Key Steps In The Diagnosis Of Chronic Heart Failure
The diagnosis of CHF requires the presence of symptoms and/or signs of HF and objective evidence of cardiac dysfunction . Typical symptoms include breathlessness, fatigue, and ankle swelling . Symptoms and signs lack sufficient accuracy to be used alone to make the diagnosis of HF.
The diagnosis of CHF is made more likely in patients with a history of MI, arterial hypertension, CAD, diabetes mellitus, alcohol misuse, chronic kidney disease , cardiotoxic chemotherapy, and in those with a family history of CMP or sudden death.
The following diagnostic tests are recommended for the assessment of patients with suspected chronic HF:
Electrocardiogram . A normal ECG makes the diagnosis of HF unlikely. The ECG may reveal abnormalities such as AF, Q waves, LV hypertrophy , and a widened QRS complex that increase the likelihood of a diagnosis of HF and also may guide therapy.
Measurement of NPs are recommended, if available. A plasma concentration of B-type natriuretic peptide < 35 pg/mL, N-terminal pro-B-type natriuretic peptide < 125 pg/mL, or mid-regional pro-atrial natriuretic peptide < 40 pmol/L make a diagnosis of HF unlikely. These will be discussed in more detail in section 4.2.,
Basic investigations such as serum urea and electrolytes, creatinine, full blood count, liver and thyroid function tests are recommended to differentiate HF from other conditions, to provide prognostic information, and to guide potential therapy.
What Is Acute Heart Failure
Heart failure is a life-threatening condition. When it occurs, your heart is still working, but it cannot deliver oxygen-rich blood throughout your body. With acute heart failure, you experience a sudden, rapid decline in heart functioning and the amount of blood your heart can pump to the rest of your body.
Causes And Symptoms Of Acute Heart Failure
The most common cause of acute heart failure is a heart attack . This is caused by blockages in the arteries supplying blood to the heart muscle. Other causes include viruses, severe infections, allergic reactions, blood clots in the lungs, certain medications, or an illness that can attack the heart muscle.1
Shortness of breath is the most common symptom of AHF. Acute heart failure can also present with symptoms of rapid swelling and fluid retention characterized by sudden weight gain, up to several pounds in a 24-hr period. Coughing, wheezing, difficulty laying flat to sleep, as well as an irregular heartbeat can also be symptoms. In some cases, it is related to pre-existing cardiomyopathy. AHF often requires unexpected hospital admission. This tends to have a poor prognosis, with a high risk of readmission and death post-discharge.1 Seek emergency medical treatment if sudden or painful symptoms develop.
You May Like: What Should Your Heart Rate Be When Walking
Causes Of Heart Failure
Heart failure is often the result of a number of problems affecting the heart at the same time.
Conditions that can lead to heart failure include:
- coronary heart disease where the arteries that supply blood to the heart become clogged up with fatty substances , which may cause angina or a heart attack
- high blood pressure this can put extra strain on the heart, which over time can lead to heart failure
- conditions affecting the heart muscle
- heart rhythm problems , such as atrial fibrillation
- damage or other problems with the heart valves
- congenital heart disease birth defects that affect the normal workings of the heart
Sometimes obesity, anaemia, drinking too much alcohol, an overactive thyroid or high pressure in the lungs can also lead to heart failure.
The Diagnosis Of Heart Failure With Reduced Ejection Fraction
The diagnosis of HFrEF requires the presence of symptoms and/or signs of HF and a reduced ejection fraction . This is most usually obtained by echocardiography. Details about the quality standards that should be adhered to when determining the presence of reduced LV systolic function by echocardiography can be found in the European Association of Cardiovascular Imaging position paper. If assessment of EF is not possible by echocardiography, then CMR or rarely, nuclear techniques can be employed.
An algorithm for the diagnosis of HFrEF is depicted in Figure . For the investigation of the underlying aetiology, please refer to Table .
