Comorbidities: Anemia Iron Deficiency Kidney Failure Diabetes Frailty
Moderate anemia is often prevalent in patients with heart failure regardless of HFrEF or HFpEF . The incidence is higher in women, elderly and diabetic patients as well as in patients with renal failure. Increased blood loss in patients treated with oral anticoagulants , aspirin or both as well as decreased absorption of vitamin and/or iron may favor anemia. Similar as in other chronic illnesses iron deficiency is common in heart failure and may influence prognosis worse. Whether anemia and/or iron deficiency are markers of heart failure severity or whether they affect outcome of heart failure disease and thus should be treated is not entirely clear. In patients with heart failure with as well as without anemia intravenous ferric carboxymaltose has improved quality of life and NYHA class but not prognosis .
Heart failure and chronic kidney disease frequently coexist and share many risk factors also. CKD worsen prognosis in heart failure patients however, patients with severe CKD often have been excluded from randomized clinical trials and thus there is limited evidence-based therapy available.
Comorbidities and aging via influencing cognitive and self-care ability affect management of heart failure patients. Also, polypharmacy is present often. In addition, frailty is common in these patients. In consequence, a multidisciplinary team is needed to take care especially for older heart failure patients to reduce hospitalizations and improve outcome.
Additional Therapies For Heart Failure
Additional medical therapies that may be considered for patients with HFrEF groups include ivabradine, digoxin and hydralazine in combination with isosorbide dinitrate. Use of these agents is usually under direct supervision of HF specialists when other therapies are not tolerated or in patients who remain symptomatic despite maximum tolerated titration of other agents. It is outside the scope of this article, but device therapies, such as cardiac resynchronisation therapy, can make significant symptomatic improvement in a selected cohort with HFrEF and implantable cardioverter defibrillators can reduce sudden cardiac death in appropriately selected patients.
Left Ventricular Diastolic Function During Exercise
A detailed description of the mechanisms and clinical relevance of diastolic dysfunction during exercise is provided in Chapter 17 . The cardiac output can increase several fold during exercise, an appropriate response to the enhanced needs of exercising muscle. Multiple factors contribute to this response, including an increase in heart rate, a modest rise in stroke volume, a reduction in peripheral vascular resistance, and an elevation in contractile force, which increases LV, arterial systolic pressure, and the force of ejection.
The increase in LV output must be matched by a rise in LV input. The left ventricle cannot accomplish this task by the same mechanisms that increase output during exercise. For example, tachycardia shortens the duration of diastole, the time during which LV filling must occur. As a result, the diastolic filling rate during exercise may be increased out of proportion to cardiac output.
Several mechanisms contribute to the left ventricular diastolic suction effect during exercise:
Some of the mechanisms that allow an increase in cardiac output and in cardiac input during exercise act in concert on systolic and diastolic functions:
You May Like: Medicines For Heart Failure
Surgery And Percutaneous Procedures
Surgery may be appropriate when certain underlying disorders are present. Surgery in patients with advanced HF should be done in a specialized center.
Surgical closure of congenital or acquired intracardiac shunts can be curative.
If HF is primarily due to a valvular disorder Overview of Cardiac Valvular Disorders Any heart valve can become stenotic or insufficient , causing hemodynamic changes long before symptoms. Most often, valvular stenosis or insufficiency… read more , valve repair or replacement should be considered. Patients with primary mitral regurgitation are more likely to benefit than patients with mitral regurgitation secondary to LV dilation, in whom poor myocardial function is likely to continue postoperatively. Surgery is preferably done before myocardial dilation and damage become irreversible. More recently, percutaneous mitral valve repair procedure, in which a clip is applied to approximate the anterior and posterior mitral leaflets, has been shown to reduce death and HF hospitalization in carefully selected patients with symptomatic HF despite optimal medical management and moderate to severe or severe mitral regurgitation with preserved LV size is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal fluid… read more ).
