be possible for you to work part-time.
The Disability Discrimination Act 1995 requires employers to make reasonable adjustments to working practices or premises to help a person with a disability.
Where possible, this might include changing or modifying tasks, altering work patterns, installing special equipment, allowing time off to attend appointments, or helping with travel to work.
Best Exercises For Congestive Heart Failure
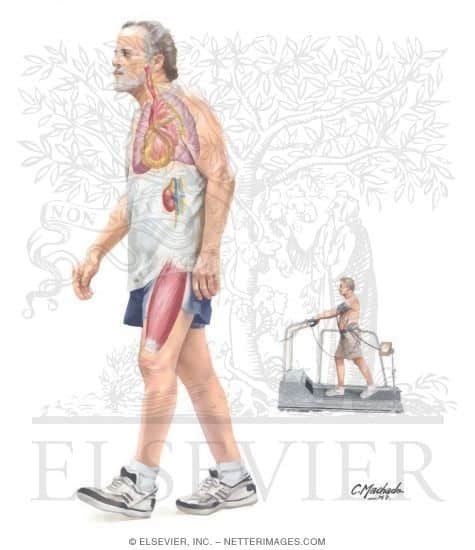
Heart failure refers to a situation where your heart functions abnormally and fails to pump the required blood necessary for the body. Due to lack of flow of blood and oxygen to several tissues and organs, performing different routine activities become difficult. However, with simple lifestyle changes, it is possible to turn the severe condition of heart failure into a success story.
Read Also: Does High Cholesterol Cause Heart Attacks
Your Heart Rate While Walking
Wearing a heart rate monitor can help ensure your heart rate doesn’t get higher than your healthcare provider recommends. If you have a fast or irregular heartbeat while exercising, rest and let your heart rate slow down. Check your pulse after 15 minutes. If it is higher than 120-150 beats per minute, stop exercising and call your healthcare provider.
Here are some additional walking tips:
- Start gradually: If youre out of shape, begin with short distances. Start with a comfortable pace and gradually increase your time or distance. Trying with several 10- to 20-minute walks a day instead of one long walk is one way to make it easier.
- Watch your form: Keep your head lifted, abs engaged and shoulders relaxed. Swing your arms naturally. Avoid carrying heavy items or hand weights because they can put extra stress on your elbows and shoulders. Try to walk naturally.
- Breathe: If you cant talk or catch your breath while walking, slow down. Speed isn’t so important in the beginning.
- Step up the pace: Walk at an easy pace for the first several minutes. Then gradually increase your speed.
- Change it up:Try brisk intervals. For example, walk fast for a few minutes then, slow for a few minutes and repeat several times. Over time youll be able to add more fast intervals with shorter recovery periods. If you are already active or have a higher level of fitness, you may be able to walk up hills or other inclines to increase the intensity.
What Will Happen Towards The End
Heart failure usually gets gradually worse over time. It may eventually reach a point where it becomes very severe and it’s unlikely the person will live much longer.
Palliative care will usually begin when heart failure reaches this stage.
This involves treatment to help you feel as comfortable as possible, as well as being offered psychological, spiritual and social support for both you and your family.
You can choose whether you want palliative care and where you’d like it to be provided.
Care can be provided:
Don’t Miss: Can Alcohol Cause Heart Palpitations
The Prediction Of The Future In Heart Failure Patients
Directly measured oxygen consumption is the objective and quantitative measure of cardiorespiratory fitness, and it represents cardiac, circulatory, and respiratory functions and muscle oxygen use. VO2 at peak exercise is a wellestablished prognostic factor in HF, but other exercise parameters are proved as powerful predictors of mortality such as ventilation /carbonic monoxide production slope, VO2 at anaerobic threshold, O2 uptake efficiency slope, VO2/work rate relationship, mean response time, and haemodynamic measurement during exercise. Recently, Alba et al.70 confirmed the role of peak VO2, O2 uptake efficiency slope, and VE/VCO2 as independent predictors with similar discriminatory capacity over recognized clinical variables. Again recently, Malhotra et al. in a stateoftheart paper71 and Keteyan et al.72 underlined the known role of CPET for careful measurement of ventilatory and O2 uptake patterns in HF to quantify disease severity, prognosis, and relative contributions of organ system to exercise intolerance.
