Ii Describe The Advantages And Disadvantages Of This Technique For Diagnosing Congestive Heart Failure
Advantages
- Vascular distribution can indicate increased left-ventricular filling pressure.
- Kerley lines, peribronchial cuffing, and ill-defined vessel margins sugget interstitial edema.
- A batwing pattern of perihilar opacity is demonstrated in alveolar edema.
- Increased vascular pedicle width corresponds to increased systemic blood volume.
- Cardiomegaly can be diagnosed when heart size is > 1/2 the thoracic diameter.
- Simple and cost-effective.
May be difficult in critically ill patients unable to hold their breath and position easily.
Quality Of Patient Care
Brigham and Womens Hospital is committed to providing all of our patients with the safest, highest-quality, most-satisfying care possible and follow established protocols that have been shown to improve patient outcomes. Our inpatient satisfaction survey, sent to patients to assess their total care experience, helps us to monitor what we are doing well and areas for improvement. We pride ourselves in the quality of patient care we provide and how we are measured compared with other hospitals.
V Describe The Advantages And Disadvantages Of The Alternative Techniques For Diagnosing Congestive Heart Failure
Transthoracic echocardiography
- Can determine systolic ejection fraction.
- Can evaluate valvular and left ventricular morphology.
- Quick and easy to perform.
Disadvantages
- Normal echocardiography does not exclude pulmonary edema.
- Poor windows due to body habitus can lead to suboptimal images.
CT with intravenous contrast
- Can show interlobular septal thickening, bronchovascular bundle thickening, and ground-glass opacities, which indicate pulmonary edema.
- ECG gated coronary CT data can calculate ejection fraction accurately.
- May reveal the underlying cause of heart failure, such as valvular disease or CAD.
Disadvantages
- Artifact from pacemakers can obscure anatomy.
- Exposure to ionizing radiation.
You May Like: How To Calculate Heart Rate Zones
Iobenguane Scanning For Cardiac Risk Evaluation
The scintigraphic imaging agent iobenguane I 123 injection is used for the evaluation of myocardial sympathetic innervation in patients with New York Heart Association class 2-3 heart failure with an LVEF of 35% or less. This radionuclide tracer, which functions molecularly as a norepinephrine analogue, can show relative levels of norepinephrine uptake in the cardiac sympathetic nervous system and contribute to risk stratification in heart failure patients. Improved reuptake of norepinephrine is associated with a better prognosis.
What Is The Outlook With Heart Failure
With the right care, congestive heart failure wont stop you from doing the things you enjoy. Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with heart failure have a life span 10 years shorter than those who dont have heart failure. Another study showed that the survival rates of people with chronic heart failure were 80% to 90% for one year, but that dropped to 50% to 60% for year five and down to 30% for 10 years.
A different study found that people who had heart failure and were discharged from the hospital had expected life spans ranging from three to 20 years, depending on various factors like age and gender. Its important to look at your specific situation when considering your prognosis.
Also Check: Signs Of Heart Attacks In Females
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Systolic Hf Prediction Results
The 12-lead ECG data of the 900 HF patients and the 900 individuals without HF were transformed into CWT spectra. The baseline data of individuals with and without systolic HF are listed in Table . Furthermore, Table presents the characteristics of the training, validation, and testing sets. In the testing dataset , the mean LVEF was 32.6±3.4%, and 73 patients had myocardial infarction, 82 had hypertension, and 69 had diabetes. Those values were similar to those in the training dataset . Figure illustrates the original ECG data from the JPG image and the CWT spectra. The CWT spectra can concentrate the unobvious ECG linear features into 2D image, which can enhance specific features of HF for machine learning classification. Also, the tenfold cross validation had been applied to our model, and demonstrated that the V6 had the highest average accuracy of 89.07% .
Table 2 Characteristics of the training, validation, and testing sets.
Don’t Miss: How Many Heart Attacks Can You Have And Live
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
Third And Fourth Heart Sounds
A double apical impulse can represent an auscultated third heart sound . Just as with the displaced point of maximal impulse, a third heart sound is not sensitive for heart failure, but it is highly specific .14 Patients with heart failure and left ventricular hypertrophy can also have a fourth heart sound . The physician should be alert for murmurs, which can provide information about the cause of heart disease and also aid in the selection of therapy.
Read Also: Does Higher Heart Rate Burn More Calories
Heart Failure During Covid
Your heart failure nurse might have been redeployed, making it hard to have in-person appointments or check-ups. ‘The key thing is to look after yourself well, and always phone your GP or heart failure team if your symptoms change or worsen,’ says BHF nurse Lucy Martin. ‘In fact, call your GP or heart failure team if you have any concerns about your medication or care – they are there to help you.’