An Understanding Of Pathophysiology Has Been Derived From Drug Studies
In the 1970s, it was believed that vasodilator drugs worked primarily by reducing high systemic vascular resistance and thus by âunloadingâ the failing left ventricle.69 Undoubtedly, the picture is far more complex than this. The chronic use of some powerful chronic vasodilator therapies, such as amlodipine,70 flosequinan, and epoprostenol,71 has had virtually no beneficial effect on survival or progression of heart failure. Epoprostenol actually worsened survival,71 as did
You May Like: What Caused Elvis Presley’s Heart Attack
How Can You Prevent Heart Failure
Some lifestyle measures can help treat heart failure and prevent the condition from developing. Maintaining a moderate weight and exercising regularly can significantly decrease your risk of heart failure. Reducing the amount of salt in your diet can also lower your risk.
Other habits that may prevent heart failure include:
- limiting alcohol intake
Genetic Contribution To Heart Failure
Genetic contribution to expression of heart failure is heterogenous and complex. Genomic variants and genetic predisposition influence the prevalence of risk factors and causes of heart failure like coronary heart disease or dilated or hypertrophic cardiomyopathy . As genetic testing is more available and cheaper it is also part of routine work up in special cases . More than 100 genes have been identified to be connected with the occurrence of cardiomyopathies . Due to the specific morphological and functional phenotypes, cardiomyopathies can be clinically divided in five different groups, i.e., dilated cardiomyopathy , HCM, restrictive cardiomyopathy , arrhythmogenic right ventricular cardiomyopathy , and non-classified cardiomyopathies as the left ventricular non-compaction cardiomyopathy . These forms may occur as familial or non-familial entity. Genetic profiles may influence risk and prognosis as well as therapeutic options of heart failure e.g., defibrillator implantation in high risk mutations for hypertrophy. Heart failure patients should also be asked for family history of the disease or the occurence of sudden death. In the current ESC-guidelines genetic testing is recommended when the prevalence of detectable mutations is sufficiently high and consistent to justify routine targeted genetic screening.
Also Check: What Factors Affect Heart Rate
Is There A Treatment For Heart Failure
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are to try to keep it from getting worse , to ease symptoms, and to improve quality of life.
Some common types of medicines used to treat it are:
- Aldosterone antagonists
- Selective sinus node inhibitors
- SGLT2 inhibitor
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. It usually includes workouts that are designed just for you, education, and tips to lower your chance of heart trouble, like quitting smoking or changing your diet.
Cardiac rehab also offers emotional support. You can meet people like you who can help you stay on track.
Anemia And Iron Deficiency
Anemia is common among patients with chronic heart failure and is frequently multifactorial. Anemia is associated with worse symptoms and outcomes in HF and so reversible causes should be sought and treated. Iron deficiency Iron Deficiency Anemia Iron deficiency is the most common cause of anemia and usually results from blood loss malabsorption, such as with celiac disease, is a much less common cause. Symptoms are usually nonspecific… read more is among the most common causes of anemia in HF, and iron replacement therapy should be considered once treatable causes such as blood loss have been excluded. Oral iron replacement is often less effective due to poor absorption and other reasons, thus intravenous iron replacement is preferred.
Recommended Reading: How Can I Lower My Heart Rate From Anxiety
Heart Failure With Preserved Ejection Fraction
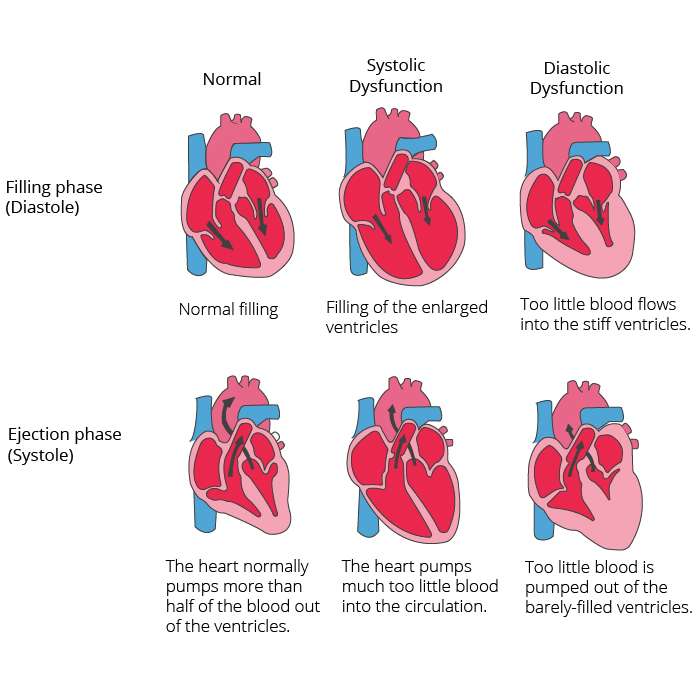
In diastolic heart failure , the same pathophysiologic processes occur that lead to decreased cardiac output in systolic heart failure, but they do so in response to a different set of hemodynamic and circulatory environmental factors that depress cardiac output.
