Who Gets Diastolic Dysfunction
Diastolic dysfunction and diastolic heart failure are relatively new cardiac diagnoses. They have always been around, of course, but it is only in the past three decades or so, since echocardiography has been widely used to diagnose heart problems, that these conditions have become commonly recognized.
The diagnosis of diastolic dysfunction is now made quite frequently, especially in people over 45 years of age, most of whom are shocked to hear they have a heart problem at all. While some of these people will go on to develop actual diastolic heart failure, many will notespecially if they get appropriate medical care and take care of themselves.
Similarly, diastolic heart failure is also diagnosed frequently today. Almost half the patients who come to emergency rooms with episodes of acute heart failure turn out to have diastolic heart failure.
People with diastolic dysfunction and diastolic heart failure are likely to be older , overweight or obese, hypertensive, female, and have no history of heart attacks. It is currently believed that the risk of developing diastolic dysfunction is the same in men and women, but that older men who are obese and have hypertension are more likely to have heart attacks than women of similar ageso their heart failure is more likely to be standard congestive heart failure than diastolic heart failure.
Treatment Of Comorbid Atrial Fibrillation And Cad
Atrial fibrillation is common in patients with HFpEF. The ACC/AHA and ESC guidelines recommend treatment of atrial fibrillation in these patients.3,5 Management includes identification and treatment of underlying causes , anticoagulation guided by appropriate risk stratification, and rate-control strategies using beta blockers, calcium channel blockers, and digoxin. No evidence supports a rhythm-control strategy unless rate control does not control symptoms.3,5 Complete revascularization is associated with improved mortality in patients with HFpEF and CAD who meet criteria for revascularization.3,30
When To Get Medical Advice
See a GP if you experience persistent or gradually worsening symptoms of heart failure.
Call 999 for an ambulance or go to your nearest A& E department as soon as possible if you have sudden or very severe symptoms.
A number of tests can be used to help check how well your heart is working, including blood tests, an ECG and an echocardiogram.
Don’t Miss: How Long Does Heart Attack Pain Last
How Does Diastolic Heart Failure Affect My Body
When the left side of your heart stiffens, your heart:
- Cant relax properly between beats.
- Doesnt fill up with as much blood as it should.
- Pumps out less blood to the rest of your body than a healthy heart would.
As a result, you experience symptoms of heart failure. You might feel short of breath or fatigued . Your breathing may get worse at night when you try to lay flat. You may also notice swelling in your belly or legs . These symptoms might get worse over time.
Heart Failure Vs Congestive Heart Failure: What’s The Difference
Heart failure affects people of all ages, from children and young adults to the middle-aged and older adults. About 6.2 million adults in the United States are currently living with heart failure, and over 64 million people are dealing with some form of heart failure worldwide.
Approximately 550,000 new cases are diagnosed in the United States each year, but many more remain undiagnosed as the initial symptoms of heart failure can be subtle and mimic similar symptoms seen in other conditions.
Congestive heart failure refers to the inadequate functioning of the heart muscle such that fluid builds up in the lungs, abdomen, feet, and arms . The condition can either be acute or chronic .
Untreated heart disease can be aggressive and fatal. The five-year survival rate is about 50% for all stages. In 2018, heart failure led to nearly 400,000 deaths, according to death certificate data, with the highest prevalence of disease primarily in the South and Midwest.
You May Like: Difference Between Heart Failure And Congestive Heart Failure
How Is Diastolic Heart Failure Diagnosed
Your healthcare provider asks you about your symptoms and family health history. Your provider also conducts a physical exam and listens to your heart with a stethoscope.
You may have specific tests to diagnose heart failure, such as:
- Chest X-ray to take images of your chest and heart.
- Electrocardiogram , a record of the electrical activity in your heart.
- Echocardiogram, using sound waves to evaluate the structure and function of your heart muscle and valves.
- Exercise stress test, increasing your heart rate with medicine or as you walk on a treadmill to see how your heart responds.
- Cardiac catheterization, using a catheter to measure your hearts pressure and blood flow.
