What Tests Diagnose Pulmonary Hypertension
Your provider may use several different tests for different purposes.
These tests measure the blood pressure in your pulmonary arteries:
- Right heart catheterization: This test is also called pulmonary artery catheterization. It measures the pressure inside your pulmonary arteries and checks how much blood your heart can pump per minute.
- Doppler echocardiogram: A Doppler echo uses sound waves to show how your right ventricle is working. It also measures blood flow through your heart valves. It allows your provider to calculate your systolic pulmonary artery pressure.
These tests look for the underlying cause of pulmonary hypertension:
- Blood tests: Check for a range of issues related to organ function, hormone levels and infections. Specific blood tests include a complete metabolic panel and a complete blood count.
- Chest CT scan: Looks for blood clots and other lung conditions that may be causing your pulmonary hypertension or making it worse.
- Chest X-ray: Shows if your right ventricle or pulmonary arteries are bigger than they should be.
- Polysomnogram : This overnight sleep test checks if you have sleep apnea.
- Pulmonary ventilation/perfusion scan: Looks for blood clots in your lungs.
Your provider may also perform a six-minute walk test. This test shows how much exercise you can handle and how much oxygen is circulating in your blood as you exercise. The results indicate if your pulmonary hypertension is mild or severe.
Complications Of Congestive Heart Failure
- Rapid Weight Loss Severe heart failure can lead to a rapid loss of weight that can be life-threatening. Heart failure can cause blood to back up into the liver and intestines, causing these organs to swell. This swelling can lead to nausea and loss of appetite, and can prevent the body from absorbing nutrients from food.
- Impaired Kidney Function Congestive heart failure weakens the hearts ability to pump blood, reducing blood flow to the kidneys. This can lead to kidney damage or kidney failure, if left untreated.
- Liver Damage Heart failure can cause fluid to build up in the liver, which can lead to scarring. This makes it more difficult for the liver to carry out its day-to-day functions.
- Arrhythmias Heart failure results in damaged heart muscles, which can lead to the development of an arrhythmia, or abnormal heart beat. Arrhythmias can include the heart beating too quickly, beating too slowly, or beating irregularly.
- Heart Valve Problems If the heart is enlarged due to heart failure, the valves of the heart, which ensure appropriate direction of blood flow through the organ, may not function properly.
- Angina and Heart Attack Heart disease is a major contributing factor in many heart failure cases, and people with congestive heart failure are at continued risk of angina and heart attack.
What Makes Yale Medicines Approach To Treating Congestive Heart Failure Unique
Yale Medicines team comprises heart failure cardiologists and cardiac surgeons, dedicated advanced-practice, registered nurses and nurse coordinators, dietitians, exercise physiologists, financial counselors, immunologists specializing in transplants, psychologists, and specialists in palliative care.
With a multidisciplinary approach, Yale Medicine physicians include the patients desires as well as input from the family to develop a comprehensive treatment plan that’s right for them.
Recommended Reading: How Serious Is Congestive Heart Failure
Sleep Apnea And Heart Failure
People who have sleep apnea experience interruptions in breathing that can last 10 seconds or more and occur repeatedly throughout the night, as many as 30 times or more in the span of an hour.
This chronic disruption of the normal sleep cycle can leave individuals with the condition feeling exhausted and sleepy during the day, and it will put them at an increased risk of health problems associated with inadequate sleep, including irritability, problems with memory or concentration, anxiety, and depression.
Sleep apnea is commonly found in people with heart failure.
Our Favorite Apps And Gadgets
This app can help you to keep track of your liquid intake to avoid excess fluid buildup, which can lead to complications. You can also track your weight, since sudden increases in weight can be due to water retention. Another great thing about this app is that it alerts you if your blood pressure or weight gets high enough that you should tell your doctor. It also allows you to send reports on your fluid intake and weight to your healthcare provider.
This app, developed in partnership with the Heart Failure Society of America, is your one-stop shop for recording symptoms, vital signs, and medications to help you manage congestive heart failure. You can also track your information and keep a journal to maintain wellness and emotional health.
Read Also: Tavr Vs Open Heart Surgery
When Should I See My Healthcare Provider
Youll most likely have follow-up appointments with multiple healthcare providers as you recover from sudden cardiac arrest. Youll also have procedures or treatments that can help prevent you from having another sudden cardiac arrest.
Be sure to tell your provider if youre having any new symptoms or if you arent feeling better during the expected time frame.
When should I go to the ER?
If you witness someone collapsing into unconsciousness, call 911 to get help. Start CPR and send someone else to find an AED.