In HFpEF, altered relaxation and increased stiffness of the ventricle occur in response to an increase in ventricular afterload . The impaired relaxation of the ventricle then leads to impaired diastolic filling of the left ventricle .
Morris et al found that right venticular subendocardial systolic dysfunction and diastolic dysfunction, as detected by echocardiographic strain rate imaging, are common in patients with HFpEF. This dysfunction is potentially associated with the same fibrotic processes that affect the subendocardial layer of the LV and, to a lesser extent, with RV pressure overload. It may play a role in the symptomatology of patients with HFpEF.
Chronic Heart Failure Part : Pathophysiology Signs And Symptoms
Rebecca Brake Advanced nurse practitioner in cardiology, Mid Cheshire NHS Foundation Trust, Cheshire, England
Ian David Jones Professor of cardiovascular nursing, School of Nursing and Allied Health, Liverpool John Moores University, Liverpool, England
Chronic heart failure is a common and complex clinical syndrome that results from impaired cardiac relaxation or contraction. Patients with chronic heart failure may experience multiple debilitating symptoms, such as fatigue, pain, and peripheral oedema. However, breathlessness may be considered the most debilitating symptom. This is the first of two articles on chronic heart failure, and outlines the pathophysiology of the condition, its causes, assessment, and signs and symptoms. Part 2 will discuss the treatment and management of the condition, including pharmacological strategies, device implantation, lifestyle modification, cardiac rehabilitation and palliative care.
Nursing Standard.31, 19, 54-63. doi: 10.7748/ns.2017.e10349
CorrespondencePeer review
This article has been subject to external double-blind peer review and checked for plagiarism using automated software
Conflict of interest
You May Like: High Blood Pressure And Heart Attack
Usmle Step 2 Style Questions Usmle
A previously healthy one-month-old infant is admitted to the hospital because of respiratory distress. He was born at term following an uncomplicated pregnancy and delivery. He had been well until 2 days ago when he developed fever and malaise. His is 162/min, respirations are 54/min, and is 64/48 mm Hg. Examination shows evidence of . A viral infection is suspected as the etiology of his acute heart failure. Which of the following is the most likely virus?