Treatment And Medication Options For Congestive Heart Failure
Heart failure is a chronic condition, and there is no cure. However, once youve been diagnosed, there are several things you can do to treat the condition and manage it so that it does not progress. Chief among them are lifestyle changes. That includes exercising and maintaining a heart-healthy diet thats low in saturated fat, trans fats, and cholesterol.
Also Check: Risk Factors For Heart Attack
Causes Risk Factors And Symptoms Of Diastolic Heart Failure
The causes of diastolic heart failure development include coronary heart disease, diabetes, high blood pressure, and obesity/inactivity. The most common cause of diastolic dysfunction and failure is chronic hypertension. This leads to left ventricular hypertrophy, which decreases cardiac compliance. Chronic hypertension also leads to increased connective tissue content.
There are several risk factors that could contribute to the condition, including the following:
- Aging: With age, the heart muscle begins to stiffen, preventing it from properly filling with blood.
- Hypertrophic cardiomyopathy: This abnormality of the heart muscle is inherited and causes the walls of the left ventricle to thicken.
- Aortic stenosis: When the opening of the aortic valve is narrowed, the left ventricle can thicken.
- Pericardial disease: This abnormality in the sac around the heart leads to fluid buildup in the pericardial space.
Diastole is when the heart returns to its relaxed state. In this condition, changes in pressure-volume of the heart lead to symptoms of diastolic heart failure. It is a complex process that is affected by factors such as heart rate, velocity of relaxation, cardiac compliance, hypertrophy, segmental wall coordination of the heart muscle, and more.
The relaxation process has four phases specialists can identify:
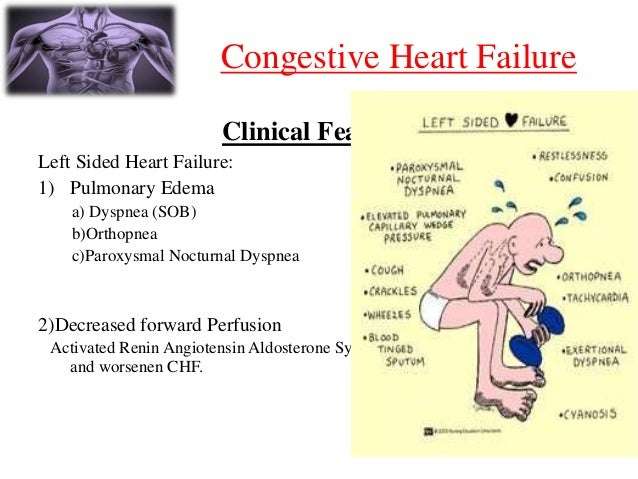
Symptoms and signs of heart failure include the following:
- Shortness of breath
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Also Check: What Caused Carrie Fisher’s Heart Attack
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
What Is Diastolic Dysfunction And Diastolic Heart Failure
The cardiac cycle is divided into two parts – systole and diastole. During systole, the ventricles contract, thus ejecting blood out of the heart and into the arteries. After the ventricles have finished contracting, they relax, and during this relaxation they fill up with blood to prepare for the next systole. This relaxation phase of the cardiac cycle is called diastole.
Sometimes, as a result of various medical conditions, the ventricles begin to become relatively stiff. Stiff ventricles are not able to fully relax during diastole as a result, the ventricles may not fill completely. As a result of this incomplete filling of the ventricles, the amount of blood pumped with the subsequent heart beat will be slightly reduced. Also, the blood which is returning to the heart can partially dam up in the bodys organs, including the lungs. Even more common, however, is swelling in the legs.
The abnormal stiffening of the ventricles and the resulting abnormal ventricular filling during diastole are referred to as diastolic dysfunction.
Diastolic dysfunction is very mild at first, and usually does not produce symptoms at first. However, diastolic dysfunction tends to progress over time. When the condition becomes is sufficiently advanced to produce pulmonary congestion or swelling in the legs, diastolic heart failure is said to be present.
