Other Descriptive Terms In Heart Failure
Right and left heart failure refer to syndromes presenting predominantly with congestion of the systemic or pulmonary veins. The terms do not necessarily indicate which ventricle is most severely damaged. High- and low-output, forward and backward, overt, treated, and congestive are other descriptive terms still in occasional use the clinical utility of these terms is descriptive without etiological information and therefore of little use in determining modern treatment for heart failure.
Mild, moderate, or severe heart failure is used as a clinical symptomatic description, where mild is used for patients who can move around with no important limitations of dyspnea or fatigue, severe for patients who are markedly symptomatic and need frequent medical attention and moderate for the remaining patient cohort.
When Should I Call An Ambulance
If you have any of the symptoms below, call triple zero immediately and ask for an ambulance. If calling triple zero does not work on your mobile phone, try calling 112.
- chest pain thats severe or worsening, or has lasted longer than 10 minutes
- chest pain that feels heavy, crushing or tight
- other symptoms, such as breathlessness, nausea, dizziness or a cold sweat
- pain in your jaw or down your left arm
Center For Advanced Heart Failure/cardiomyopathy At Brigham And Womens Hospital
The Center for Advanced Heart Failure/Cardiomyopathy, an integral part of the Heart & Vascular Center at Brigham and Womens Hospital , brings together heart failure experts, including cardiologists, interventional cardiologists, cardiac surgeons, cardiovascular imaging specialists, congenital heart disease specialists, and many others, to care for patients as one team. Together, the team tailors therapies to each patients needs, offering the latest medical, interventional, and surgical approaches to congestive heart failure treatment.
You May Like: Symptoms Of Congestive Heart Failure In Women
You Dont Have To Face Hf Alone
The term heart failure makes it sound like the heart is no longer working at all and theres nothing that can be done. Actually, heart failure means that the heart isnt pumping as well as it should be. Congestive heart failure is a type of heart failure that requires seeking timely medical attention, although sometimes the two terms are used interchangeably.
Your body depends on the hearts pumping action to deliver oxygen- and nutrient-rich blood to the bodys cells. When the cells are nourished properly, the body can function normally.With heart failure, the weakened heart cant supply the cells with enough blood. This results in fatigue and shortness of breath and some people have coughing. Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult.
Heart failure is a term used to describe a heart that cannot keep up with its workload. The body may not get the oxygen it needs.
Heart failure is a serious condition, and usually theres no cure. But many people with heart failure lead a full, enjoyable life when the condition is managed with heart failure medications and healthy lifestyle changes. Its also helpful to have the support of family and friends who understand your condition.
You May Like: How To Read Heart Rate Monitor
Facts About Heart Failure In The United States
- About 6.2 million adults in the United States have heart failure.1
- In 2018, heart failure was mentioned on 379,800 death certificates .1
- Heart failure costs the nation an estimated $30.7 billion in 2012.2 This total includes the cost of health care services, medicines to treat heart failure, and missed days of work.
Read Also: Stages Of Heart Failure In Dogs
Treatment For Heart Failure
- Angiotensin-converting enzyme inhibitors promotes vasodilation of the blood vessels, lowering the pressure and improving the blood flow .
- Beta blockers reduces heart rate and blood pressure .
- Angiotensin II receptor blockers similar to ACE inhibitors and can be used if the patient does not tolerate ACE inhibitors .
- Digitalis or digoxin improves the contraction of heart muscles, regulate heart rhythm and reduces heartbeat.
- Inotropes to improve the function of the heart to pump blood in severe heart failure.
- Diuretics to facilitate elimination of excess fluid in the body through urination .
- Inotropes. These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
2. Surgical interventions. These include coronary bypass surgery, heart valve repair or replacement, and heart transplant. It may also involve the insertion of medical devices such as implantable cardioverter-defibrillators , cardiac resynchronization therapy , and ventricular assist devices .
3. Lifestyle changes. A crucial part of the treatment plan for a patient with heart failure is to change several habits that are linked to the disease. These include smoking cessation, blood pressure control, diabetes management, dietary changes, stress management, exercise and increase in physical activity.
Pathophysiology Of Heart Failure
Normal myocardial function requires sufficient nutrient-rich, toxin-free blood at rest and during exercise sequential depolarization of the myocardium normal myocardial contractility during systole and relaxation during diastole normal intracardiac volume before contraction and limited resistance to the flow of blood out of the heart . The capacity of the heart to adapt to short-term changes in preload or afterload is remarkable, but sudden or sustained changes in preload , afterload , or demand may lead to progressive failure of myocardial function. Asymptomatic dysfunction progresses steadily to overt heart failure.