Also Check: Salt And Heart Attacks
Education Counselling And Support
- A role is emerging for heart failure liaison nurses in educating and supporting patients and their families, promoting long term compliance, and supervising treatment changes in the community
- Depression is common, underdiagnosed, and often undertreated counselling is therefore important for patients and families, and the newer antidepressants seem to be well tolerated and are useful in selected patients
Short term bed rest is valuable until signs and symptoms improve: rest reduces the metabolic demand and increases renal perfusion, thus improving diuresis. Although bed rest potentiates the action of diuretics, it increases the risk of venous thromboembolism, and prophylactic subcutaneous heparin should be considered in immobile inpatients. Full anticoagulation is not advocated routinely unless concurrent atrial fibrillation is present, although it may be considered in patients with very severe impairment of left ventricular systolic function, associated with significant ventricular dilatation. Intravenous loop diuretics may be administered to overcome the short term problem of gut oedema and reduced absorption of tablets, and these may be used in conjunction with an oral thiazide or thiazide-like diuretic . Low dose spironolactone improves morbidity and mortality in severe heart failure, when combined with conventional treatment . Potassium concentrations should be closely monitored after the addition of spironolactone.
Congestive Heart Failure: Prevention Treatment And Research
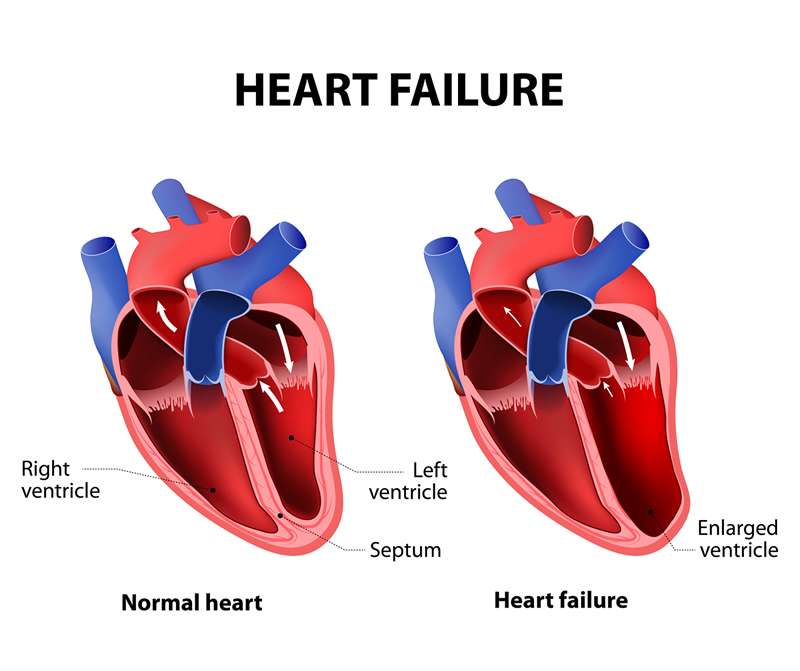
Congestive heart failure is a serious condition in which the heart doesnt pump blood as efficiently as it should. Despite its name, heart failure doesnt mean that the heart has literally failed or is about to stop working. Rather, it means that the heart muscle has become less able to contract over time or has a mechanical problem that limits its ability to fill with blood. As a result, it cant keep up with the bodys demand, and blood returns to the heart faster than it can be pumped outit becomes congested, or backed up. This pumping problem means that not enough oxygen-rich blood can get to the bodys other organs.
The body tries to compensate in different ways. The heart beats faster to take less time for refilling after it contractsbut over the long run, less blood circulates, and the extra effort can cause heart palpitations. The heart also enlarges a bit to make room for the blood. The lungs fill with fluid, causing shortness of breath. The kidneys, when they dont receive enough blood, begin to retain water and sodium, which can lead to kidney failure. With or without treatment, heart failure is often and typically progressive, meaning it gradually gets worse.
More than 5 million people in the United States have congestive heart failure. Its the most common diagnosis in hospitalized patients over age 65. One in nine deaths has heart failure as a contributing cause.
Recommended Reading: Does Clonidine Lower Heart Rate
Causes Of Acute Heart Failure
Many conditions can weaken or damage the heart over time. This can lead to heart failure.
With chronic heart failure, your heart tries to adapt to the additional strain over time until it just cant adapt anymore. Thats when acute heart failure happens.
Its also possible for acute heart failure to happen even in people who otherwise seem healthy. There are a number of conditions that can put a sudden strain on your heart.
Causes of acute heart failure include:
- coronary artery disease, which can cause a narrowing of the arteries
- heart attack, which causes damage to the heart muscle and is often caused by coronary artery disease
- use of certain illegal drugs, such as cocaine
- chemotherapy and radiation treatments
In the United States, Black and Hispanic people receive heart failure diagnoses more often than people from other racial or ethnic groups. And Black people in the United States are also at the highest risk of dying from heart failure.
