Copd Vs Chf: Similarities And Differences
Chronic obstructive pulmonary disease and congestive heart failure can leave you feeling short of breath. These two serious conditions share many symptoms and common risk factors. But the causes and treatments of each are very different.
COPD is a term for several types of serious respiratory conditions that block airflow to the lungs. The two main COPD conditions are chronic bronchitis and emphysema. These diseases leave your lungs unable to work at full strength, making it difficult to breathe.
With bronchitis, the airways that extend from your trachea into your lungs become irritated.
Emphysema occurs when serious damage is done to the tiny air sacs in your lungs where oxygen and carbon dioxide are exchanged.
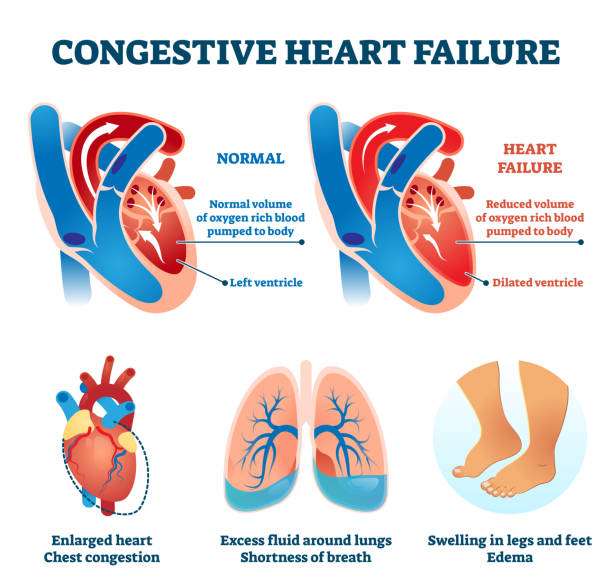
CHF occurs when your heart becomes too weak to pump blood through your body. When blood isnt pumped out of the heart effectively, fluid levels build up or become congested.
When blood backs up or pools in the heart, the heart beats more rapidly and expands to handle the greater volume of blood. This makes heart failure worse.
Similar symptoms
Shortness of breath and wheezing are symptoms of both COPD and CHF. Breathing difficulties are usually experienced after physical activity and tend to develop gradually.
At first, you may notice feeling out of breath after simple activities such as climbing a set of stairs. As COPD and CHF worsen, shortness of breath or wheezing may occur with little physical effort.
Modified Treatment For Combined Copd And Chf
Some medications used for COPD can exacerbate CHF. In COPD, beta-agonists dilate the airways, but they can also impair heart function. In fact, beta-blockers, which actually oppose the action of beta-agonists, are typically used in CHF.
Experts suggest the use of cardioselective beta-blockers for the treatment of CHF in people who also have COPD because these medications specifically target the heart without interfering with lung function.
How Do I Know If I Have Copd And Heart Problems
If you are concerned about COPD and heart problems or if you think you may be experiencing them, it is important to talk to your doctor immediately. Fatal congestive heart failure can strike without warning.
However, multiple types of medication can help control hypertension and other conditions that can lead to heart failure.
If prescription medications fail, surgical procedures can be performed to return heart function. Healthy eating habits, such as a reduced or low sodium diet, eating plenty of fruits and vegetables and consuming lean protein can help you manage symptoms if you have COPD and heart problems as well.
If you have COPD and heart problems, your doctor may ask you to monitor your weight, breathing and appetite to keep track of how youre doing and how well your treatment is working. If you experience increased swelling in your feet, legs or abdomen, it is important to speak with a doctor.
Recommended Reading: What Causes Heart Rate To Drop Suddenly
Congestive Heart Failure Lung Sounds
Congestive heart failure lung sounds
Congestive Heart Failure Lung Sounds. Chest pain that radiates through the upper body. As the disease progresses and the bases fill with fluid, basilar sounds will become diminished or absent with crackles heard in the upper lobes. Swelling in the hands, feet, and. These sounds can also occur if a foreign.
