Diuretic Resistance And Crs Syndrome
Several studies that used different metrics tried to establish a correlation between efficacy of diuretics and heart failure-related clinical outcomes. In the case of patients having reduced diuretic efficacy, Testani et al. found high mortality rates even after correcting for diuretic dose and fluid output. Valente et al. and Voors et al. observed increased death and rehospitalization rates associated with diuretic resistance in heart failure at 60 days, whereas Ter Maaten et al. reported similar outcomes at 30-day follow-up. After correcting for the GFR, Verbrugge et al. and Singh et al. reported higher death and rehospitalization rates related to diuretic resistance.
Acute CRS is a reflection of worsening renal function in patients with CHF . CRS is found in 2533% of all patients with acute decompensated heart failure . Extrarenal hemodynamic changes, cellular dysregulation, neurohormonal activation, and intrarenal microvascular and oxidative stress underlie acute CRS . In a few cases, intravenous diuretic-mediated renal injury is responsible for worsening renal function . Other proposed mechanisms of CRS pathophysiology include neurohumoral adaptations, reduced renal perfusions, elevated venous pressure, and dysfunction of the right ventricle .
Read Also: How To Lower Your Heart Rate While Running
What Are The Stages Of Congestive Heart Failure
The New York Heart Association has developed a scale that commonly is used to determine the functional capabilities of heart failure.
New York Heart Association Functional Classification of Heart Failure
How To Stay Safe
Hospitalization for a heart failure exacerbation could be especially tricky in the pandemic, particularly in areas where health systems are already strained. There are a number of ways you can keep your heart failure in check and avoid getting COVID-19:
- Make sure you are up to date on all of your vaccinations, including influenza and pneumonia vaccines.
- Ask your healthcare provider if you can stay in touch with them through virtual or telehealth appointments to limit your exposure.
- Discuss the necessity of certain health screenings or nonessential procedures with your practitioner.
- Make sure you keep a list of your current medications and doses with you at all times.
- Keep at least a 30-day supply of your medications on hand.
- Stay active and find ways to reduce stress while keeping social distancing recommendations in mind.
Don’t Miss: Why Use A Heart Rate Monitor
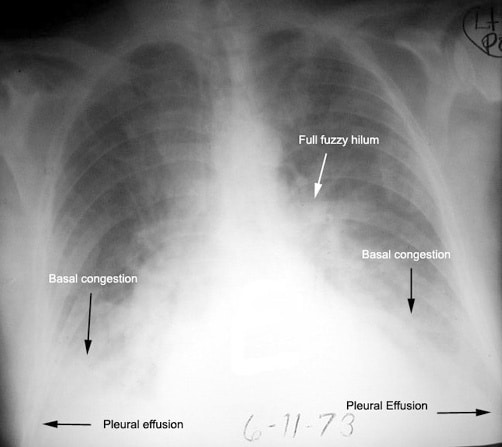
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Deterrence And Patient Education
Effective treatment of comorbidities and risk factor reduction can decrease the chance of developing heart failure. Patient education should be focused on ensuring compliance with prescribed evidence-based treatments.
- Hypertension effective treatment of systolic and diastolic hypertension can reduce the risk of heart failure by approximately 50%
- Diabetes is directly associated with the development of heart failure, independent of other associated clinical conditions
- Alcohol heavy alcohol use is associated with heart failure
- Metabolic syndromes important to keep up treatment based on evidence-based guidelines to decrease the risk of heart failure
- Patient education regarding dietary salt restriction and fluid restriction is imperative
Also Check: Stmptoms Of Heart Attack
Symptoms Of Reduced Pumping Capability
The most prominent symptoms are:
- Extreme weakness and fatigue
- Muscle weakness and muscle wasting
- Lethargy and inanition
- Extreme weight loss
Obviously, symptoms like this are not compatible with a long life. Unless the cardiac function can be improved, or unless cardiac transplantation or a ventricular assist device can be used, once a person with heart failure develops these kinds of symptoms, death usually follows relatively soon.
Also Check: Is Congestive Heart Disease Hereditary
If Youre Over 65 Be Sure To Follow The Latest Pneumonia Vaccine Guidelines
Each year, about a million people in the United States end up in the hospital with pneumonia, a serious lung infection that can be caused by an array of different viruses, bacteria, and even fungi. New research suggests that older people hospitalized with pneumonia face four times their usual risk of a having a heart attack or stroke or dying of heart disease in the month following the illness.
The risk declines over the following year, according to the report, published in the Jan. 20, 2015, Journal of the American Medical Association. Infections put added stress on your heart, forcing it to work harder. Your bodys efforts to fight the infection also trigger unhealthy changes inside your arteries, such as releasing chemicals that can make blood more likely to clot, which can lead to a heart attack or stroke.