These trends are related to racism and inequities in healthcare, according to the American College of Cardiology.
To diagnose acute heart failure, your doctor will run certain tests. Your doctor can then identify your stage of heart failure, to help find the right treatment for you.
What Are The Treatments For Heart Failure
Your treatment will depend on the type of heart failure you have and how serious it is. There’s no cure for heart failure. But treatment can help you live longer with fewer symptoms.
Even with treatment, heart failure usually gets worse over time, so you’ll likely need treatment for the rest of your life.
Most treatment plans include:
You may need heart surgery if:
- You have a congenital heart defect or damage to your heart that can be fixed.
- The left side of your heart is getting weaker and putting a device in your chest could help. Devices include:
- A biventricular pacemaker .
- A mechanical heart pump or a total artificial heart).
As part of your treatment, you’ll need to pay close attention to your symptoms, because heart failure can worsen suddenly. Your provider may suggest a cardiac rehabilitation program to help you learn how to manage your condition.
Don’t Miss: 100 Resting Heart Rate
When To Get Emergency Help
Heart failure is not the same thing as a heart attack. But, like a heart attack, acute heart failure can be a life threatening event. Someone with acute heart failure will typically need emergency hospital care. If your symptoms are sudden or severe, call 911 or your local emergency services for help.
If not treated, heart failure can lead to serious complications. These complications can include cardiac arrest, which is when your heart stops beating.
Some people with heart failure may have several health conditions. If thats the case, it can be hard to know whats causing your symptoms.
But when it comes to symptoms of heart failure, its best to get them checked by a doctor right away. According to a 2017 study, fast treatment of acute heart failure can lead to better outcomes.
Treatments For Heart Failure
Treatment for heart failure usually aims to control the symptoms for as long as possible and slow down the progression of the condition.
How you’re treated will depend on what is causing your heart failure.
Common treatments include:
- lifestyle changes including eating a healthy diet, exercising regularly and stopping smoking
- medicine a range of medicines can help many people need to take 2 or 3 different types
- devices implanted in your chest these can help control your heart rhythm
- surgery such as a or a heart transplant
Treatment will usually be needed for life.
A cure may be possible when heart failure has a treatable cause. For example, if your heart valves are damaged, replacing or repairing them may cure the condition.
Recommended Reading: Can You Live With Heart Failure
Will I Need Other Treatments
After you leave the hospital, you may need medications, like beta blockers or water pills, to maximize heart health. Other treatments may be necessary to prevent future episodes of acute heart failure.
These treatments may include surgery to:
- Stent placement or coronary bypass surgery for coronary artery disease.
- Repair or replace worn-out heart valves .
- Implant a pacemaker or implantable cardioverter defibrillator to help you maintain a regular heartbeat and help treat dangerous heart rhythms.
- Replace your heart with a healthy one from a donor .
- Give your heart extra help with a ventricular assist device until you can have a transplant.