Dont Miss: Does Acid Reflux Cause Heart Palpitations
You May Like: Symptoms Woman Having Heart Attack
Summary Of Treatment Recommendations
Patients with HFpEF and symptoms of volume overload should be treated with diuretics.31 Hypertension should be treated according to appropriate guidelines.3 Although RCTs of several medications showed fewer heart failure hospitalizations, this benefit was offset by increases in hospitalizations for other reasons. Thus, in the absence of hypertension, the evidence does not support treating patients with HFpEF with any medication except diuretics. Additionally, RCTs of angioten-sin receptor blockers, nitrates, and spironolactone raise concerns about adverse effects, and physicians should avoid using these medications, if possible.18,2325 Similarly, physicians should avoid the use of digoxin in patients 65 years and older.27 Physicians should consider referring patients with HFpEF who can exercise safely for exercise training or cardiac rehabilitation. Comorbid atrial fibrillation or CAD should be treated.
Atrial Natriuretic Peptide And B
ANP and BNP are endogenously generated peptides activated in response to atrial and ventricular volume/pressure expansion. ANP and BNP are released from the atria and ventricles, respectively, and both promote vasodilation and natriuresis. Their hemodynamic effects are mediated by decreases in ventricular filling pressures, owing to reductions in cardiac preload and afterload. BNP, in particular, produces selective afferent arteriolar vasodilation and inhibits sodium reabsorption in the proximal convoluted tubule. It also inhibits renin and aldosterone release and, therefore, adrenergic activation. ANP and BNP are elevated in chronic heart failure. BNP especially has potentially important diagnostic, therapeutic, and prognostic implications.
For more information, see the Medscape Drugs & Diseases article Natriuretic Peptides in Congestive Heart Failure.
You May Like: What Should My Heart Rate Be While Exercising
Etiology Congestive Heart Failure
The various causes for diastolic congestive heart failure are listed below:
Hypertension causes left ventricular hypertrophy, or LVH, and impaired relaxation. Over time, this progresses, resulting in higher degrees of diastolic dysfunction, low cardiac output and symptoms of congestive HF.
The aging process of the heart is not well understood, but fibrotic changes are seen within the myocardium. This results in a relaxation abnormality that is almost universally present by the age of 60. In the elderly, this can progress, causing significant diastolic impairment and congestive heart failure.
Restrictive cardiomyopathies frequently cause deposition of substances within the myocardium, causing diastolic relaxation abnormalities and, when severe, diastolic congestive HF.
Valvular heart disease such as mitral stenosis technically causes heart failure due to diastolic dysfunction of the left ventricle. Severe aortic stenosis causes LVH, and when left ventricular pressures increase a significant amount, diastolic HF can occur.
When a tachyarrhythmia such as atrial fibrillation occurs with an uncontrolled ventricular response, congestive HF can occur in the setting of normal systolic function from a shortened diastolic filling time. This is technically a form of diastolic HF however, once ventricular rates are controlled, the cardiac hemodynamics should dramatically improve.
Invasive Assessment Of Diastolic Function
Cardiac catheterization with simultaneous pressure and volume measurements is the gold standard for assessing LV diastolic function. Prerequisites are high-fidelity pressure recordings with simultaneous angio- or echocardiography or the use of the conductance technique. The rate of LV relaxation, rate and timing of diastolic filling as well as myocardial and chamber stiffness can be determined .
2.3.1 Isovolumic relaxation
The most commonly used index for quantitation of isovolumic relaxation is the time constant of relaxation . The pressure fall has been shown to be exponential under most circumstances but may deviate from a true mono-exponential pressure curve in aortic regurgitation or during myocardial ischemia. Calculation of the time constant of relaxation is currently the only reliable method for measuring the rate of relaxation . All other parameters such as isovolumic relaxation time, peak negative dP/dt, etc. are not true representatives of LV relaxation but are dependent on heart rate, peak systolic pressure, etc.
