Heart Failure With Preserved Ejection Fraction
In HFpEF , LV filling is impaired, resulting in
-
Increased LV end-diastolic pressure at rest or during exertion
-
Usually, normal LV end-diastolic volume
Global contractility and hence ejection fraction remain normal .
However, in some patients, marked restriction to LV filling can cause inappropriately low LV end-diastolic volume and thus cause low CO and systemic symptoms. Elevated left atrial pressures can cause pulmonary hypertension and pulmonary congestion.
Diastolic dysfunction usually results from impaired ventricular relaxation , increased ventricular stiffness, valvular disease, or constrictive pericarditis. Acute myocardial ischemia is also a cause of diastolic dysfunction. Resistance to filling increases with age, reflecting both cardiomyocyte dysfunction and cardiomyocyte loss, and increased interstitial collagen deposition thus, diastolic dysfunction is particularly common among older adults. Diastolic dysfunction predominates in hypertrophic cardiomyopathy, other disorders with ventricular hypertrophy , and amyloid infiltration of the myocardium. LV filling and function may also be impaired if marked increases in RV pressure shift the interventricular septum to the left.
E What Diagnostic Tests Should Be Performed
Chest x-ray and EKG are essential in the evaluation of a patient with suspected heart failure. Beyond providing information supporting the diagnosis of heart failure, these diagnostic tests often provide an alternative diagnosis that implies heart failure may not be the key diagnosis.
Echocardiogram is also essential and will provide substantial information about the size, structure, and function of the heart. MRI, which provides detailed information on the myocardium, should be considered.
MRI can provide strong, noninvasive evidence of etiology in many cases, such as prior infarction, myocarditis, hypertrophic cardiomyopathy, left ventricular noncompaction, stress or Takotsubo cardiomyopathy, amyloidosis, sarcoidosis, or hemochromatosis, for example. Positron emission tomography can also be used to diagnose cardiac sarcoidosis.
Endomyocardial biopsy should be considered in highly select circumstances, such as suspicion of myocarditis. Biopsy also has a role in defining the subtype of amyloid cardiomyopathy ). Patients with a family history of cardiomyopathy should be offered the option of referral for genetic counseling and testing.
Students Who Viewed This Also Studied
Cardiac System Quiz 3 .docx
West Coast University
Oakland Community College NUR 2520
Cardiovascular Exam.docx
West Coast University NURS 317L
Cardiac System Quiz 3 .docx
test_prep
Hunter College, CUNY NURS 221
cardiac system.docx
University of South Alabama NU 301
NCLEX Challenge 5.docx
American Career College, Anaheim NURS MISC
unnamed .jpg
Clayton State University NURS 303
Chapter 72 PrepU .docx
Recommended Reading: Typical Resting Heart Rate For A Healthy Individual
Articles On Heart Failure Types & Stages
If you have systolic heart failure, the left ventricle of your heart, which pumps most of the blood, has become weak. This may happen because it’s gotten bigger. Since it’s larger, the ventricle can’t contract the way it should. Because of that, your heart doesn’t pump with enough force to push blood throughout your body.
Pulmonary Hypertension In Heart Failure With Preserved Or Reduced Ejection Fraction
Both systolic and diastolic dysfunction of the left ventricle can result in elevation in LVEDP, left atrial pressure, and pulmonary venous pressure, and can thus result in PH. The degree of PH in heart failure is thought to be proportional to the duration and intensity of exposure to PVH, which occurs independent of left ventricular ejection fraction ,67 but may also be related to other factors. In heart failure with reduced EF , the prevalence of PH varies depending on the study population and definition used. In one study performed in 377 consecutive patients with heart failure and EF less than 35%, the prevalence of a mPAP greater than 20 mm Hg was 62% and was highly correlated with PAWP.68 Diastolic dysfunction can also result in PH. Ventricular systolic and diastolic stiffness increases with age, particularly in females.69 Both diastolic dysfunction prevalence70 and PAPs71 increase with age. In HFpEF , PH is also quite common. In an Olmsted County community study of patients with HFpEF, the median estimated RVSP by echocardiography was 48 mm Hg and 83% of patients had an RVSP 35 mm Hg.72 Elevation in PAPs is associated with adverse prognosis in both HFpEF and HFrEF.68,72,73
Masaru Obokata, Barry A. Borlaug, in, 2021
Also Check: Afrin Heart Palpitations
E Common Pitfalls And Side
-
Wrong medication
-
Inadequate dose
-
ACEI/ARB generally increase creatinine about 20% or less and this modest change should not precipitate cessation
-
ICD too soon
-
Stopping neurohormonal therapy before considering decrement in diuretic dose
-
Use of non-steroidal anti-inflammatory drugs , which can precipitate decompensation
-
Not uptitrating beta blocker due to history of reactive airway disease or asymptomatic, mild bradycardia
-
Overly aggressive fluid restriction in the absence of hyponatremia
ACEI/ARB
Bisoprolol 2.5-20 mg/day
Carvedilol 25 mg b.i.d. or 80 mg daily of controlled release
Metoprolol succinate 200 mg daily
Aldosterone antagonists
Spironolactone 25 mg daily
Eplerenone 25-50 mg daily
Digoxin is sometimes used in patients with atrial fibrillation and heart failure with insufficient rate control. Typical dose is 62.5 to 250 mcg daily.