Diagnosis And Treatment Of Chronic Heart Failure
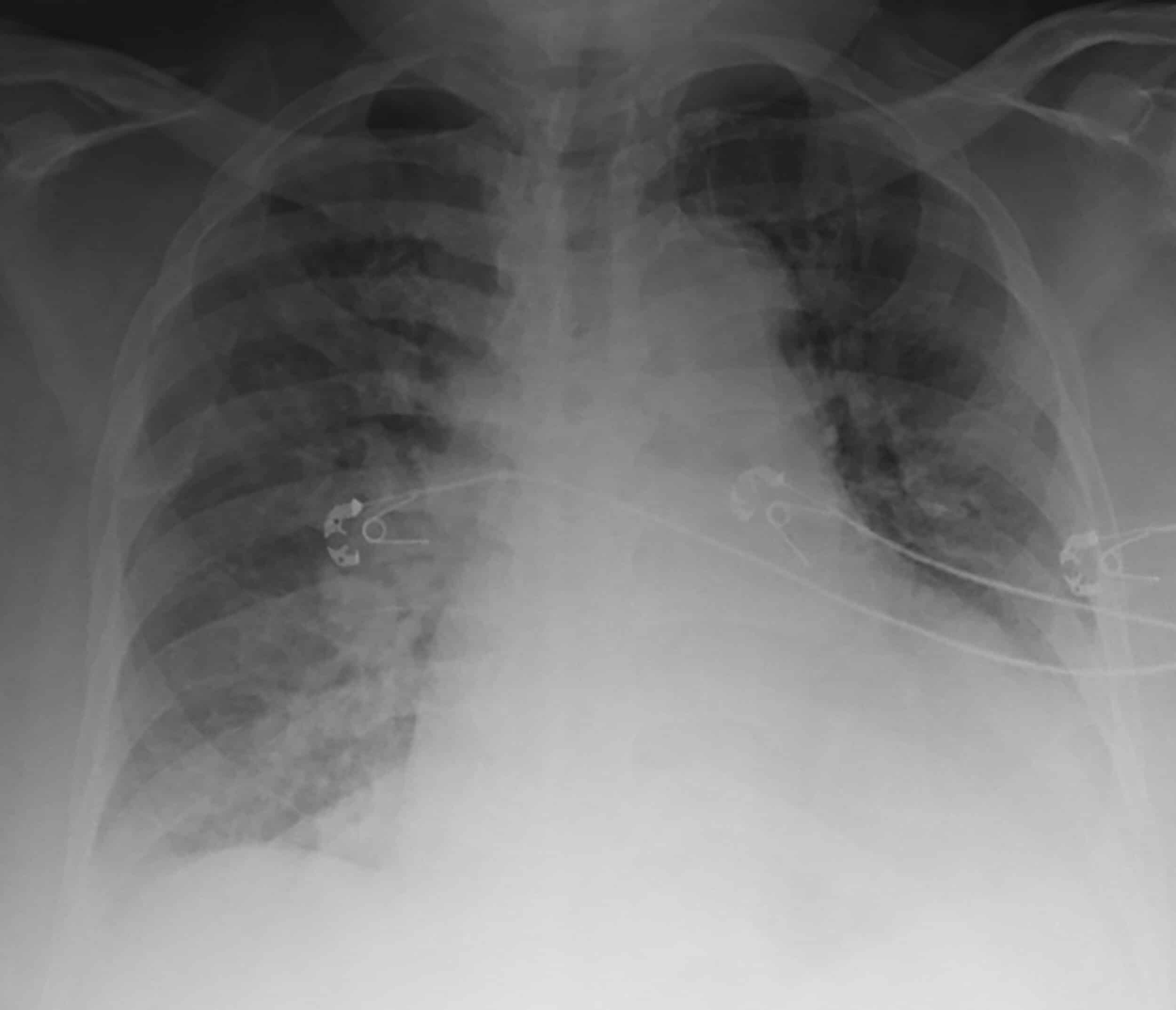
The diagnosis of chronic heart failure uses the same format as when diagnosing acute heart failure. A physician will take a complete medical history and perform a physical exam to detect congestion and fluid buildup or abnormal heart rhythms. Blood and imaging tests are also used to diagnose the type of heart failure and to determine how severe it is. To determine the most appropriate treatment, heart failure is generally classified by doctors to assess the stage and functional status of HF according to the severity of their self-reported symptoms.2,3
Chronic HF is a life-long condition that will get worse over time. It generally cannot be cured but it can be medically managed over a lifetime. Treatments may be able to improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes require effort, but increasing exercise, reducing dietary sodium, managing stress, and losing weight may improve quality of life.2
Read Also: Congested Heart Failure Symptoms
Factors That Can Worsen Symptoms Of Heart Failure
The symptoms of heart failure can be worsened by a number of factors, including:
- too much salt, fluid, or alcohol in the diet
- some viral and bacterial infections
- kidney diseases
Treatment for heart failure may include:
- medicines, such as
- diuretics to remove excess fluid and improve symptoms of heart failure
- mineralcortiocoid receptor antagonists are also recommended and used in most patients with heart failure to reduce mortality and hospitalisation
- ACE inhibitors to open up blood vessels, reduce blood pressure and reduce sodium retention and water retention
- certain beta-blockers to slow the heart rate and reduce its work
- aldosterone blockers to reduce blood pressure and reduce the effects of damage to the heart muscle
- ACE inhibitors, beta blockers and aldosterone blockers can increase survival and reduce the likelihood of hospitalisation.