Coronary artery disease accounts for nearly 70 percent of all cases of heart failure.7 Less frequent causes include diabetes mellitus and valvular heart disease . Heart failure also can be multifactorial. For example, the disease can result from acute myocardial infarction with papillary muscle dysfunction and acute pulmonary edema .
| Common |
| Dyspnea, pulmonary vascular congestion, reduced left-sided contractility | |
| Biventricular failure | Dyspnea, dependent edema, jugular venous distention, pulmonary vascular congestion, bilateral reduced contractility |
Although the symptoms, causes, prevalence, and epidemiology of the six different types of heart failure are somewhat different, there is substantial overlap, and types may coexist. Therefore, this review presents an approach to diagnosis that is appropriate regardless of the type or cause of heart failure.
Recommended Reading: How To Reduce Risk Of Heart Attack
Stage A Treatment Options
Treatment options in stage A mainly focus on promoting your overall health and disease prevention. If you meet the stage A criteria, your doctor will recommend lifestyle changes to slow or stop disease progression.
Heart Failure Doctor Discussion Guide
Chf Nursing Care Plan 4
Nursing Diagnosis: Activity intolerance related to imbalance between oxygen supply and demand as evidenced by fatigue, overwhelming lack of energy, verbalization of tiredness, generalized weakness, and shortness of breath upon exertion
Desired Outcome: The patient will demonstration active participation in necessary and desired activities and demonstrate increase in activity levels.
| CHF Nursing Interventions | Rationales |
| Assess the patients activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. | To create a baseline of activity levels and mental status related to fatigue and activity intolerance. |
| Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Alternate periods of physical activity with rest and sleep. | To gradually increase the patients tolerance to physical activity. |
| Teach deep breathing exercises and relaxation techniques. Provide adequate ventilation in the room. | To allow the patient to relax while at rest and to facilitate effective stress management. To allow enough oxygenation in the room. |
| Refer the patient to physiotherapy / occupational therapy team as required. | To provide a more specialized care for the patient in terms of helping him/her build confidence in increasing daily physical activity. |
Recommended Reading: Can Flonase Cause Heart Palpitations
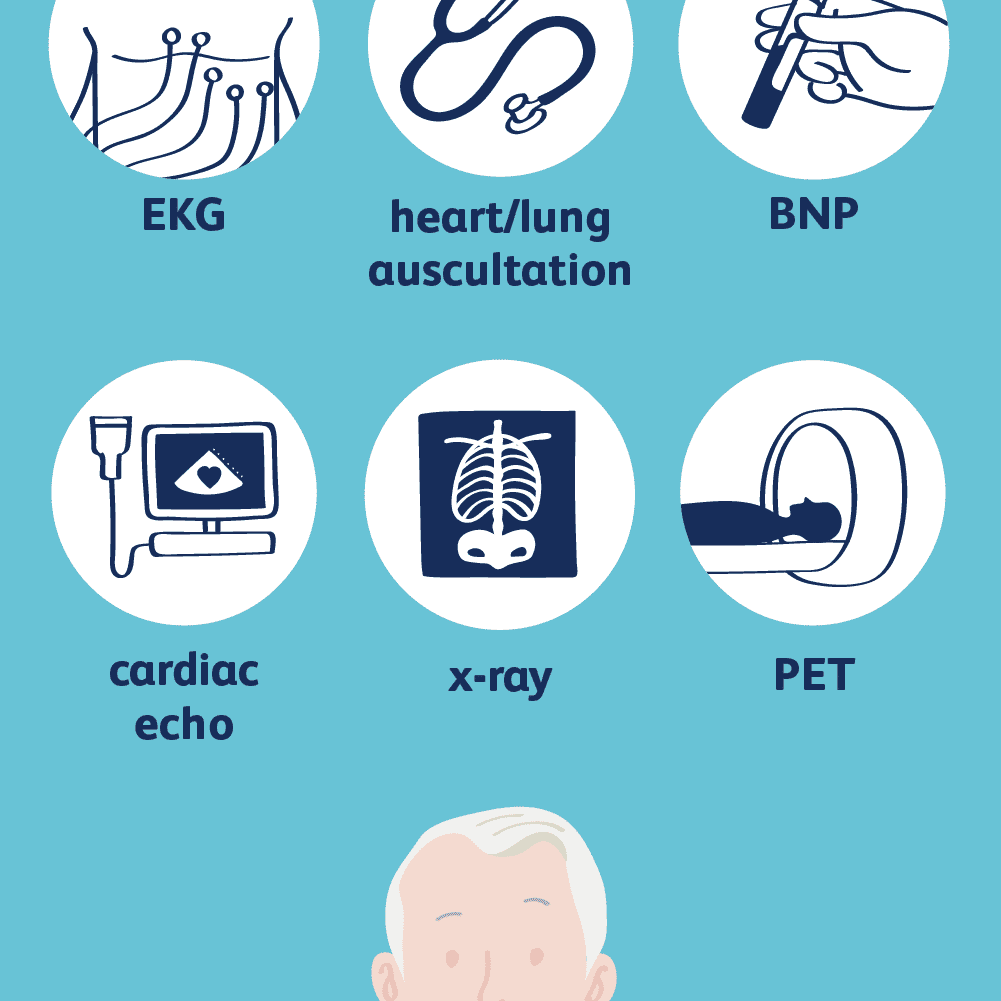
Tests To Measure Your Ejection Fraction
Your provider may order an echocardiography or other imaging tests to measure your ejection fraction. Your ejection fraction is the percent of the blood in the lower left chamber of your heart that is pumped out of your heart with each heartbeat. Ejection fraction measures how well your heart pumps. This helps diagnose the type of heart failure you have and guides your treatment.