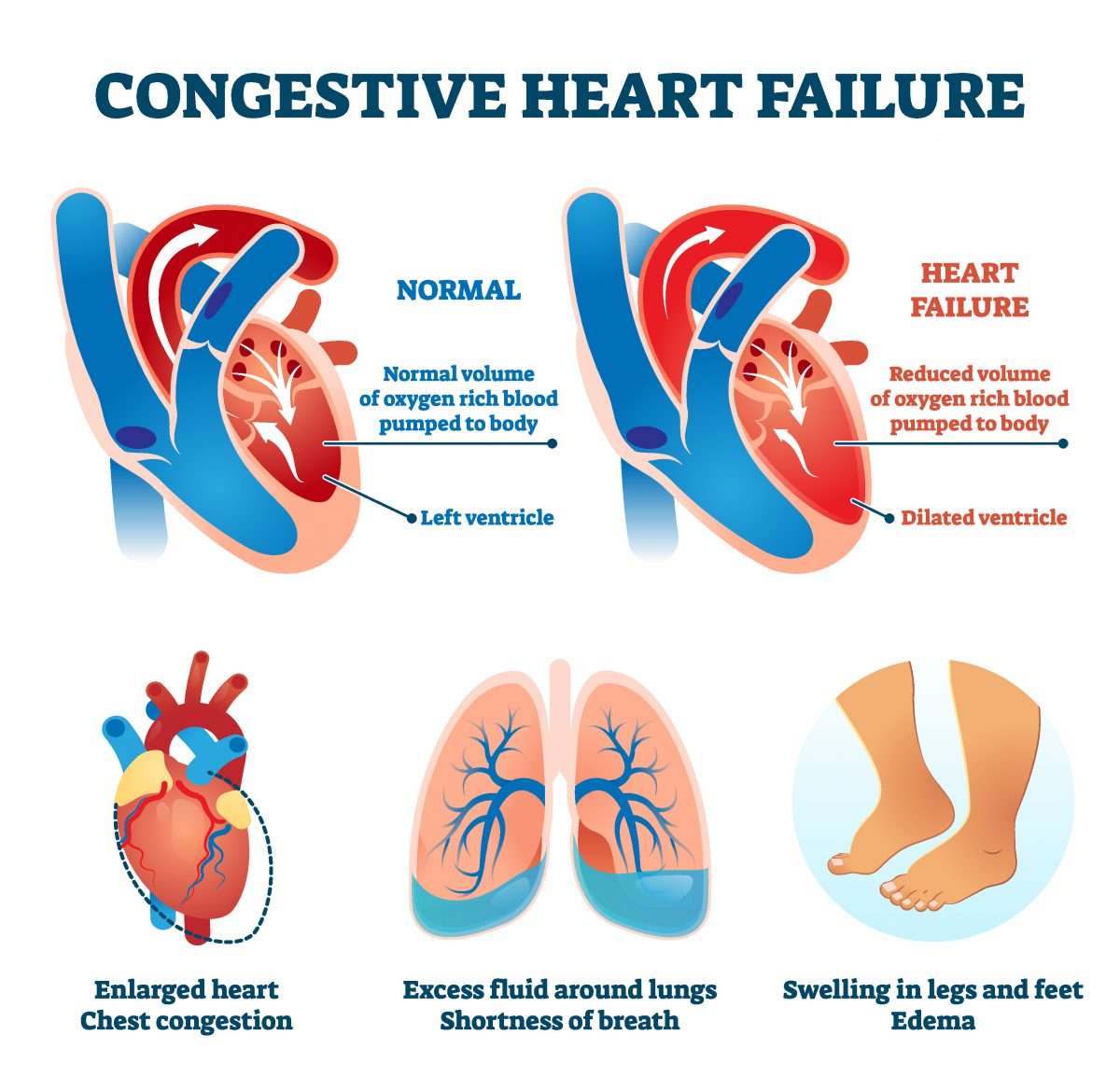
s used to describe a point at which the heart cant supply enough blood to meet the s demands.
This can happen in two ways, either the hearts ventricles cant pump blood hard enough during systole, called , or not enough blood fills into the ventricles during diastole, called .
In both cases, blood backs up into the lungs, causing congestion or fluid buildup, which is why its also often known as , or just CHF.
Congestive heart failure affects millions of people around the world and since it means that the s needs are not being met, it can ultimately lead to death.
Part of the reason why so many people are affected by heart failure, is that there are a wide variety of like and valvular disease that can impair the hearts ability to pump out blood andover timecan ultimately cause the heart to fail.
The heart rate is pretty intuitive, but the stroke volumes a little tricky.
So notice that not all the blood was pumped out right?
And the stroke volume is only a fraction of the total volume.
Overproduction Of Reactive Oxygen Species
Activated oxidative stress has been demonstrated in animal studies as well as in human studies to cause heart failure also lowered antioxidant activity in failing human hearts promotes oxidative stress . Furthermore, some risk factors for the development of heart failure also show increased oxidative stress i.e., hypertension, diabetes, obesity. Also in myocardial hypertrophy parameters of the redox-sensitive signaling pathways and transcription factors are activated . However, the complete mechanism is not understood yet . There are several factors activated via ROS which may influence contractility: proinflammatory mediators, periods of ischemia, auto-oxidation of catecholamines.
Don’t Miss: How Fatal Are Heart Attacks
What Causes Heart Failure
Heart failure is caused by many conditions that damage the heart muscle, including:
- Coronary artery disease.Coronary artery disease , a disease of the arteries that supply blood and oxygen to the heart, causes decreased blood flow to the heart muscle. If the arteries become blocked or severely narrowed, the heart becomes starved for oxygen and nutrients.
