Risk Factors To Atrial Fibrillation
Risk factors associated with atrial fibrillation are as follows:
- Age. The risk of atrial fibrillation increase as the patient gets older.
- Heart disease. Patients with heart issues, such as congenital heart disease, congestive heart failure, coronary artery disease, history of heart attack, surgeries on the heart, and heart valve issues, increases the risk for atrial fibrillation.
- Hypertension. Hypertension, especially uncontrolled hypertension not managed with lifestyle modifications or medications, increases the risk for the condition.
- Thyroid disease. Thyroid problems may trigger arrhythmias in some people, including the development of atrial fibrillation.
- Other chronic health conditions. Conditions such as diabetes, metabolic syndrome, long-term kidney disease, lung issues, and apnea predispose a patient in developing atrial fibrillation.
- Alcohol use. Alcohol consumption may trigger episodes of atrial fibrillation in some people. Uncontrolled alcohol consumption further increases the risk.
- Obesity. Patients who are overweight have greater risks for atrial fibrillation.
- Familial history. Atrial fibrillation in the family may be passed down from generation to generation.
Chf Nursing Care Plan 4
Nursing Diagnosis: Activity intolerance related to imbalance between oxygen supply and demand as evidenced by fatigue, overwhelming lack of energy, verbalization of tiredness, generalized weakness, and shortness of breath upon exertion
Desired Outcome: The patient will demonstration active participation in necessary and desired activities and demonstrate increase in activity levels.
| CHF Nursing Interventions | Rationales |
| Assess the patients activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. | To create a baseline of activity levels and mental status related to fatigue and activity intolerance. |
| Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Alternate periods of physical activity with rest and sleep. | To gradually increase the patients tolerance to physical activity. |
| Teach deep breathing exercises and relaxation techniques. Provide adequate ventilation in the room. | To allow the patient to relax while at rest and to facilitate effective stress management. To allow enough oxygenation in the room. |
| Refer the patient to physiotherapy / occupational therapy team as required. | To provide a more specialized care for the patient in terms of helping him/her build confidence in increasing daily physical activity. |
Imbalanced Nutrition: More Than Body Requirements
May be related to:poor dietary habits, lack of exercise, excessive eating compared to nutritional needs, eating in response to emotional cues or external stimuli, poor dietary habits, lack of knowledge about appropriate portion size and food preparation.
As evidenced by:increased BMI, undesirable eating patterns, and sedentary lifestyle.
Dont Miss: Heart Rate Svt
Don’t Miss: Increased Resting Heart Rate
Nursing Care Plan Diagnosis Interventions For Anxiety Nervousness Inability To Cope And Ineffective Individual Coping
This free nursing care plan is for the following conditions: Anxiety, Nervousness, Inability to Cope, and Ineffective Individual Coping What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing care plan? This care plan is listed to give an
Congestive Heart Failure: Nursing Diagnosis & Care Plan
The nursing intervention plan is to be started from the patients education within the scope of CHF. The daily intake of fluid should be appropriate and include all liquids consumed per day, including tea, juice, soup, fruits, and vegetables. When dry mouth and thirst appear, one needs to rinse mouth, add lemon or a piece of ice to the water, take a small sip of water. The intake of table salt is limited, the daily rate of sodium chloride is a teaspoon, and it should not be forgotten that salt is added to food, so one does not have to add salt to ready-made meals and does not eat salty foods . Refusal to use all types of alcoholic beverages and smoking cessation are recommended.
Control of body weight is prescribed daily in the morning on an empty stomach in the same clothes as self-control diary. Among the indicators for home, self-control is also blood pressure measurement two times a day in the morning and evening and pulse control. These indicators must be recorded in the patients diary which can be monitored by a nurse in order to show them to the attending physician at the next visit . The optimal types of exercise for patients are walking, swimming, cycling. It is easier to start physical training with activities that do not require the support of their own weight. For a nurse, there is also a necessity to assess vital signs at least every 4 hours.
Read Also: Which Arm Is Heart Attack Sign
How To Conduct Electrocardiogram To Diagnose Heart Failure
Step 1: The patient will lie down or sit down if theyre too weak to stand.