- If 40% or less of the blood in your left ventricle is pumped out in one beat, you have heart failure with reduced ejection fraction.
- If 50% or more of the blood in your left ventricle is pumped out in one beat, you have heart failure with preserved ejection fraction.
- If your ejection fraction is somewhere in between 41% to 49%, you may be diagnosed with heart failure with borderline ejection fraction.
Liver Size And Hepatojugular Reflux
The key component of the abdominal examination is the evaluation of liver size. Hepatomegaly may occur because of right-sided heart failure and venous congestion.
The hepatojugular reflux can be a useful test in patients with right-sided heart failure. This test should be performed while the patient is lying down with the upper body at a 45-degree angle from the horizontal plane. The patient keeps the mouth open and breathes normally to prevent Valsalva’s maneuver, which can give a false-positive test. Moderate pressure is then applied over the middle of the abdomen for 30 to 60 seconds. Hepatojugular reflux occurs if the height of the neck veins increases by at least 3 cm and the increase is maintained throughout the compression period.18
Also Check: Can Heart Attack Symptoms Go On For Days
What Items Are Not Allowed In Checked Luggage Uk Tui
okla lottery
National Center for Health Statistics ICD-10-CM Fiscal Year: Select Fiscal Year: FY2022 – includes January 2022 Addenda FY2021 – includes January 2021 Addenda FY2020 – includes April 1, 2020 Addenda FY2019 – October 1, 2018.
ICD-10 Interactive Self Learning Tool. The WHO Electronic ICD–10-training tool is designed for self-learning,and classroom use. The modular structure of this ICD–10 training permits user groups specific tailoring of courses on individual paths, if desired. Detailed information is given in the introduction of the tool, and in the user guide.
what is a tunic
In ICD-11, PTSD is defined as a fear-based disorder characterized by three symptom clusters, namely re-experiencing of the trauma in the here and now, avoidance of traumatic reminders, and a persistent sense of current threat. The ICD-11 definitions for C-PTSD and PD are substantially comparable in terms of self- and interpersonal problems, and childhood. What is the ICD–10 code for new onset CHF? 21. What is the ICD 9 code for congestive heart failure? Table 1ICD-9-CM diagnosis codeDiagnosisDescriptionHeart failure428.0 Congestive.
in response to the covid-19 pandemic, the centers for medicare & medicaid services is implementing 2 new procedure codes, in addition to the 7 new procedure codes previously announced, bringing the total to 9 new procedure codes, to describe the introduction or infusion of therapeutics, including vaccines for covid-19 treatment, into the.
How Can I Improve My Quality Of Life With Heart Failure
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Eat a healthy diet. Limit your consumption of sodium to less than 1,500 milligrams each day. Eat foods high in fiber. Limit foods high in trans fat, cholesterol, and sugar. Reduce total daily intake of calories to lose weight if necessary.
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also decrease heart failure progression.
- Don’t overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
Also Check: Open Heart Surgery Recovery Stories
Chf Is Not A Death Sentence
While serious, congestive heart failure diagnosis doesnt mean your life is over. Its important to understand how manageable it is. By taking the right steps, patients can learn to live a happy and fulfilling life.