- Heart attack. A heart attack happens when a coronary artery becomes suddenly blocked, stopping the flow of blood to the heart muscle. A heart attack damages the heart muscle, resulting in a scarred area that doesnât work the way it should.
- Cardiomyopathy. Damage to the heart muscle from causes other than artery or blood flow problems, such as from infections or alcohol or drug abuse.
- Conditions that overwork the heart. Conditions including high blood pressure, valve disease, thyroid disease, kidney disease, diabetes, or heart defects present at birth can all cause heart failure. In addition, heart failure can happen when several diseases or conditions are present at once.
Asymptomatic Left Ventricular Dysfunction
It is now believed that many patients go through a period of asymptomatic LV dysfunction before the development of overt or symptomatic heart failure. Random echocardiographic screening of healthy populations of men and women aged 25 to 74 years suggests that approximately 1.5% of the general population has asymptomatic LV dysfunction,12 but this finding is very age dependent. Heart failure prevalence, as defined and diagnosed by clinical factors used by the Framingham investigators, is
You May Like: When Is Heart Rate Too High
What Are The Risk Factors For Heart Failure
Heart failure can happen to anyone. However, certain factors may increase your risk of developing this condition.
There is a higher incidence of heart failure in men compared with women, though the prevalence is about the same for all sexes.
People with diseases that damage the heart are also at an increased risk. These conditions include:
- ivabradine in some cases
- verquvo in some cases
Always speak with your doctor before taking new medications. Some medications are completely off-limits to people with heart failure, including naproxen and ibuprofen .
Pathophysiology Of Heart Failure
| Pathophysiology of heart failure | |
|---|---|
| A comparison of healthy heart with contracted muscle and a weakened heart with over-stretched muscle . | |
| Health | Harmful |
The main pathophysiology of heart failure is a reduction in the efficiency of the heart muscle, through damage or overloading. As such, it can be caused by a wide number of conditions, including myocardial infarction , hypertension and cardiac amyloidosis . Over time these increases in workload will produce changes to the heart itself:
The heart of a person with heart failure may have a reduced force of contraction due to overloading of the ventricle. In a healthy heart, increased filling of the ventricle results in increased contraction force and thus a rise in cardiac output. In heart failure, this mechanism fails, as the ventricle is loaded with blood to the point where heart muscle contraction becomes less efficient. This is due to reduced ability to cross-link actin and myosin filaments in over-stretched heart muscle.
The general effect is one of reduced cardiac output and increased strain on the heart. This increases the risk of cardiac arrest and reduces blood supply to the rest of the body. In chronic disease the reduced cardiac output causes a number of changes in the rest of the body, some of which are physiological compensations, some of which are part of the disease process:
You May Like: Congestive Heart Failure Alcohol
Can Surgery Be Used To Treat Heart Failure
In heart failure, surgery may sometimes prevent further damage to the heart and improve the heart’s function. Procedures used include:
- Coronary artery bypass grafting surgery. The most common surgery for heart failure caused by coronary artery disease is . Although surgery is more risky for people with heart failure, new strategies before, during, and after surgery have reduced the risks and improved outcomes.
- Heart valve surgery. Diseased heart valves can be treated both surgically and non-surgically .
- Implantable left ventricular assist device . The LVAD is known as the “bridge to transplantation” for patients who haven’t responded to other treatments and are hospitalized with severe systolic heart failure. This device helps your heart pump blood throughout your body. It allows you to be mobile, sometimes returning home to await a heart transplant. It may also be used as destination therapy for long-term support in patients who are not eligible for transplant.
- Heart transplant. A heart transplant is considered when heart failure is so severe that it doesn’t respond to all other therapies, but the person’s health is otherwise good.
How Can I Improve My Quality Of Life With Heart Failure
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Eat a healthy diet. Limit your consumption of sodium to less than 1,500 milligrams each day. Eat foods high in fiber. Limit foods high in trans fat, cholesterol, and sugar. Reduce total daily intake of calories to lose weight if necessary.
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also decrease heart failure progression.
- Don’t overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
You May Like: Do Arteries Carry Blood To The Heart