Your GP is qualified to answer any questions you might have. Dont worry about wasting their time this is exactly what theyre there for.
- Find out more about coronavirus and how it affects people with heart conditions at our coronavirus support hub.
How Long It Lasts
When you first develop AFib, it may come and go. Your irregular heart rhythm may last anywhere from a few seconds to a few weeks. If a thyroid problem, pneumonia, or other treatable illness is behind it, AFib usually goes away once that cause is better.
But for some people, their heart rhythm doesn’t return to normal.
Recommended Reading: Does Heart Failure Go Away
Table Of Cutoff Values
Table 2, below, summarizes the evidence-based cutoff values of BNP and NT-proBNP for ruling in and ruling out the diagnosis of heart failure in the dyspneic patient presenting to the emergency department.
Table 2. Evidence-Based BNP and NT-proBNP Cutoff Values for Diagnosing HF
|
Criterion |
|
|
BNP = B-type natriuretic peptide GRF = glomerular filtration rate HF = heart failure LR = likelihood ratio NPV = negative predictive value NT-pro-BNP = N-terminal proBNP PPV = positive predictive value = not specifically defined. * Derived from Breathing Not Properly data . Derived from PRIDE data . Derived from subset of Breathing Not Properly data . |
BNP and NT-proBNP levels are higher in older patients, women, and patients with renal dysfunction or sepsis. Atrial fibrillation has also been associated with increased BNP levels in the absence of acute heart failure. However, BNP levels may be disproportionately lower in patients who are obese due to fat metabolism or who have hypothyroidism or advanced end-stage heart failure . NT-proBNP plasma levels are also lower in obese heart failure patients relative to nonobese patients with heart failure, regardless of whether the etiology is ischemic or nonischaemic.
Should I Still Call 999 Or Go To Hospital If I’m Worried About My Health
Whether or not you have coronavirus symptoms, it’s essential to dial 999 if you have symptoms that could be a heart attack, or if your heart symptoms get worse.
Dont delay because you think hospitals are too busy the NHS still has systems in place to treat people who need urgent heart treatment. If you delay, you are more likely to suffer serious heart damage and more likely to need intensive care and to spend longer in hospital.
You should dial 999 if you have possible heart attack symptoms or if you are having severe difficulty breathing, such as gasping for breath, choking, lips turning blue, or not being able to get words out. If you feel like youre struggling to manage your condition at home, contact your doctor or NHS 111.
Recommended Reading: What Is The Average Recovery Time For Open Heart Surgery
Can I Improve My Heart Failure Naturally
If your doctor prescribes you medication its important to take it. But making changes to your lifestyle is also going to have a big impact on improving your health.
Changes may include:
- weighing yourself regularly sudden weight gain may mean too much fluid is building up in your body
- watching the amount of fluid you have each day
- limiting how much alcohol you drink
- keeping active this can help improve your energy, stamina and fitness
- keeping to a healthy weight, which will help to prevent your heart from working too hard.
Diet changes are also essential when managing your weight and keeping your heart healthy.
You could feel healthier by eating:
- one or two portions of fruit or veg with every meal
- sunflower oil, olive oil, nuts and avocados instead of saturated fat options like crisps and butter
- one or two portions of beans or pulses everyday with a meal
- your protein in the form of fish, eggs and lean meats
- less salt and sugar.
What Procedures And Tests Diagnose Congestive Heart Failure
Congestive heart failure can be a medical emergency, especially if it acutely decompensates and the patient can present extremely ill with the inability to breathe adequately. In this situation, the ABCs of resuscitation need to be addressed while at the same time, the diagnosis of congestive heart failure is made.