Step 2: The doctor will place electrodes on the patients chest to check for electrical activity in the heart. These electrodes are placed over each of the hearts four chambers, and one electrode is also placed on their back .
Step 3: The doctor will apply a small amount of gel to each electrode and also put the back electrode in place.
Step 4: The doctor will turn on the EKG machine and read its printout for irregularities that may indicate heart failure. Depending on what is found, they may refer you to a specialist who can do further tests.
Signs And Symptoms Of Atrial Fibrillation
Clinical manifestations of atrial fibrillation comprise of the following:
- Presence of palpitations, characterized by fast and pounding heartbeat
Atrial fibrillation can be classified under these subtypes:
- Occasional Also known as paroxysmal atrial fibrillation, this subtype have symptoms that comes and goes, with durations of a few minutes to hours. In this subtype, manifestations may occur for as long as a week they may occur repeatedly and may alleviate without treatment. However, occasional A-fib would still need therapeutic management.
- Persistent This subtype is characterized as atrial fibrillation with tenacious manifestations that do not revert to normal heart rhythm. Because of this, and its associated life-threatening effects, persistent atrial fibrillation would need cardioversion or other medical therapies in order to reinstate and sustain normal heart rhythm.
- Long-standing persistent Another subtype wherein the patient experiences consistent atrial fibrillation that lasts more than 12 months.
- Permanent In this subtype, the condition is persistent and therefore would need medications to regulate the heart rate and therefore, address the irregular heart rhythm.
Also Check: Arm Pain And Heart Attack
Chf Nursing Care Plan 5
Nursing Diagnosis: Excess Fluid Volume related to decreased cardiac output and increased glomerular filtration rate as evidenced by S3 heart sound, blood pressure level of 190/85, orthopnea, pitting edema of the ankles, and weight gain
Desired Outcome: The patient will demonstrate a balanced input and output, and stabilized fluid volume
| CHF Nursing Interventions | Rationales |
| Assess vital signs and auscultate lungs to find any crackles or wheezes. | Heart failure, especially left-sided HF may lead to pulmonary congestion, as evidenced by crackles or wheezes upon auscultation of the lungs. |
| Commence a fluid balance chart, monitoring the input and output of the patient. | To monitor patients fluid volume accurately and effectiveness of actions to monitor the progress of excess fluid volume. |
| Restrict fluid intake as instructed by the physician. | To reduce fluid volume and manage edema. |
| Weigh the patient on a daily basis. | Diuretics are needed to manage heart failure, but may put the patient at risk for sudden fluid loss, which is reflected through his/her weight. |
| Monitor patients serum electrolytes and renal function to the physician as needed. | The use of diuretics may result to excessive fluid shifts and electrolyte loss. |
Nursing Care Plan For Ineffective Breathing Pattern: Diagnosis And Interventions Dyspnea Respiratory Distress Syndrome Hyoxia Acute Respiratory Failure Hypoxemia And Respiratory Illness
Ineffective breathing pattern care plan: This nursing care plan and diagnosis is for the following condition: Ineffective Breathing Pattern, Dyspnea, Respiratory Distress Syndrome, Hypoxia, Acute Respiratory Failure, Hypoxemia, and Respiratory Illness What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop
You May Like: Can Tens Unit Cause Heart Attack
Risk For Diminished Cardiac Output Related To Decreased Ability Of The Heart Muscle To Contract
For example, the heart may not be able to contract forcefully enough to pump blood through the body. This is known as congestive heart failure. The lungs may also be affected by the condition, causing shortness of breath and fatigue.
Heart failure can occur in people of all ages, though it is most common in adults over 55 years old or those who have had a previous heart attack. People with diabetes are also at increased risk for developing this condition because diabetes affects the way their bodies use sugar and other nutrients that help keep the heart healthy.