Can Surgery Be Used To Treat Heart Failure
In heart failure, surgery may sometimes prevent further damage to the heart and improve the heart’s function. Procedures used include:
- Coronary artery bypass grafting surgery. The most common surgery for heart failure caused by coronary artery disease is . Although surgery is more risky for people with heart failure, new strategies before, during, and after surgery have reduced the risks and improved outcomes.
- Heart valve surgery. Diseased heart valves can be treated both surgically and non-surgically .
- Implantable left ventricular assist device . The LVAD is known as the “bridge to transplantation” for patients who haven’t responded to other treatments and are hospitalized with severe systolic heart failure. This device helps your heart pump blood throughout your body. It allows you to be mobile, sometimes returning home to await a heart transplant. It may also be used as destination therapy for long-term support in patients who are not eligible for transplant.
- Heart transplant. A heart transplant is considered when heart failure is so severe that it doesn’t respond to all other therapies, but the person’s health is otherwise good.
Read Also: Does Acetylcholine Increase Heart Rate
What Happens In Congestive Heart Failure
The heart has two upper chambers and two lower chambers . Normally, blood:
But in heart failure, the heart cant work as it should and not enough blood and oxygen get to the organs. And blood backs up in the heart and then into the lungs.
What Causes Heart Failure
Heart failure can start suddenly after a medical condition or injury damages your heart muscle. But in most cases, heart failure develops slowly from long-term medical conditions.
Conditions that can cause heart failure include:
Also Check: What Is A Resting Heart Rate
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
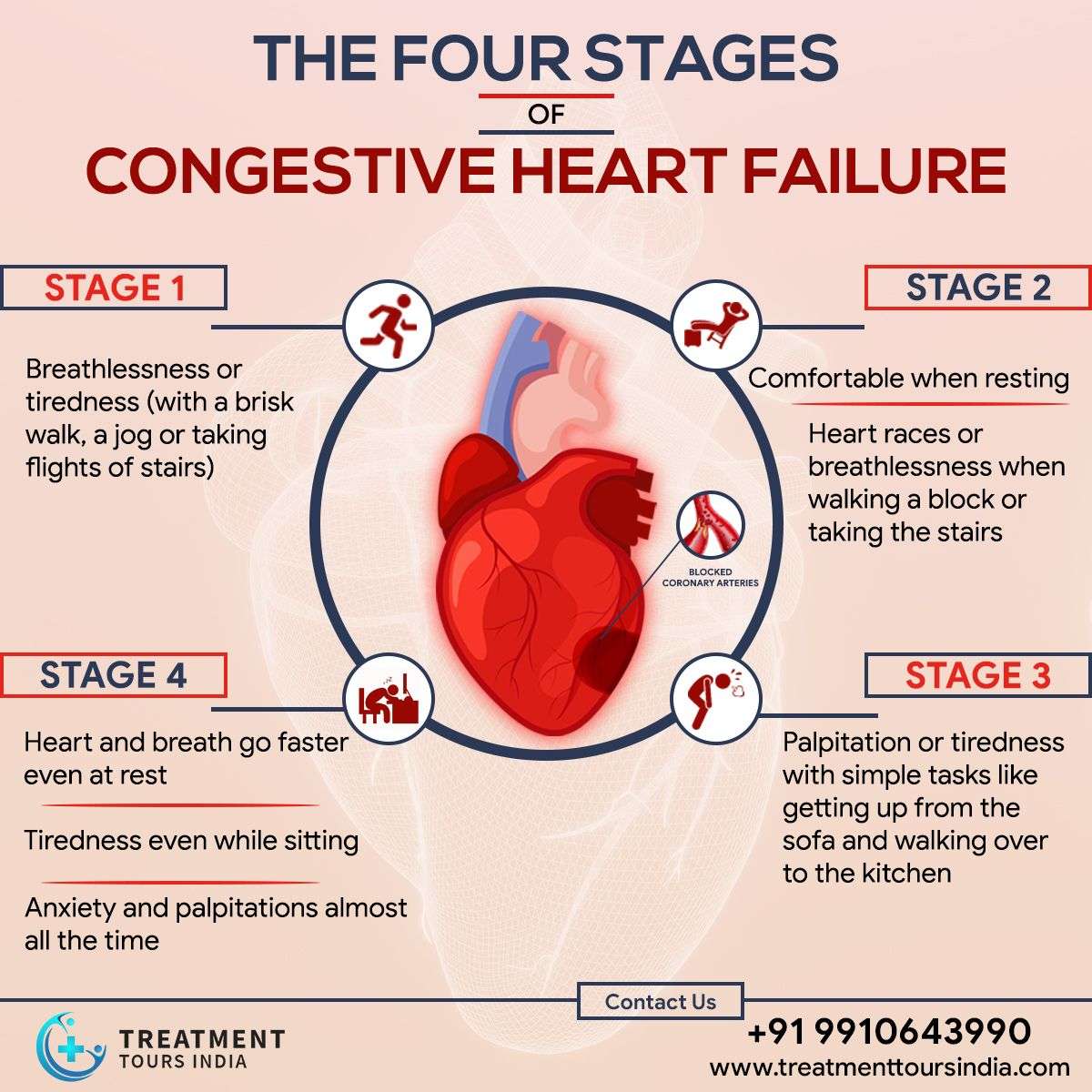
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Heart Failuresigns And Symptoms