Common tests that are done to help with the diagnosis of congestive heart failure include the following:
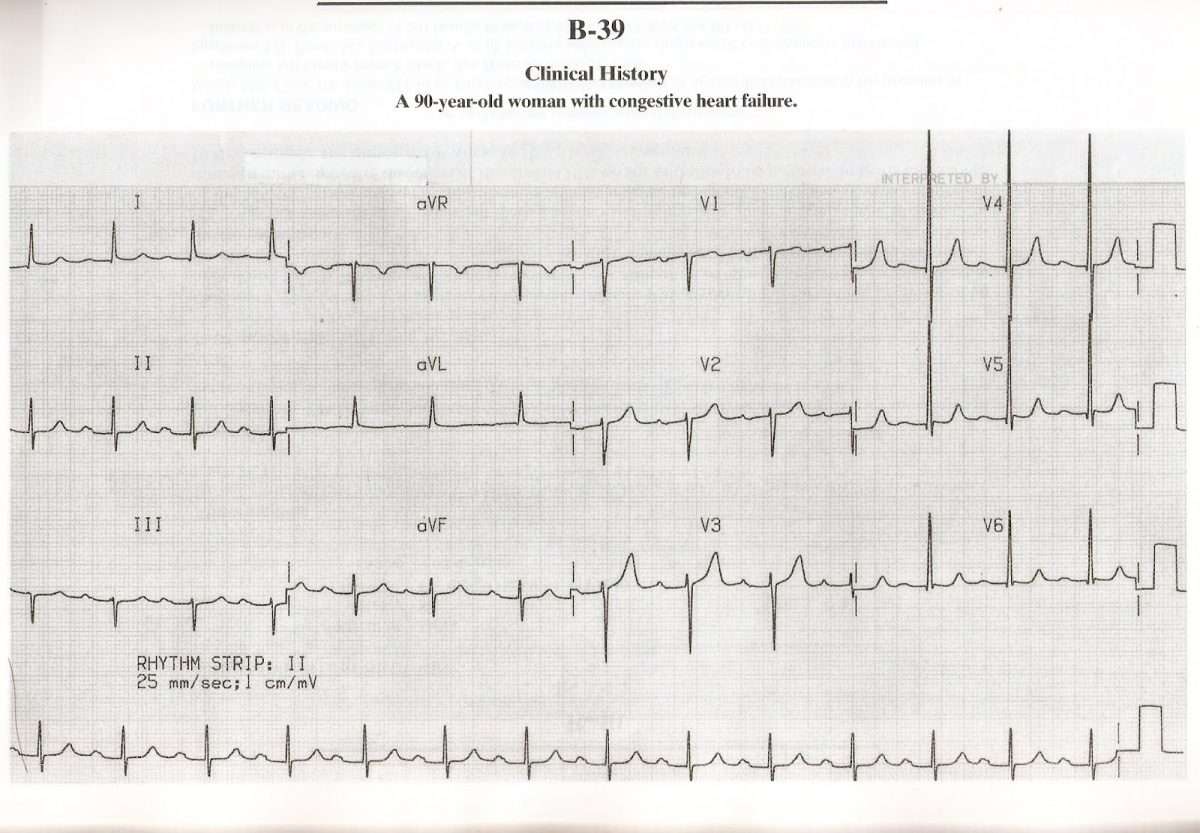
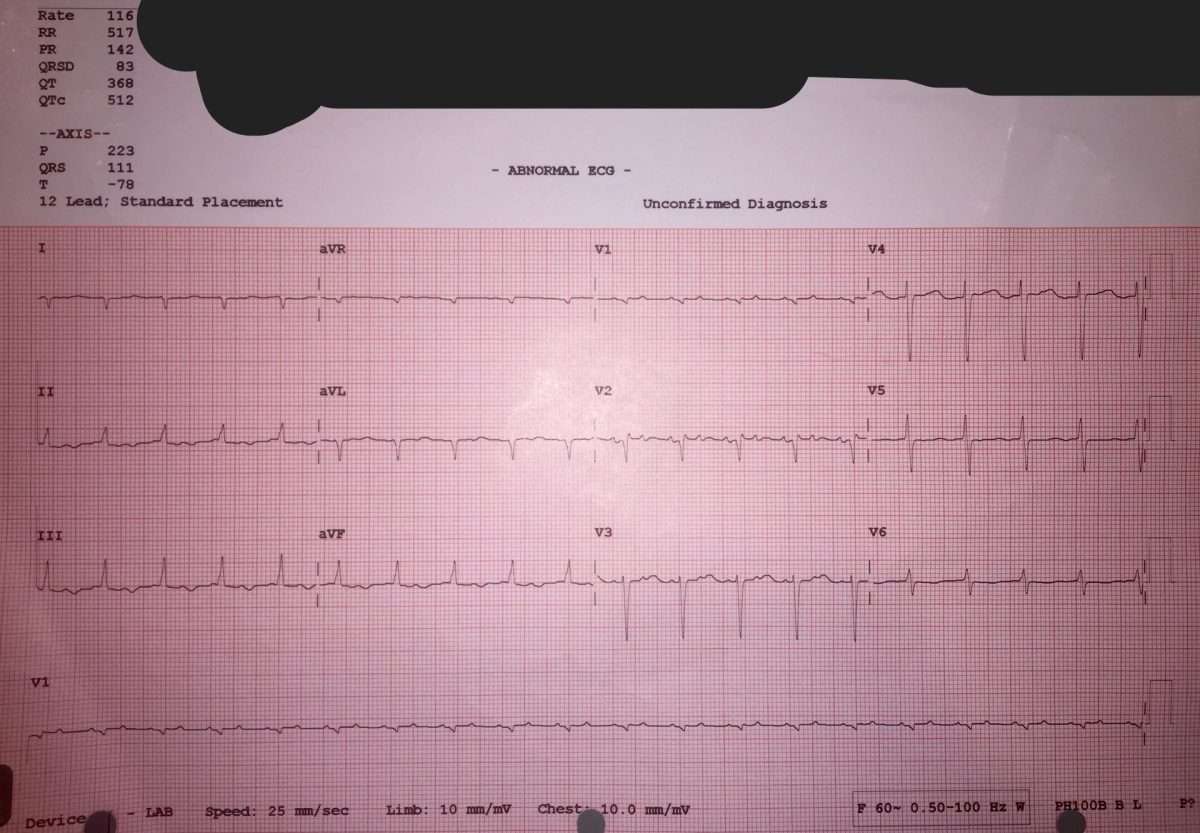
- Electrocardiogram to help assess heart rate, rhythm, and indirectly, the size of the ventricles and blood flow to the heart muscle.