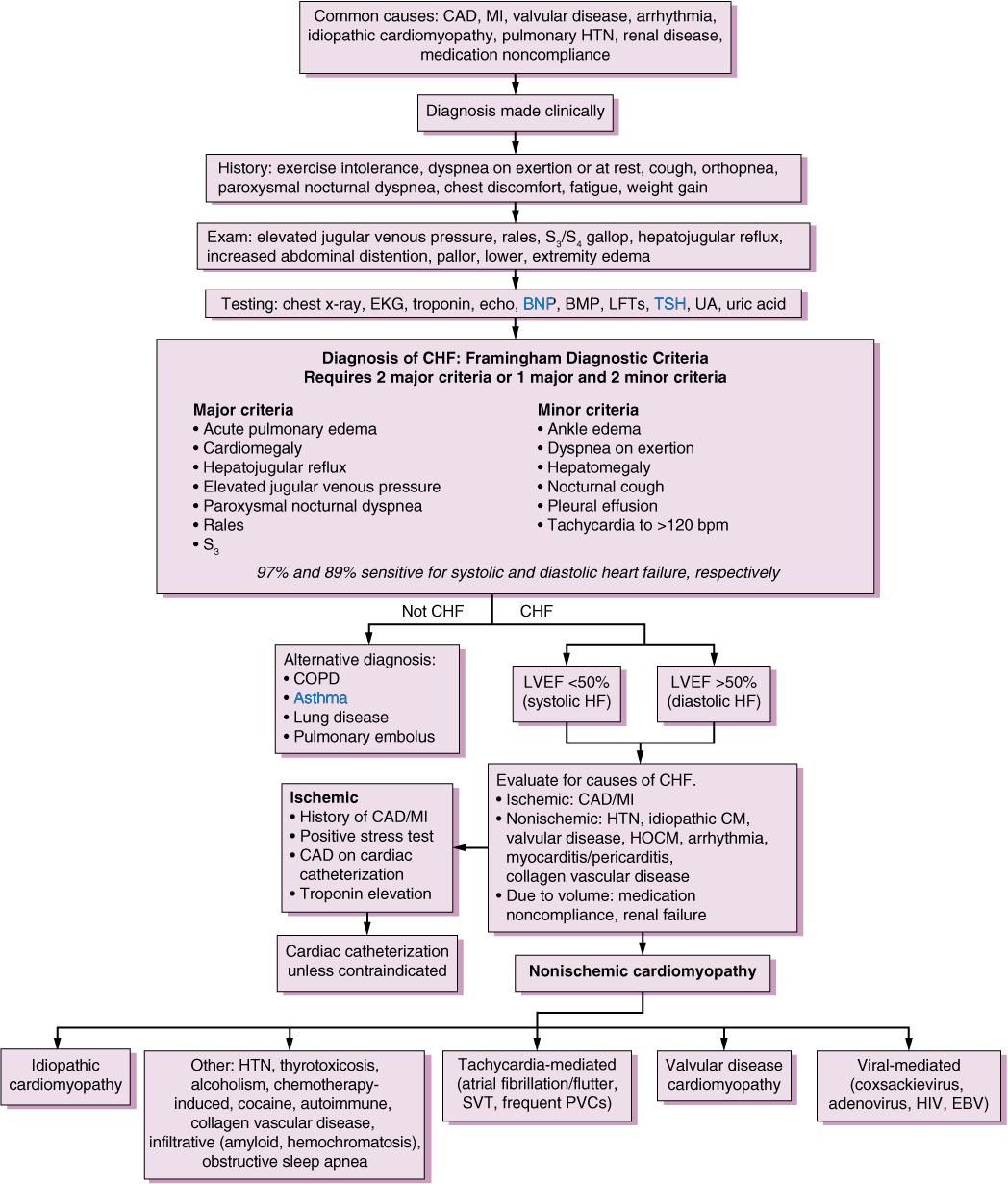
Congestive Heart Failure Chf Nursing Care Plans Diagnosis And Interventions
Congestive Heart Failure CHF NCLEX Review and Nursing Care Plans
CHF can affect either both sides of the heart or just one side. The three types of CHF are biventricular, left-sided, and right-sided heart failure. In left-sided heart failure, the left ventricle becomes enlarged and becomes dilated together with the left atrium in order to compensate for the increased pressure.
Right-sided heart failure usually happens after left-sided heart failure. Pooling of blood in the left heart chambers causes an increase in pressure, impairing the normal blood drainage from the lungs to the left atrium. The pressure in the pulmonary veins increases, causing the right ventricle to compensate by pumping more vigorously.