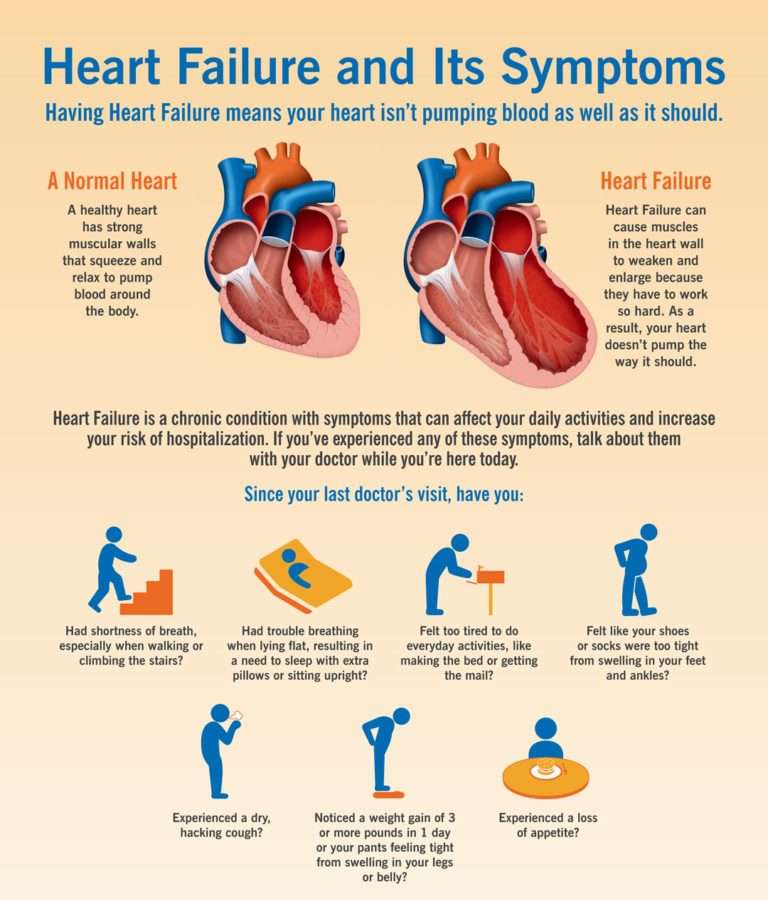
Heart failure is a condition in which the heart fails to function properly. The terms “heart failure” and “congestive heart failure ” don’t mean that the heart has actually “failed” or stopped but mean one or more chambers of the heart “fail” to keep up with the volume of blood flowing through them.
Heart failure is brought on by a variety of underlying diseases and health problems.
Your condition may involve the left side, the right side or both sides of the heart. Each side has two chambers:
- An atrium or upper chamber
- A ventricle or lower chamber
Any one of these four chambers may not be able to keep up with the volume of blood flowing through it.
Two types of heart dysfunction can lead to heart failure, including:
- Systolic Heart Failure This is the most common cause of heart failure and occurs when the heart is weak and enlarged. The muscle of the left ventricle loses some of its ability to contract or shorten. In turn, it may not have the muscle power to pump the amount of oxygenated and nutrient-filled blood the body needs.
- Diastolic Failure The muscle becomes stiff and loses some of its ability to relax. As a result, the affected chamber has trouble filling with blood during the rest period that occurs between each heartbeat. Often the walls of the heart thicken, and the size of the left chamber may be normal or reduced.
Read Also: How To Control Heart Rate
What Dietary Changes Should I Make
Your provider will give you specific recommendations. One key step involves reducing your sodium intake. This means:
- Avoid adding salt at the table or using seasoning salt.
- Avoid smoked, cured, salted and canned meat products.
- Buy foods that are low sodium or low salt.
- Limit fast foods and prepared foods.
Other dietary changes include:
- Eat foods high in fiber .
- Eat foods high in potassium .
- Eat foods high in magnesium .
- Limit foods that contain refined sugar, saturated fat and cholesterol.