- Blood tests may include a complete blood count , electrolytes, glucose, BUN, and creatinine .
- B-type natriuretic peptide may help decide if a patient has shortness of breath from congestive heart failure or a different cause. It is a chemical that is located in the heart ventricles and may be released when these muscles are overloaded.
- Echocardiography or ultrasound testing of the heart is often recommended to assess the anatomy and the function of the heart. In addition to being able to evaluate the heart valves and muscle, the test can look at blood flow within the heart, watch the chambers of the heart contract, and measure the ejection fraction .
Other tests may be considered to evaluate and monitor a patient with suspected congestive heart failure, depending upon the clinical situation.
Don’t Miss: What Causes Diastolic Heart Failure
What Are The Symptoms Of Heart Failure
The main symptoms of heart failure are:
- Shortness of breath when youre active or resting, because youre not getting enough oxygen.
- Swollen feet, ankles, stomach and around the lower back area, caused by fluid build up.
- Feeling unusually tired or weak because theres not enough blood and oxygen getting to your muscles.
You should see your GP immediately if you begin to experience any of these symptoms.
Bnp Measurement Not Indicated With Nesiritide Therapy
Nesiritide is a synthetic BNP analogue therefore, the measurement of BNP is not indicated in patients who are receiving nesiritide. If BNP is used as a diagnostic marker to rule in heart failure, the level must be determined before nesiritide therapy is started.
In a study by Miller et al, levels of NT-proBNP and BNP decreased in patients with advanced heart failure after therapy with nesiritide, but the majority of the patients did not have biochemically significant decreases in these markers even with a clinical response. The investigators were unable to give a definitive reason for their results, and they indicated that nesiritide therapy should not be guided by the use of levels of both markers. Fitzgerald et al also found decreased levels of both natriuretic peptides following nesiritide therapy in patients with decompensated heart failure.
For more information, see the Medscape Drugs & Diseases article Natriuretic Peptides in Congestive Heart Failure.
Also Check: How To Check For Heart Attack
What Are The Most Common Symptoms Of Congestive Heart Failure
Swelling is the most common symptom of congestive heart failure. Often, swelling is most apparent in the extremities, especially in the legs and ankles, but it can occur in other parts of the body as well. Fluid collection in and around the lungs can cause shortness of breath , especially during physical activity or when lying down. Other common symptoms of heart failure include fatigue, loss of appetite, and weight gain.
What Are The Signs And Symptoms Of Congestive Heart Failure
Shortness of breath
The hallmark and most common symptom of left heart failure is shortness of breath and may occur:
Chest Pain
Right heart failure, left heart failure, or both
Read Also: Can Blood Test Detect Heart Attack
What Are The Treatments For Heart Failure
Treatment of heart failure focuses on slowing or reversing its progression. The earlier treatment starts, the better the outcome.
After a diagnosis, your doctor will recommend a series of lifestyle changes. You may be asked to reach and maintain a healthy weight, increase your activity level , restrict salt intake, restrict fluid intake, and avoid alcohol. If you smoke or chew tobacco, you’ll be advised to stop. You will need to work with your doctor to find the right balance of rest and activity — mobility is important to keep blood circulating. You will also need to weigh yourself daily and record your weight to detect fluid retention.
Your doctor will also prescribe several medications to manage your heart failure or the underlying problem that caused the heart failure. Drugs used to treat heart failure, often in combination, include:
Diuretics or water pills can help reduce symptoms of heart failure or keep them from getting worse. For example, they may help make breathing easier by helping pull fluid out of the lungs. A diuretic makes you urinate a lot, especially when you first start taking it. The diuretics you’re most likely to be started on for heart failure include bumetanide , furosemide , and torsemide .
You may also be given a thiazide diuretic like chlorothiazide or metolazone . Another option is a mineralocorticoid receptor antagonist like eplerenone and spironolactone that not only removes extra salt and fluid but also holds onto potassium.