In time, the cardiac muscles of the right chambers wear down, causing right-sided heart failure. Failure of both sides of the heart is called biventricular heart failure.
Congestion is one of the common features of heart failure, thus the term congestive heart failure is still used by many medical professionals.
Read Also: High Heart Rate While Sleeping
Nursing Care Plan Diagnosis Interventions For Disturbed Body Image Residual Limb Amputation And Amputee
This free nursing care plan diagnosis, and interventions for the following conditions: Disturbed Body Image, Residual Limb, Amputation, and Amputee What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing care plan? This care plan is listed to give an example
Study Population And Sample
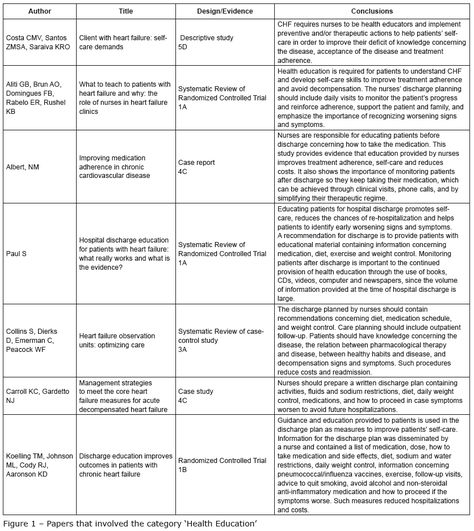
The population consisted of hospitalized patients with heart failure over a period of 12 months , considering a simple random sampling selection and overall margin of error resulting in a maximum of n = 5%. Total sample size corrected by the size of the N population was calculated using the following formula: n=/1+1111 Callegari-Jacques SSM. BioestatÃstica: princÃpios e aplicações Porto Alegre: Artmed 2003.. The sample selected for this study respecting the inclusion and exclusion criteria included 70 patients. Therefore, the estimated ratios in this study are subject to maximum error of 8.75% and a 95% confidence level.
The sample selection was non-probabilistic with an initial composition of 84 patients, but with four losses due to hospital discharge before the end of data collection, six losses due to death and two losses due to discontinuity by transfers. The final sample consisted of 72 patients followed for three weeks of hospitalization from the time of hospital admission.
Also Check: How Do You Calculate Maximum Heart Rate
Don’t Miss: How To Recognize A Heart Attack
Chf Nursing Care Plan 3
Nursing Diagnosis: Deficient Knowledge related to new diagnosis of Congestive Heart Failure as evidenced by patients verbalization of I want to know more about my new diagnosis and care
Desired Outcome: At the end of the health teaching session, the patient will be able to demonstrate sufficient knowledge of congestive heart failure and its management.
Nursing Care Plan Diagnosis Interventions Risk For Aspiration Impaired Swallowing Ineffective Swallowing Difficulty Swallowing Dysphagia Peg Tube Feeding And Difficulty Chewing
This nursing care plan and diagnosis with nursing interventions is for the following condition: Risk For Aspiration, Impaired Swallowing, Ineffective Swallowing, Difficulty Swallowing, Dysphagia, Peg Tube Feeding, and Difficulty Chewing. What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing
Don’t Miss: What Takes Blood Away From The Heart
Nursing Interventions For Excess Fluid Volume
| Interventions | Rationale |
| Inform the patient and his/her relatives regarding fluid restriction. Advice to take fluid as per order. | Taking a low amount of fluid reduces extracellular volume. In advanced heart failure, fluid restriction is done around 1 litre/day. |
| Instruct the patient to take diuretics as prescribed. | Diuretics facilitates the excretion of excess body fluids. The patient could not maintain normal life due to an increase in the frequency of urination. So compliance with medication becomes difficult. For that, taking diuretics after work, or later in the day can increase compliance. |
| Instruct the patient to avoid a sodium-containing diet or take a low sodium diet. | Sodium retains water in the body. Restriction of sodium reduces excess fluid volume. |
| Instruct the patient to discuss with the physician regarding all the medication he/she is taking. | The patient may have comorbidities for which he/she may have taken some drugs. These drugs may counteract each other. So its better to discuss the medication taken by the patient. |
| Instruct the patient to contact the physician about any symptoms like weight gain, leg swelling, or change in breathing sounds. | Early recognition of symptoms can prevent readmission of the patient in the hospital. The patient can consult a doctor or nurse through telephone. |
| For severe fluid volume, excess considers the patient for hemofiltration or ultrafiltration. | It is an invasive procedure that draws out excess fluid in a short period. |
Heart Failure Nursing Diagnosis
Several nursing diagnoses could be used when caring for patients with heart failure. Some of the more common ones include
Anxiety occurs because those who suffer from heart failure may have symptoms such as shortness of breath, fatigue, and palpitations, resulting in constant worry about their health. Excessive anxiety may lead to depression and may affect the ability of the individual to carry out daily activities.