Adventitious Sounds: Types, Diagnosis, When To Seek Help From verywellhealth.com
People with congestive heart failure often have pulmonary edema. This includes asthma, emphysema, pneumonia, acute bronchitis, chronic bronchitis, congestive heart failure, and more. Short of breath, especially when lying. One with pneumonia, one with interstitial pulmonary fibrosis , and one with congestive heart failure . Background although congestive heart failure patients typically present with abnormal auscultatory findings on lung examination, respiratory sounds are not normally subjected to additional analysis. First and second heart sounds normal and unsplit.
Also Check: What Is The Normal Heart Rate Per Minute
Should Patients With Chronic Obstructive Pulmonary Disease Be Screened For Heart Failure
Asymptomatic LVSD fulfils the WilsonJunger criteria for successful screening: the condition is medically important and clearly defined, with effective treatment, an established natural history and early asymptomatic stage, detectable by an acceptable and safe, valid and reliable test applicable to the target population, resulting in cost-effective screening for which adequate resources exist. The predictive value of screening is critically dependent on disease prevalence. The high prevalence of LVSD in patients with COPD thus favours success. Sequential peptide testing and then echocardiography may counter the inherent limitations of peptides or echocardiography alone in pulmonary disease. Robust randomized trials are required to determine the efficacy and cost-effectiveness of such screening. Such a trial is currently being planned.
Also Check: Left Sided Heart Failure Treatment
You May Like: Does Benadryl Lower Heart Rate
Restrictive Pulmonary Function Tests
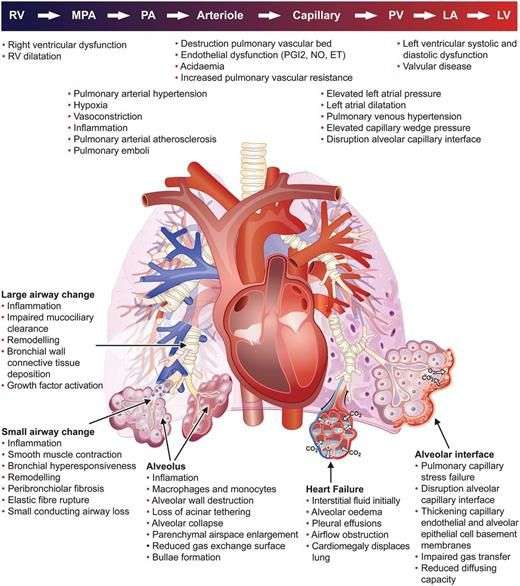
Restrictive ventilatory defects predominate in patients with stable HF.48 FEV1 and FVC were normal or proportionately reduced in a multicentre study of 130 patients.49 Contributory factors include interstitial fibrosis,50 respiratory muscle weakness,45,51,52 cardiomegaly, and pulmonary congestion.53 FEV1 and FVC may also be proportionately reduced with a normal ratio in patients with severe chronic obstructive pulmonary disease and gas trapping. Usually in such cases increased total lung capacity and residual volume help diagnose obstruction.39 However, restricted lung volumes mask hyperinflation and thus the diagnosis of chronic obstructive pulmonary disease in patients with concurrent HF.6
Causes Of Cardiac Coughing
Congestive heart failure causes excess fluid to build up in your body. That adds to your blood volume and can ease the strain on your heart.
When this fluid builds up in the alveoli in your lungs, its called lung congestion. The cardiac cough is your bodys attempt to clear out the fluid.
Causes of lung congestion include:
- Worsening heart failure
- Your prescription heart medication not working as effectively as it should
- Not taking your heart medication as prescribed
- A side effect of angiotensin-converting enzyme inhibitors, a type of medication commonly prescribed for heart failure
The cough from ACE inhibitors tends to be a dry, hacking cough. If its bad enough, you may need to switch to a different heart medication.
If you suspect this side effect, let your healthcare provider know right away. Dont stop taking your heart medication without their approval, even if you think its triggering your cough.
Don’t Miss: Congestive Heart Failure Prevention
Prevalence And Prognosis Of Heart Failure And Chronic Obstructive Pulmonary Disease
The prevalence of GOLD stage II or higher COPD is 510% of adults. One-year mortality in the community is relatively low , but higher following hospitalization ., Future projections have wide uncertainty intervals, depending on statistical methodology, estimates of prevalence, and associated mortality. Nevertheless, the Global Burden of Disease study anticipates COPD to become the third leading cause of death globally by 2020.