2.3.2 Diastolic filling
2.3.3 Passive diastolic function
PaVcSaEC
Read Also: How Low Should Your Heart Rate Be When Sleeping
Pulmonary Hypertension And Right Ventricular Dysfunction
Most HFpEF patients exhibit pulmonary hypertension which is significantly associated with increased morbidity and mortality. Left atrial and pulmonary venous pressure increases in HFpEF due to diastolic insufficiency thus increasing pulmonary artery pressure. In patients with advanced HFpEF changes in the pulmonary vasculature may develop, leading to pre-capillary pulmonary hypertension. Right ventricular dysfunction is also common in HFpEF patients, occurring in 20-35% of patients. This right ventricular dysfunction is more common in patients with more advanced HFpEF as well as those with pulmonary hypertension and lower ejection fractions.
Complications Of Congestive Heart Failure
- Rapid Weight Loss Severe heart failure can lead to a rapid loss of weight that can be life-threatening. Heart failure can cause blood to back up into the liver and intestines, causing these organs to swell. This swelling can lead to nausea and loss of appetite, and can prevent the body from absorbing nutrients from food.
- Impaired Kidney Function Congestive heart failure weakens the hearts ability to pump blood, reducing blood flow to the kidneys. This can lead to kidney damage or kidney failure, if left untreated.
- Liver Damage Heart failure can cause fluid to build up in the liver, which can lead to scarring. This makes it more difficult for the liver to carry out its day-to-day functions.
- Arrhythmias Heart failure results in damaged heart muscles, which can lead to the development of an arrhythmia, or abnormal heart beat. Arrhythmias can include the heart beating too quickly, beating too slowly, or beating irregularly.
- Heart Valve Problems If the heart is enlarged due to heart failure, the valves of the heart, which ensure appropriate direction of blood flow through the organ, may not function properly.
- Angina and Heart Attack Heart disease is a major contributing factor in many heart failure cases, and people with congestive heart failure are at continued risk of angina and heart attack.
Read Also: How Many Heart Attacks Did Dick Cheney Have
Diastolic Heart Failure: Causes Symptoms Treatment And Life Expectancy
Diastolic heart failure occurs when the lower left chamber of the heart, known as the left ventricle, is unable to fill with blood during the diastolic phase . This reduces the amount of blood pumped out to the body. If the left ventricle muscle becomes stiff or thickened, diastolic heart failure is the result. In this case, the heart must increase the pressure inside the ventricle to fill it with enough blood. Prolonged behavior like this causes blood to build up inside the left atrium and then the lungs. This leads to fluid congestion and heart failure symptoms.
Acute On Chronic Systolic Or Diastolic Congestive Heart Failure Admission
Scenario:
Patients have a history of CHF most of the time. New onset CHF is also seen in ER. They develop pedal edema gradually at home but recently they might have had more shortness of breath, tiredness, more swelling, cough, PND or orthopnea, etc. Not uncommonly, patients ate lot of salted chips, pretzels, or drank soup bought from store with high salt content immediately before they present in ER. This is relatively common. Some patients keep drinking a lot of water like they always did when they were young.
EMS:
Oxygen via Nasal cannula or Non Rebreather mask depending on necessity.
Lasix if diagnosis is very clear to the EMS staff.
Routine labs plus BNP, EKG, CXR
Oxygen
IV Lasix 40-80 mg x 1, Foley catheter placement
ABG, BiPap or Intubation if necessary> ICU if intubated
Observe in Telemetry floor. Can make them inpatient if patient has severe electrolyte disturbances, tachycardia, hypotension, worsening kidney function or if requiring BiPap etc.
Low salt diet-2gm Sodium diet, fluid restriction to 1500ml.
Continue IV Lasix 40-60mg Q 2-3 times a day .
Input/Output.
Cardiac Enzymes Q3hrs 2 or 3 times.
2D ECHO
Lipid Panel in AM labs.
Elevate legs with pillows above heart level and also elevate head of the bed to help with breathing
Cardiology consult
ACEI or ARB if EF < 40%-for after load reduction.
Coreg or Toprol XL, Start Beta Blockers at low doses and when patient is euvolemic.
Hydralazine and Nitrates esp. if African American Patients.
IV Lasix +/-Metolazone.
Recommended Reading: What Side Of The Heart Pumps Blood To The Lungs