Diarrhea because heart failure commonly causes hypoproteinemia, a deficiency of protein in the blood, it can cause an inability to control bowel movements or trouble with defecation. This may prove to be embarrassing for the patient and have a negative impact on their well-being.
like congestive heart failure , restrictive cardiomyopathy is caused by decreased cardiac output due to impaired ventricular function, resulting in insufficient blood flow through the body. Because of this, heart failure patients may develop clinical signs such as peripheral edema and shortness of breath.
Chronic Pain heart failure can be associated with chronic pain due to the stress on the body from the reduced cardiac output and fluid overload .
Activity intolerance those who suffer from heart failure are often limited in the amount of physical activity they can participate in, which may severely impact their quality of life.
Fluid Overload heart failure is commonly related to fluid overload, which can be dangerous and lead to complications such as pulmonary edema.
Recommended Reading: What Is Your Resting Heart Rate Supposed To Be
Diagnostic Evaluation Of Heart Failure Patients
- Change in level of consciousness
- S3 AND S4 Gallop sounds
Assessment for decreased cardiac output
Nursing interventions for decreased cardiac output
| Interventions | Rationale |
| Administer medication and assess patients home compliance with prescribed medication. | Heart failure patients require taking several types of medications. It includes angiotensin-converting enzyme inhibitors , beta-blockers, diuretics, aldosterone antagonists, digoxin and vasodilators. |
| Administer oxygen if needed or if the patient does not maintain the appropriate saturation level. | In case of heart failure or accumulation of fluid in the lungs, oxygen supply could not meet the demand of the body. Therefore supplemental oxygen is needed. |
| If there is an increase in preload, restrict fluid and sodium intake as ordered. | This restriction decreases extracellular fluid volume in the body and reduces the cardiac load. |
Nursing Care Plan For Hypertension
These nanda nursing care plans include a diagnosis, and many nursing interventions for the following conditions: Hypertension What are nursing care plans ? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing care plan? This care plan is listed to give an example of how a
Read Also: Does Vitamin B12 Increase Heart Rate
Ineffective Breathing Pattern Related To A Decreased Respiratory Rate
Respiratory rate is the number of breaths a person takes in one minute. Its measured by counting how many times your patient breathes in one minute, and you can do this with a watch or by counting out loud. A normal respiratory rate is 12-20 breaths per minute . In patients with CHF, respiratory rate may be decreased due to difficulty breathing through the narrowed airways caused by edema or other interstitial lung disease. To monitor this condition, check your patients respiratory status every shiftespecially if they have symptoms such as shortness of breath or fatigueand keep track of what changes when you note an increase/decrease in their respiratory status over time
Nursing Intervention Of Heart Failure Patients In Emergency Department
- Elicit Cardiac History and Physical Assessment
- Auscultation of all four cardiac sounds for rate, rhythm, and quality. . Then auscultate for murmur grade 1 to 6 .
- Palpation for LV hypertrophy by feeling the sternum and observing for sharp, deep systolic murmur in apex beat.
- Check pulse oximetry heard 100% on room air .
- Teaching: It is important to teach the heart failure patient and family members/ loved ones about the disorder, its prognosis, and the cause of disease projections in addition to reassurance for available treatment modalities. It is also important to teach them about medications and their activities and the signs of toxicity, as this will lead to more effective medication management.
Read Also: What Causes Heart Rate To Spike