Serious infections like pneumonia are linked to a higher risk of heart attack as well as worsening heart failure in people with that condition, says Dr. Scott Solomon, a professor of medicine at Harvard Medical School. For older people, the pneumonia vaccine may help prevent these dangerous complications, but an annual flu shot is also important, he notes. The same virus that causes the flu can also cause viral pneumonia in some people and nudge others to develop bacterial pneumonia.
Recommended Reading: Heart Rate When Having A Heart Attack
Risk Of Heart Failure After Community Acquired Pneumonia: Prospective Controlled Study With 10 Years Of Follow
- Accepted 11 January 2017
Pneumonia Risk Soars In Heart Failure Patients Especially Hfpef
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Patients with heart failure get pneumonia at a rate almost three times greater than expected and, once they do get pneumonia, have about a fourfold greater risk of death, investigators for a retrospective analysis of 13,000 patients from two landmark randomized HF trials have found.
Dr. John J.V. McMurray
The investigators also found that HF patients with preserved ejection fraction are at the highest risk of developing pneumonia. The findings underscore the importance of patients with HF getting a pneumonia vaccination, they found.
The analysis showed that 6.3% of patients in the PARADIGM-HF trial and 10.6% of those in the PARAGON-HF trial developed pneumonia, reported the study authors, led by John J.V. McMurray, MD, of the British Heart Foundation Cardiovascular Research Center at the University of Glasgow in Scotland .
The main reason for doing this study was the fact that many heart failure patients are not vaccinated, as they should be, against pneumonia both pneumococcus and influenza vaccination, Dr. McMurray said in an interview. We wanted to document the frequency and consequences of pneumonia in patients with heart failure to help highlight this deficiency in care.
Dr. McMurray said he believes this is the first study to document the incidence of pneumonia and pneumonia-related outcomes according to the two major ejection fraction phenotypes.
You May Like: Open Heart Surgery Name
The Role Of Platelets
Mirsaeidi et al. , recognising that platelets were inflammatory cells that played an important role in host antimicrobial defences, undertook a study to evaluate the association between abnormalities of the platelet count and 30-day mortality in patients with CAP. These investigators documented that the occurrence of either thrombocytopaenia or thrombocytosis were associated with in-hospital mortality in patients with CAP and that these abnormalities of the platelet count were better predictors of outcome than similar abnormalities of the leukocyte count.
Recent and novel insights into the pathogenesis of CAP-associated CVEs have been provided by the findings reported in a study by Cangemi et al. . This study, which did not distinguish between viral and bacterial CAP, confirmed the high risk for development of myocardial infarction, which peaked within 2 days of hospitalisation. Notwithstanding disease severity and heart ejection fraction, significant predictors of myocardial infarction included elevated concentrations of the circulating biomarkers of platelet activation, soluble CD40 ligand, P-selectin and thromboxane B2 , as well as the mean platelet volume . The contention that platelet activation plays a pivotal role in orchestrating inflammatory events which trigger, or more likely exacerbate, vascular damage and dysfunction is supported by the steadily increasing recognition of the critical role played by these cells in mediating inflammatory and immune responses .
Telling The Difference Between Dog Congestive Heart Failure And Pneumonia
My dog has an enlarged heart,a murmur and is coughing.An echo and an x-ray were taken in nov 2009 and the cardiologist said her heart is not in congestive failure so no medication was prescribed.She is still coughing but the cough now sounds like she has fluid in her lungs. how do i know if she is now in congestive heart failure or could it be something else like phnemonia? Thanks for your help.
-
By: Erin Broersma El Segundo, CA
Replied on 04/19/2011
If she has an enlarged heart and a murmur, there are medications that help the heart pump more efficiently. I would say if she saw a cardiologist, I would ask them about products such as Enalapril and Digoxin. If she is coughing due to her heart murmur, there are also medications that help open airways and pull fluid from the chest Theophylline, and Lasix . If she has pneumonia, she will be running a fever. She also will not feel well. If she is lethargic and not wanting to eat/drink, I would be concerned that she has pneumonia. It seems more likely, with her medical history, that she may be coughing due to the fact her heart is not working as well as it could be and fluid is forming around her heart and in her lungs. This is a normal side-effect of such a diagnosis and medications tend to alleviate the excess fluid and allow her to breathe much better, while reducing or eliminating the coughing.
Don’t Miss: How To Treat Heart Failure
When Dialysis Is An Option
Recent research suggests that people with advanced heart failure who no longer respond well to diuretics may benefit from a procedure called peritoneal dialysis, which can be done at home. A tube called a catheter is inserted into your abdomen, and a sterile cleansing fluid gets pumped in. Its later drained through the tube, carrying excess fluids out with it. One method requires the procedure be done up to five times a day the other method, which is machine-assisted, works overnight as you sleep.
Dont Miss: Chronic Congestive Heart Failure
Complications Of Heart Failure And Covid
People with heart failure are at a greater risk of becoming severely ill with COVID-19. One study found that among patients who were hospitalized with a COVID-19 infection, there was a 50% mortality rate among those with pre-existing heart failure compared with a mortality rate of 10% in individuals without heart failure.