Nonetheless, the prognostic power of CPETderived parameters is deeply supported by literature, but they were poorly considered for prognostic scores. Indeed, only HF survival score73 and HFACTION predictive risk score model74 included only peak VO2 and exercise duration at CPET among other clinical parameters, totally excluding ventilatory parameters.
Types And Amount Of Exercise
Talk with your doctor before starting an exercise program. Also check with your doctor if you want to add or change activities. You may need to do some testing first.
- Work towards 20-30 minutes of activity per day most days of the week
- You dont have to be active for 30 minutes straight
- Its okay to be active for three different 10-minute blocks throughout the day
You might be able to participate in a cardiac rehabilitation program. This is an exercise program especially for patients with heart problems. While you exercise, your blood pressure, heart rate, and other physical responses are watched closely. After the program, an exercise routine is provided to you.
Don’t Miss: What Are Signs Of Heart Failure
The Danger Of Inactivity
According to the American Heart Association journal Circulation, as many as 250,000 deaths per year in the United States can be attributed to a lack of regular exercise. Living a sedentary, or inactive, lifestyle has consistently been one of the top five risk factors for heart disease. Other risk factors include high blood pressure, high cholesterol, smoking, and obesity. Those with low levels of physical fitness also experience a higher rate of cardiovascular events, like heart attack and death.
According to research from the University of South Carolina, men who reported more than 23 hours a week of sedentary activity had a 64 percent greater risk of dying from heart disease than those who reported less than 11 hours. Inactivity also affects other risk factors for heart disease. For example, according to the University of Maryland Medical Center, sedentary people have a 35 percent greater risk of developing high blood pressure than physically active people do.
Tracking Your Daily Fluid Intake
If you have heart failure, its common for your body to retain fluid. So your healthcare team may recommend limiting your liquid intake.
Many people are prescribed diuretics to help them get rid of extra water and sodium to reduce their hearts workload.
Talk with your doctor about how much liquid to drink every day.
Recommended Reading: Normal Heart Rate When Working Out
Exercise And Your Heart
Getting regular exercise when you have heart disease is important.
Exercise can make your heart muscle stronger. It may also help you be more active without chest pain or other symptoms.
Exercise may help lower your blood pressure and cholesterol. If you have diabetes, it can help you control your blood sugar.
Regular exercise can help you lose weight. You will also feel better.
Exercise will also help keep your bones strong.
Always talk with your health care provider before starting an exercise program. You need to make sure the exercise you would like to do is safe for you. This is particularly important if:
- You recently had a heart attack.
- You have been having chest pain or pressure, or shortness of breath.
- You have diabetes.
- You recently had a heart procedure or heart surgery.
Monitoring Your Blood Pressure

Monitoring blood pressure at home, in addition to regular monitoring in a doctors office, can help control high blood pressure.
Chart your blood pressure readings over time. This can reveal trends and help to eliminate false readings.
Find out more about how healthy eating can lower your blood pressure with the DASH eating plan.
You May Like: Does Ibuprofen Help Prevent Heart Attacks
Regular Reviews And Monitoring
You’ll have regular contact with your GP or care team to monitor your condition at least every 6 months.
These appointments may involve:
- talking about your symptoms, such as whether they’re affecting your normal activities or are getting worse
- a discussion about your medication, including any side effects
- tests to monitor your health
It’s also a good opportunity to ask any questions you have or raise any other issues you’d like to discuss with your care team.
You may be asked to help monitor your condition between appointments.
For example, your care team may suggest weighing yourself regularly so any changes in your weight, which could be a sign of a problem, are picked up quickly.
Contact your GP or care team if your symptoms are getting worse or you develop new symptoms.
Your care team will advise you about when and where to seek advice if there’s a potential problem.
Treatment Options For Chf:
Drug therapy
Drug therapy is usually combined with exercise therapy in an attempt to delay the onset of symptoms. This also improves the quality of life and decreases the mortality rate significantly. A primary care physician or a cardiologist prescribes the drug based on the stage or severity of heart failure. Types and number of drugs a patient can be on also depend on physical symptoms, lifestyle and the tolerance level of a patient. Usually, the patients are on beta-blockers and or ACE inhibitors. These will help to reduce heart rate, reduce blood pressure and mainly reduce the afterload to the heart. The doctors may also prescribe diuretics to help reduce the edema.
As a physical therapist, you need to be aware of what kind of drug your patient is on and when they take it. The drugs change vitals and affect the clinical presentation while in the rehab gym.