In Systolic Heart Failure The Left Ventricle Becomes Weak And Can’t Contract And Work The Way It Should
The right side of the heart cannot pump the used blood it received from the body efficiently so it can’t get the blood back to the lungs to get replenished. In general, a larger number. What’s the difference between diastolic and systolic heart failure? Acute decompensated heart failure is a term used a reduced stroke volume, as a result of a failure of systole, diastole or both. Diastolic heart failure is more common than systolic heart failure in elderly patients. Heart failure, also known as congestive heart failure, is recognized as a clinical syndrome characterized by signs and symptoms of fluid overload or of inadequate tissue heart failure is the inability of the heart to pump sufficient blood to meet the needs of the tissues for oxygen and nutrients. The disease results from the buildup of fatty deposits in your arteries, which. It is a condition where the heart does not pump well. The left ventricle can’t contract vigorously, indicating a pumping problem. Heart failure symptoms include fatigue, nausea, coughing, lightheadedness, and loss of appetite. This can occur for several reasons, as congestive heart failure is the predominant clinical presentation in multiple disease states. Systolic heart failure features diminished ability of the ventricles to contract during systole. That means your heart won’t pump forcefully enough.
Don’t Miss: How Much Can Marijuana Increase A Person’s Heart Rate
B What’s The Evidence For Specific Management And Treatment Recommendations
2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Developed in collaboration with the International Society for Heart and Lung Transplantation.
Iv Management With Co
-
Concurrent anemia: Treatment may improve heart failure symptoms.
-
Concurrent arrhythmias: Consider the role that uncontrolled arrhythmias may have on heart failure exacerbation. Improved control of atrial fibrillation or premature ventricular contractions may improve symptoms. Many antiarrhythmics are contraindicated in severe heart failure.
-
Concurrent cancer: Consider whether antineoplastics may be contributing to heart failure
-
Concurrent chronic kidney disease: Continue ACEI/ARB if possible, but if necessary to discontinue, replace with isosorbide/hydralazine combination. May contribute to anemia. Aldosterone antagonists have a substantially increased risk of hyperkalemia.
-
Concurrent diabetes: Avoid thiazolidinediones in all heart failure patients and metformin if there is significant renal dysfunction.
-
Concurrent gout: It is likely that diuretic dosing will need to be increased if a gout flareup is treated with steroids.
-
Concurrent liver disease: Liver congestion is common and may result in the need to alter dose of medications metabolized by the liver.
-
Concurrent osteoarthritis: Avoid nonsteroidal antiinflammatory drugs
-
Concurrent pulmonary disease: Does not typically contraindicate beta-blocker usage
-
Concurrent prostatic hypertrophy: Alpha blockers should be avoided, as they have been shown to increase mortality in heart failure patients.
-
Concurrent sleep apnea: Should be treated aggressively to minimize neurohormonal activation.
Recommended Reading: Can Lexapro Cause Heart Palpitations
Management: Acute Heart Failure
The approach to the management of acute decompensation is different from that to CHF. Acute pulmonary edema should be managed by:
- sitting the patient up
- giving diamorphine
- giving nitrates
- giving loop diuretics
Blood pressure is a key measurement and should be considered when deciding the rate of a nitrate infusion or whether to use -agonists. If the systolic blood pressure drops below 100 mm Hg, consideration should be given to replacing the nitrate infusion with one containing dobutamine . Although the effect of an IV diuretic can often be dramatic , nitrates are preferred because, in addition to decreasing preload, they also decrease peripheral resistance and do not reduce cardiac output.
It is also important to take the precipitating factor into account. If, for example, a patient is in atrial fibrillation, slowing the ventricular rate may be more effective than a combination of more general measures. Similarly, if a patient has suffered an MI then thrombolysis or intervention may be the key to their recovery.
B History Part : Prevalence
Approximately half of patients with heart failure have systolic failure and the other half have diastolic heart failure. Some have features of both types. Heart failure is perhaps more common in men and in those who identify as black racially.