Heart failure is less common, affecting 13% of the general population, but carries a worse prognosis. Annual mortality in stable community patients approximates 57%, while median survival following hospitalization remains just 2 years. Approximately half of patients have HF with preserved ejection fraction and half left-ventricular systolic dysfunction . The prevalence of the latter is thus around 1% of the general population.
What Are The Radiological Findings Of Congestive Heart Failure
The radiological tests conducted and their findings are as mentioned below:
Chest X-Ray
A chest X-ray can be used to view both the heart and lungs. The chest X-ray can assess the size of the heart and the fluid accumulation in the lungs.
Based on the progression of CHF, 3 phases have been described, which are as follows:
Phase 1: Vascular Phase
-
This represents the first phase of CHF and signifies pulmonary venous hypertension.
-
Cardiomegaly is evident.
-
Prominent upper pulmonary vessels, in contrast to lower blood vessels, are evident in healthy individuals.
-
Hilar level sees an increase in the artery to bronchus ratio, which appears as white round densities.
-
The pulmonary artery is more prominent in diameter than the bronchi .
-
Hilar haziness and fullness: Pulmonary veins are enlarged, and fluid is seen collecting around the vessels.
-
Vascular redistribution is not seen in supine X-rays .
Phase 2: Interstitial Phase
-
They occur due to interstitial edema and amplified lymphatic drainage.
-
The bronchial wall thickening appears as a white rim around the bronchioles, which appear dark.
-
Thickening of the fissures between the lobes of the lungs.
Phase 3: Alveolar Phase
Computed Tomography
-
CT is not generally recommended to diagnose heart failure. However, it can reveal any congenital or valvular diseases if present.
-
Thickening of the septal lines will be evident.
-
Ground-glass opacity appearance .
Read Also: What Can I Do To Slow My Heart Rate Down
Do You Have Copd Or Congestive Heart Failure Here’s How To Age At Home
COPD and CHF affect many older adults. Both pose significant challenges to those diagnosed and their families, as they require ongoing management. They can lead to various health crises, overall decline, and generally impact your ability to remain safely at home. But, they dont have to…if managed well.
Today, well share a bit more about these conditions and the resources to help. If youve just been diagnosed with COPD or CHF or are struggling with these conditions, we want to reassure you that they can be managed at home. Life can be good again.
Shortness Of Breath From Copd
Similarly to CHF patients, those with COPD will most commonly notice their shortness of breath when physically active. The conditions which cause COPD such as chronic bronchitis and emphysema result in irritation and damage to airways or the air sacs in the lungs where oxygen and carbon dioxide are exchanged. When someone with COPD exhales, this damage prevents oxygen from being fully released before the next breath is drawn in, resulting in shortness of breath.
You May Like: Does Acid Reflux Cause Heart Palpitations
Study Design And Participants
The study used a retrospective cohort study design. Data were retrieved from the Medical Information Mart for Intensive Care III, which is a large, freely-available database comprising deidentified health-related data associated with patients admitted to critical care units of the Beth Israel Deaconess Medical Center between 2001 and 2012.14 This study was exempt from institutional review board approval due to the retrospective design, lack of direct patient intervention, and the security schema for which the reidentification risk was certified as meeting safe harbor standards by Privacert .
All adult patients in the database were included, but for patients who had more than one ICU admission in the database, only the first ICU admission was included. We also excluded patients who stayed in ICU less than 24 hours. Detailed inclusion of the participants is showed in Figure 1.
|
Figure 1 Inclusion of the study subjects. |
Coordinated Congestive Heart Failure Care: Results
With proper aftercare and coordination, CHF patients experience a much lower chance of rehospitalization. Additionally, at-home CHF care enables the elder to live independently longer at home. This results in more years of life and more life in those years. It also typically reduces long-term costs. Caregivers experience less stress as well.