Is There A Treatment For Heart Failure
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are to try to keep it from getting worse , to ease symptoms, and to improve quality of life.
Some common types of medicines used to treat it are:
- Aldosterone antagonists
- Selective sinus node inhibitors
- SGLT2 inhibitor
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. It usually includes workouts that are designed just for you, education, and tips to lower your chance of heart trouble, like quitting smoking or changing your diet.
Cardiac rehab also offers emotional support. You can meet people like you who can help you stay on track.
Don’t Miss: How To Check For Heart Attack
What Are The Symptoms Of Heart Failure
The symptoms of heart failure depend on which side of your heart is affected and how serious your condition has become. Most symptoms are caused by reduced blood flow to your organs and fluid buildup in your body.
Fluid buildup happens because the flow of blood through your heart is too slow. As a result, blood backs up in the vessels that return the blood to your heart. Fluid may leak from the blood vessels and collect in the tissues of your body, causing swelling and other problems.
Symptoms of heart failure may include:
- Feeling short of breath when you do things like climbing stairs. This may be one of the first symptoms you notice.
- Fatigue or weakness even after rest.
What Are The Stages Of Pulmonary Hypertension
There are four main stages of pulmonary hypertension. The World Health Organization calls these functional classes. Theyre based on the symptoms you feel and refer to how well you can carry out your daily activities. As PH gets worse, the symptoms become more noticeable and more disruptive to your daily life.
- Class 1: You dont have any symptoms.
- Class 2: You dont have symptoms when youre resting. But you feel some discomfort or shortness of breath during some routine activities. These include household chores and climbing stairs.
- Class 3: You may still feel fine when youre resting. But its now much harder to do normal tasks because you feel tired or short of breath.
- Class 4: You have symptoms even when youre resting. The symptoms get worse when you try to do any normal task.
Recommended Reading: Lowering Heart Rate Breathing
How Can I Reduce My Risk
You can reduce your risk in many ways, such as:
- Keeping your regular follow-up appointments with your healthcare provider.
- Making healthy lifestyle changes such as losing weight and eating a low-fat diet.
- Avoiding smoking and other tobacco products.
- Taking medications your healthcare provider prescribes for high cholesterol or arrhythmia.
- Getting an implantable cardioverter defibrillator if your healthcare provider recommends it.
- Having procedures or surgery your healthcare provider recommends, such as angioplasty or catheter ablation.
- Taking genetic testing if recommended by your physician to look for potential causes of sudden cardiac death.
- Teaching your family the importance of immediate care and learning CPR.
High school and college athletes should have a heart screening every two years. This should include an evaluation of their personal and family history and a physical exam. Their sports physician may recommend additional testing such as an electrocardiogram if there are any concerning findings on an initial evaluation.
If your healthcare provider suspects a heart problem, you should get a referral to a cardiologist.
Meet Kim Ketter And Shaun Rivers Aha Heart Failure Ambassadors
ER nurse Kim Ketter had been feeling exhausted and short of breath for months, but it wasnt until one day when she suffered heart palpitations at work that she decided to see a doctor about her symptoms. Her diagnosis of cardiomyopathy and HF came as a surprise. When she learned her condition may be genetic, Kim knew that her twin sister and fellow nurse, Shaun Rivers, could also be at risk for HF, so she suggested Shaun see her doctor and get tested as well. The results from Shauns stress test indicated that she also had HF.
As ambassadors, Kim and Shaun are sharing their story to provide hope and support for people affected by HF.
Read Also: Can Hormones Cause Heart Palpitations
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
When Someone You Love Has Heart Failure
As her fathers health declined, Sue Macdonald and her family found caring for him became a full-time job.
Sue Macdonald likes to remember the good days with her father, Greg. Shed rather not think about the last few years of his life, before he died at age 76 from heart failure and related complications.
Greg had type 1 diabetes plus an accumulation of other health problems, including a form of dementia that might have been triggered by mini-strokes. He underwent heart valve surgery in his 60s as well as a triple bypass, then required several more operations when infection set in. Like many people with heart disease, he was eventually diagnosed with heart failure.
The family Sue, her mother and sister were drained from the effort of looking after him at home, even with regular visits from a personal support worker.
It was a full-time job taking care of my dad, dealing with the sheer number of appointments and trying to coordinate care, Sue says. Plus he was increasingly unhappy. When you know things are not getting better, it can be hard to stay positive.
Gregs family doctor was doing his best, Sue says. But there were lots of specialists involved. And specialists are very focused on their own areas whether its endocrinology or cardiology. It was a different system for each.
Families under stress
It is scary when it is something happening to someone who had been strong and there for you.
- Learn more about heart failure
Also Check: Why Is My Resting Heart Rate Increasing