Risk increases with age. Regardless, the most important risk factors for developing heart failure on a population basis are hypertension, myocardial infarction, and diabetes.
The majority of diastolic heart failure is a result of longstanding hypertension, and this phenotype of heart failure is more common in women. Infiltrative diseases, such as amyloidosis and hemochromatosis, also typically lead to diastolic heart failure, often with restrictive physiology.
Prior chest radiation is another potential cause of diastolic heart failure, and the incidence may increase as prolonged cancer survivorship increases. Once patients are hospitalized with diastolic heart failure, the prognosis is approximately the same as systolic heart failure.
Hypertension and diabetes also increase the risk of systolic heart failure through the increased risk of coronary artery disease and myocardial infarctions. Thus efforts to minimize coronary artery disease would be anticipated to have substantial impact on risk of developing heart failure.
Alcohol, cocaine, methamphetamines, anthracyclines, some antirheumatic medications and tyrosine kinase inhibitors are common toxic causes of heart failure, which are typically identified through patient history.
Recommended Reading: How Does Heart Disease Affect The Skeletal System
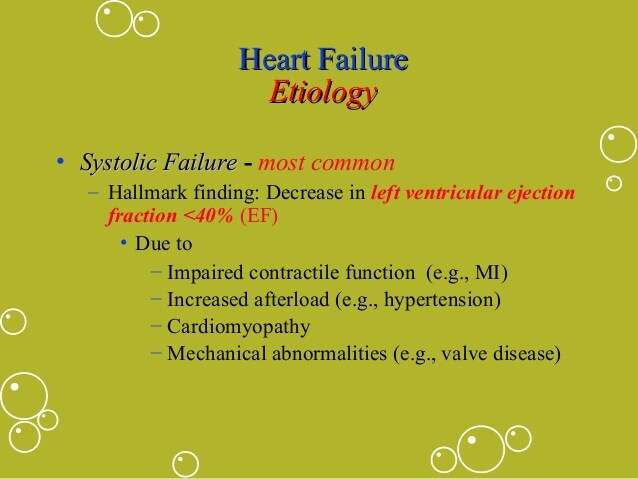
Heart Failure With Reduced Ejection Fraction
In HFrEF , global LV systolic dysfunction predominates. The LV contracts poorly and empties inadequately, leading to
-
Increased diastolic volume and pressure
Many defects in energy utilization, energy supply, electrophysiologic functions, and contractile element interaction occur, with abnormalities in intracellular calcium modulation and cAMP production.
Predominant systolic dysfunction is common in heat failure due to myocardial infarction, myocarditis, and dilated cardiomyopathy. Systolic dysfunction may affect primarily the LV or the right ventricle LV failure often leads to RV failure.
Pathophysiology Of Heart Failure
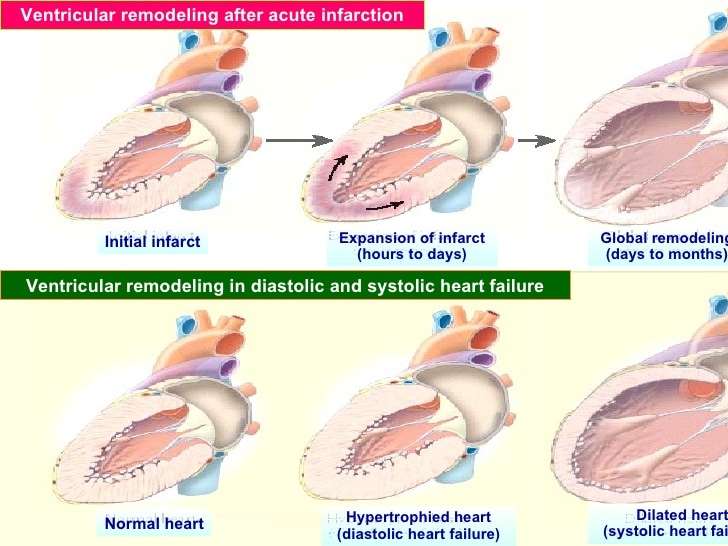
In heart failure, the heart may not provide tissues with adequate blood for metabolic needs, and cardiac-related elevation of pulmonary or systemic venous pressures may result in organ congestion. This condition can result from abnormalities of systolic or diastolic function or, commonly, both. Although a primary abnormality can be a change in cardiomyocyte function, there are also changes in collagen turnover of the extracellular matrix. Cardiac structural defects , rhythm abnormalities , and high metabolic demands also can cause HF.