Treatment for COVID-19 can also lead to serious complications for people with heart failure due to several contributing factors:
- Breathing can be difficult for people with heart failure even without a COVID-19 infection. Fluid can accumulate in the body, particularly in the lungs, since blood that cant be pumped throughout the body causes a backup. This can further reduce the much-needed oxygen supply in people with heart failure. Additionally, COVID-19 usually results in pneumonia and decreased movement of oxygen across the cells in the lung to the bloodstream.
- As COVID-19 and heart failure create difficulty for the body to breathe and pump blood, a persons chances of requiring mechanical ventilation increase. This may seem like the fix. However, especially for people with heart failure, there has been evidence that the high pressure required to support the breathing of people with COVID-19 on mechanical ventilation can further increase pressure in the pulmonary vessels. This creates even greater strainand damageto the heart.
- Severe COVID-19 infection has also been known to cause kidney damage, which can further increase the workload of the heart.
You May Like: Heart Failure Nursing Care Plan
What Is Ejection Fraction
Ejection fraction refers to how well your left ventricle pumps blood with each heart beat. Most times, EF refers to the amount of blood being pumped out of the left ventricle each time it contracts. The left ventricle is the hearts main pumping chamber.
Your EF is expressed as a percentage. An EF that is below normal can be a sign of heart failure. If you have heart failure and a lower-than-normal EF , your EF helps your doctor know how severe your condition is.
Moderate Stage Of Chf
At Stage C, as the heart continues to fail, the person develops weakness and significant fatigue, shortness of breath or palpitations with the slightest physical exertion. She begins to limit activity because of these symptoms as she is only comfortable when resting. A doctors evaluation and testing shows moderate signs of heart dysfunction,
Other possible symptoms might include more visible edema of the lower extremities and the hands might also swell as the fluid congestion in body tissues increases. Shoes and rings might be tighter. The pulse might become weaker because of the struggling heart.
Read Also: What Does A High Resting Heart Rate Mean
Enhancing Healthcare Team Outcomes
The treatment of heart failure and acute decompensated heart failure is challenging despite the use of maximal evidence-based therapy based on the stage of heart failure. Given the limited effect that current treatment strategies have on the progression of heart failure, it is important to identify ways to maximize patient outcomes and quality of care by the interprofessional team.
Patients at potential risk for heart failure based on comorbidities or other identified risk factors should receive appropriate evidence-based preventative counseling and treatments. When appropriate, the primary care providers who may be the most involved in the management of the patients risk factors should consult other specialists, including cardiologists, endocrinologists, pharmacists, cardiology nurses, and nutritionists, to ensure that they are providing the best advice and treatment for their patients. Nurses monitor patients, provide education, and collaborate with the physicians and the rest of the team to improve outcomes. Pharmacists review medications, inform patients and their families about side effects and monitor compliance.
Given the propensity of heart failure patients to require re-current admissions, often because of non-heart failure related conditions, the collaboration between inpatient and outpatient services can be of benefit in the continuity of care and helping promote improved outcomes.
Initial Stages Of Chf
In the initial, mild stage A, there are underlying high-risk factors for CHF such as smoking or high blood pressure. However, the affected person has no symptoms or limitations at rest or with physical activity and there are no signs of CHF on evaluation by a doctor.
In stage B, the person develops mild symptoms of fatigue, shortness of breath, or heart palpitations with routine physical activity. There are minor signs of heart dysfunction on a doctors evaluation. There might also be a mild, intermittent collection of fluid, known as edema, in the ankles and feet.
Recommended Reading: Does Blood Pressure Increase During Heart Attack
What Is The Prognosis And Life Expectancy For Congestive Heart Failure
- The degree to which other organ systems are involved and the severity of other accompanying conditions
- The person’s symptoms and degree of impairment
- Other factors that remain poorly understood
With the availability of newer drugs to potentially favorably affect the progression of the disease, the prognosis in congestive heart failure is generally more favorable than that observed just 10 years ago. In some cases, especially when the heart muscle dysfunction has recently developed, a significant spontaneous improvement is not uncommonly observed, even to the point where heart function becomes normal.
Heart failure is often graded on a scale of I to IV based on the patient’s ability to function.
The prognosis of heart failure patients is very closely associated with the functional class.
An important issue in congestive heart failure is the risk of heart rhythm disturbances . Of those deaths that occur in individuals with congestive heart failure, approximately 50% are related to progressive heart failure. Importantly, the other half are thought to be related to serious arrhythmias.
What Causes Heart Failure
Heart failure can start suddenly after a medical condition or injury damages your heart muscle. But in most cases, heart failure develops slowly from long-term medical conditions.
Conditions that can cause heart failure include:
Recommended Reading: Failure Of The Right Side Of The Heart