Will there be necessary lifestyle changes? Certainly. But it doesnt mean you have to stop what youre doing. Do regular physical exercises like walking, swimming, biking, and light-weight exercises. Avoid activities such as running in very hot or very cold weather or doing heavy lifting. Stick to a diet thats low in sodium and avoid processed foods.
Consult a doctor for the best steps to combat your CHF.
Patient Experiences
Chf Nursing Care Plan 5
Nursing Diagnosis: Excess Fluid Volume related to decreased cardiac output and increased glomerular filtration rate as evidenced by S3 heart sound, blood pressure level of 190/85, orthopnea, pitting edema of the ankles, and weight gain
Desired Outcome: The patient will demonstrate a balanced input and output, and stabilized fluid volume
| CHF Nursing Interventions | Rationales |
| Assess vital signs and auscultate lungs to find any crackles or wheezes. | Heart failure, especially left-sided HF may lead to pulmonary congestion, as evidenced by crackles or wheezes upon auscultation of the lungs. |
| Commence a fluid balance chart, monitoring the input and output of the patient. | To monitor patients fluid volume accurately and effectiveness of actions to monitor the progress of excess fluid volume. |
| Restrict fluid intake as instructed by the physician. | To reduce fluid volume and manage edema. |
| Weigh the patient on a daily basis. | Diuretics are needed to manage heart failure, but may put the patient at risk for sudden fluid loss, which is reflected through his/her weight. |
| Monitor patients serum electrolytes and renal function to the physician as needed. | The use of diuretics may result to excessive fluid shifts and electrolyte loss. |
Don’t Miss: What Causes Low Blood Pressure And High Heart Rate
Complications Of Congestive Heart Failure
- Rapid Weight Loss Severe heart failure can lead to a rapid loss of weight that can be life-threatening. Heart failure can cause blood to back up into the liver and intestines, causing these organs to swell. This swelling can lead to nausea and loss of appetite, and can prevent the body from absorbing nutrients from food.
- Impaired Kidney Function Congestive heart failure weakens the hearts ability to pump blood, reducing blood flow to the kidneys. This can lead to kidney damage or kidney failure, if left untreated.
- Liver Damage Heart failure can cause fluid to build up in the liver, which can lead to scarring. This makes it more difficult for the liver to carry out its day-to-day functions.
- Arrhythmias Heart failure results in damaged heart muscles, which can lead to the development of an arrhythmia, or abnormal heart beat. Arrhythmias can include the heart beating too quickly, beating too slowly, or beating irregularly.
- Heart Valve Problems If the heart is enlarged due to heart failure, the valves of the heart, which ensure appropriate direction of blood flow through the organ, may not function properly.
- Angina and Heart Attack Heart disease is a major contributing factor in many heart failure cases, and people with congestive heart failure are at continued risk of angina and heart attack.
Quality Of Patient Care
Brigham and Womens Hospital is committed to providing all of our patients with the safest, highest-quality, most-satisfying care possible and follow established protocols that have been shown to improve patient outcomes. Our inpatient satisfaction survey, sent to patients to assess their total care experience, helps us to monitor what we are doing well and areas for improvement. We pride ourselves in the quality of patient care we provide and how we are measured compared with other hospitals.
You May Like: How To Avoid Strokes And Heart Attacks
Third And Fourth Heart Sounds
A double apical impulse can represent an auscultated third heart sound . Just as with the displaced point of maximal impulse, a third heart sound is not sensitive for heart failure, but it is highly specific .14 Patients with heart failure and left ventricular hypertrophy can also have a fourth heart sound . The physician should be alert for murmurs, which can provide information about the cause of heart disease and also aid in the selection of therapy.
Chf Nursing Care Plan 3
Nursing Diagnosis: Deficient Knowledge related to new diagnosis of Congestive Heart Failure as evidenced by patients verbalization of I want to know more about my new diagnosis and care
Desired Outcome: At the end of the health teaching session, the patient will be able to demonstrate sufficient knowledge of congestive heart failure and its management.
Don’t Miss: How Do They Do Heart Bypass Surgery
What Is The Outlook For People With Heart Failure
With the right care, heart failure may not stop you from doing the things you enjoy. Your prognosis or outlook for the future will depend on how well your heart muscle is functioning, your symptoms, and how well you respond to and follow your treatment plan.
Everyone with a long-term illness, such as heart failure, should discuss their desires for extended medical care with their doctor and family. An “advance directive” or “living will” is one way to let everyone know your wishes. A living will expresses your desires about the use of medical treatments to prolong your life. This document is prepared while you are fully competent in case you are unable to make these decisions at a later time.
Show Sources