Recommended Reading: What Heart Chamber Pushes Blood Through The Aortic Semilunar Valve
Precipitating Factors Of Ahf
The onset and increase in systemic congestion that precede AHF may develop over hours up to days, and can be triggered by several factors, either directly through stimulation of pathophysiological mechanisms leading to fluid accumulation or redistribution or indirectly through a worsening of cardiac diastolic or systolic function. The understanding of the pathophysiology involved in the development of AHF is important for providing the appropriate treatment. Although in many patients a progressive increase in body weight and pulmonary pressures may be observed as early as several days before hospital admission, in a relevant proportion of patients AHF is associated with only a minimal increase in body weight,. Several registries, including the North American OPTIMIZE-HF registry and the Euro-Asian registry of the GREAT network, have investigated the presence of precipitants in patients with AHF,. Acute coronary syndromes, arrhythmias , infections , uncontrolled hypertension and non-compliance with dietary recommendations and drug prescriptions are the most common identified precipitants,. Of note, in a relevant proportion of patients , no precipitants could be identified, whereas a combination of multiple factors were present in ~520% of patients,.
Challenges In The Interpretation Of Genetic Variants
The interpretation of potentially disease-causing rare variants is challenging owing to the relatively high frequency of rare benign variation in the population. This means that an individual variant might be rare but, collectively, variation in a specific gene is common. For example, healthy individuals appear to carry many unique variants that do not cause disease. There is, therefore, a need for robust population-matched control data to avoid spurious genedisease associations. The ExAC data-set of over 60,000 exomes will help to address the pressing need for greater amounts of control data . Several groups have shown how ExAC can be leveraged to aid the interpretation of rare variants in cardiomyopathies . These population data should be placed, however, in the context of other available resources to aid clinicians and researchers in interpreting rare variants, such as disease variant databases , computational data , functional data, and, crucially, segregation data. Conflict can arise between these sources, leading to a greater proportion of variants being categorized as of uncertain significance instead of likely pathogenic or pathogenic. We direct the reader to the recent American College of Medical Genetics and Genomics report that provides comprehensive guidelines on variant interpretation .
You May Like: How Much Can Marijuana Increase A Person’s Heart Rate
C Laboratory Tests To Monitor Response To And Adjustments In Management
Basic metabolic panels are typically performed shortly after initiation of therapy , to monitor renal function and ensure that diuretics are not causing dangerous perturbations in serum potassium levels. Following initiation of aldosterone antagonists, more frequent monitoring of potassium is indicated.
A commonly used strategy is 1 week after initiation or dose increase, and then again at 1 month. Once a stable medication regimen has been established, routine intermittent testing in heart failure patients is not typically performed. There is some data to suggest that BNP levels may be used to guide therapy.
What Is The Prognosis And Life Expectancy For Congestive Heart Failure
- The degree to which other organ systems are involved and the severity of other accompanying conditions
- The person’s symptoms and degree of impairment
- Other factors that remain poorly understood
With the availability of newer drugs to potentially favorably affect the progression of the disease, the prognosis in congestive heart failure is generally more favorable than that observed just 10 years ago. In some cases, especially when the heart muscle dysfunction has recently developed, a significant spontaneous improvement is not uncommonly observed, even to the point where heart function becomes normal.
Heart failure is often graded on a scale of I to IV based on the patient’s ability to function.
The prognosis of heart failure patients is very closely associated with the functional class.
An important issue in congestive heart failure is the risk of heart rhythm disturbances . Of those deaths that occur in individuals with congestive heart failure, approximately 50% are related to progressive heart failure. Importantly, the other half are thought to be related to serious arrhythmias.
Don’t Miss: How To Calculate Target Heart Rate Zone
Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Pregnancy
- Nutritional deficiencies
A History Part I: Pattern Recognition
Exertional dyspnea and fatigue are virtually universal. Volume overload is usually found, but in the modern era of powerful loop diuretics, some patients do not manifest fluid overload.
Nocturnal symptoms such as orthopnea and/or paroxysmal nocturnal dyspnea are also highly suggestive of heart failure. Abdominal discomfort or fullness is also a frequently reported symptom. Patients with well-compensated heart failure may have minimal symptoms and no evidence of volume overload. Characteristics of end-stage heart failure may include cachexia and Cheyne-Stokes respirations.
Recommended Reading: Does Benadryl Lower Heart Rate
D Physical Examination Findings
-
Evaluation of the central venous pressure is of the utmost importance.
-
Signs of volume overload
-
Extra heart sounds
-
Severe hypertension suggests diastolic heart failure
-
Profoundly low cardiac output states may be characterized by hypotension and/or narrow pulse pressure along with cool or mottled skin.
-
Sinus tachycardia is common but may be compensatory.
-
Respiratory distress