Surgery And Medical Devices
Surgery is sometimes used to treat heart failure. Your doctor may use one of the following devices to help restore function:
- Biventricular pacemaker. This device helps both sides of your heart beat at the correct speed by sending electrical impulses.
- Implantable cardioverter defibrillators . An ICD is implanted under your skin, like a pacemaker. It monitors your heart rate and uses an electrical signal to correct it when needed.
- Heart pumps. An implant such as a ventricular assist device can help your heart pump blood more strongly.
Depending on your overall heart health, other procedures can include:
- Heart valve replacement or repair. If your heart fails because of a problematic heart valve, your doctor may repair or replace the valve.
- Coronary bypass surgery. In this surgery, your surgeon will remove a blood vessel from another part of your body. This blood vessel is fashioned into a new pathway to work around a clogged artery. Sometimes a less invasive alternative, such as angioplasty with stent placement, can be used instead.
- Heart transplant. If your condition is severe and other treatments arent working, your doctor may recommend heart transplant surgery.
Recommended Reading: Can 30 Year Olds Have Heart Attacks
Treatments For Patients With Heart Failure With Mildly Reduced Ejection Fraction
As in other forms of HF, diuretics should be used to control congestion. No substantial prospective RCT has been performed exclusively in patients with HFmrEF . Some data can be gleaned from subgroup analysis of trials in HFpEF, none of which have met their primary endpoint. Although strong recommendations cannot be made about specific therapies at this point in time, we have included a Table of Recommendations to help guide the management of patients in this category.
Pharmacological treatments to be considered in patients with heart failure with mildly reduced ejection fraction
ACE-I=angiotensin-converting enzyme inhibitor ARB=angiotensin-receptor blocker HF=heart failure HFmrEF=heart failure with mildly reduced ejection fraction MRA=mineralocorticoid receptor antagonist NYHA=New York Heart Association.
7.3.1 Angiotensin-converting enzyme inhibitors
There are no specific trials of ACE-I in patients with HFmrEF. Although, the PEP-CHF trial was conducted in patients with HFpEF and included patients with an LVEF > 40%, it did not report outcomes according to LVEF.
However, in patients with HFmrEF, many will also have CAD, hypertension, or post-MI LV systolic dysfunction and will, therefore, already be treated with ACE-I.
Therefore, ACE-I use may be considered in patients with HFmrEF.
7.3.2 Angiotensin receptor II type 1 receptor blockers
7.3.3 Beta-blockers
7.3.4 Mineralocorticoid receptor antagonists
7.3.6 Other drugs
7.3.7 Devices
Pathophysiological Mechanisms Of Ahf
An underlying structural or functional cardiac condition is a prerequisite for AHF and includes a multitude of different acute or chronic cardiac pathologies. The underlying cardiac disease leads to the activation of several pathophysiological pathways that counter the negative effects of HF on oxygen delivery to the peripheral tissues, but such pathways can also eventually cause systemic congestion, ventricular remodelling and organ dysfunction. Furthermore, some acute diseases can act as precipitating factors and trigger AHF either by directly impairing cardiac diastolic and/or systolic function or by further promoting systemic congestion. Systemic congestion has a major effect on the clinical presentation in the majority of patients with AHF and is a relevant determinant of multi-organ dysfunction occurring in AHF . The pathophysiology of AHF is heterogeneous, as it is greatly affected by the nature of the underlying cardiac disease. It is perhaps not surprising, therefore, that the responses to treatment may vary and that different patients may respond best to distinct treatment strategies that depend on the underlying pathophysiology.
Fig. 1: Schematic representation of possible pathophysiological mechanisms in AHF.
LV systolic and diastolic dysfunction
Fluid retention
Fluid redistribution
Also Check: High Heart Rate At Rest
Whereas The Benefits Of Aceis Appear To Be Class Specific
Although there was initial optimism surrounding the use of tissue ACEIs vs non-tissue ACEIs, there appears to be no significant difference in outcomes between agents, and the benefits appear to be a class effect.41 Conversely, the beneficial effects of -blockers are thought to be limited to specific drugs. -Blockers with intrinsic sympathomimeticactivity and other agents, including bucindolol, have not demonstrated a survival benefit.42,43 On the basis of these studies, we recommend that -blocker use be restricted to carvedilol, bisoprolol, and metoprolol succinate, agents proven to improve survival in clinical trials.