Recommended Reading: Can You Live With Heart Failure
When To Terminate The Exercise Session
Exercise is a beneficial treatment tool for CHF but it needs to have the right response. A clinician needs to terminate the exercise session if they see the following signs:
- A decrease in heart rate with an increase in workload
- A decrease in systolic BP of more than 10 mm of Hg with an increase in workload
- Diastolic BP increase more than 20 mm of HG with an increase in workload
- SpO2 measurement is below 80% with supplemental oxygen
- Patient requests to terminate the session
Signs And Symptoms Of Congestive Heart Failure:
Cardinal symptomsof congestive heart failure are:
- Shortness of breath at rest or with activity
- fatigue/lethargy
- Swelling or edema mainly dependent edema
Clinical presentation is mainly associated with types of heart failure or heart dysfunction.
Diastolic heart failure presents with dyspnea, tachypnea, cough, wheezing, presence of abnormal heart sound S3, systolic murmur, hypoxemia, orthopnea, and peripheral edema .
Systolic heart failure clinically demonstrates fatigue, angina, activity intolerance, decreases mental status, decreased urination, cool, pale, diaphoresis, hypoxia, desaturation on SpO2, cyanosis, and dyspnea.
You May Like: Heart Attacks Young People
Measuring Vitals In A Patient With Heart Failure:
It is also very important to make sure your patients are safe while performing an exercise. Personally, I dont rely on the age-related measurement of maximum heart rate when it comes to clinically complicated patients like a patient with CHF. There are few ways to measure the intensity of heart rate and find a favorable range to be in. Heart rate can be measured by the Karvonen method. Maximum heart rate should be between 60 % to 80% in order to achieve favorable results with CHF.
You can also check the Borg scale of the perceived rate of exertion or modified RPE. This will help to know how severe the fatigue level is while performing exercises. Usually, with CHF, you want your patient to be at 3 to 5 out of 10 on modified RPE or 11 to 15 out of 20 on RPE to be safe. Again, your patient may not be able to get to that point just in the first session of exercise. I am trying to give some general guidelines for exercise with CHF.
It is a good idea to measure blood pressure as well as heart rate while exercising. You want to see a linear relationship with heart rate as well as with systolic blood pressure and exercise resistance level or overload. As I mentioned above, I like to know what kind of medications my patients take. As that has an effect on their heart rate and blood pressure.
What Are Heart Disease And Heart Failure
Heart disease, also known as cardiovascular disease, is any disease that involves the blood vessels in the heart, limbs, or brain. The term covers:
- High blood pressure.
The primary risk factors for developing heart disease include:
- High blood pressure .
- Disease of the coronary arteries .
- A history of prior heart attack .
- A family history of heart disease.
- Cigarette smoking.
- Age over 45 for men over 55 for women.
Heart failure is a syndrome that occurs when the heart fails to meet the needs of the body. This means the heart is not functioning as it should. It occurs when the heart is unable to fill with, or pump, blood effectively. As a result, the body does not get the blood and oxygen it needs.
Primary risk factors for developing heart failure include:
- Coronary artery disease due to a buildup of plaque in the arteries of the heart.
- Heart defects inherited or present at birth.
- High blood pressure.
- Obesity increased body mass index.
Also Check: What Is An Unsafe Heart Rate
Caring For Someone With Heart Failure
Looking after someone with heart failure can mean anything from helping with hospital or GP visits and collecting prescriptions, to full-time caring.
There are many ways you can support someone with heart failure.
Heart failure can be disabling and distressing, and many people with the condition find it a huge relief to share their concerns and fears with someone.
As a carer, if you can attend GP and hospital appointments with the person with heart failure, you can encourage them to ask the right questions while you note down the answers.
You could also provide the doctor with additional information or insights into the person’s condition, which can be helpful for planning the right treatment.
Another way you can help is by watching for warning signs that the person’s heart failure is getting worse or they’re not responding to treatment.
Contact the person’s doctor if you notice a new symptom or their current symptoms are getting worse.
Signs to look out for include:
- shortness of breath that isn’t related to usual exercise or activity
- increased swelling of the legs or ankles
- significant weight gain over a few days
- swelling or pain in their tummy
- trouble sleeping or waking up short of breath
- a dry, hacking cough
- increasing tiredness or feeling tired all the time
See the care and support guide for information about all aspects of caring for someone with a long-term condition.