You May Like: What Is The Life Expectancy Of Someone With Congestive Heart Failure
Pulmonary Edema Or Pneumonia
Pulmonary edema can overlap with pneumonia, but it is a different condition. Pneumonia is an infection that often occurs as a complication of a respiratory infection, such as the flu.
It can be difficult to distinguish between the two. If the individual or a family member can provide a detailed medical history, this will make it easier for a physician to make the correct diagnosis and provide the right treatment.
The patient will undergo a physical exam first. The doctor will use a stethoscope to listen to the lungs for crackles and rapid breathing, and the heart for abnormal rhythms.
Blood tests will be carried out to determine blood oxygen levels the doctor will often order other blood tests, including:
- electrolyte levels
- blood counts and blood markers of heart failure
An ultrasound of the heart, an echocardiogram, and an electrocardiogram can help determine the condition of the heart.
A chest X-ray may be used to see whether there is any fluid in or around the lungs and to check the size of the heart. A CT scan of the chest may also be ordered.
Relationship Between Chronic Obstructive Pulmonary Disease And Heart Failure
Chronic obstructive pulmonary disease is characterized by low-grade systemic inflammation, which may contribute to the progression of atherosclerosis and adverse cardiovascular events.9597 Myocardial dysfunction may ensue. In the NHANES III survey, moderate to severe airflow obstruction was associated with elevated inflammatory markers and electrocardiographic ischaemia.95 Reduced FEV1 independently predicts cardiovascular mortality in population studies after adjusting for age, cigarette smoking, hypertension, cholesterol, and obesity.98 A meta-analysis demonstrated an increased relative risk of 1.75 when comparing worst and best FEV1 quintiles.99 However, the multivariable models were often limited, notably lacking adjustment for co-existing diabetes and cardiovascular disease.
Don’t Miss: How To Diagnose Heart Attack
Hospitalisations For Coronary Heart Disease And Heart Failure
Data on hospitalisations were available from the national Danish Patient Registry, until November 2014. The national Danish Patient Registry was established in 1977 and provides complete nationwide registry data without loss to follow-up. Data are available on permission for research purposes from 1977 and forward and the cardiovascular diagnoses have a high specificity and positive predictive value. Denmark used the International Classification of Diseases -8 until 1994 and hereafter shifted directly to ICD-10. Participants with previous admissions for COPD and asthma were removed from the reference group of no respiratory disease. We recorded hospital admissions for coronary heart disease and heart failure , and in our main analysis individuals with previous admissions of coronary heart disease and heart failure were included in the prospective analysis, however, we also performed a sensitivity analysis excluding individuals with previous cardiovascular admissions from our analysis, as described below.
Copd And Chf Often Occur Together
Experts are not entirely sure exactly why people with COPD can also have heart failure. But as mentioned earlier, the lung damage from COPD does place extra stress on the heart. In the end, both conditions result in respiratory symptoms. When they occur together, studies show that the risk of negative outcomes is much increased4
Also Check: Symptoms Woman Having Heart Attack
From Shared Risk Factors To Pathophysiological Mechanisms
Cardiologists readily accept the cardiovascular disease continuum, the hypothesis that frames cardiovascular diseases as a chain of events initiated by risk factors and progressing through numerous physiological pathways to the development of end-stage heart disease and HF. Hopefully in coming years, the concept of a cardiopulmonary continuum, as a common ground of heart and lung disease, will be the basis for future achievements. Interest has grown in the association of chronic pulmonary and cardiac diseases the observation that HF and COPD coexist more frequently than expected from their respective population prevalences being a major reason for this interest. These epidemiological observations encourage new pathophysiological interpretations to understand the connection between the pulmonary and cardiovascular continuum.
Inflammatory pathways involved in the cardiopulmonary continuum. Patients with chronic obstructive pulmonary disease have peripheral lung inflammation. These patients have also increased circulating cytokines, including interleukin – 1b, IL-6, IL-18, and TNFa, as well as acute-phase proteins, such as C-reactive protein and serum amyloid A . This low grade chronic inflammation may represent the link with the increased propensity to cardiovascular, metabolic, bone, neurological diseases as well as the peripheral muscle abnormalities typical of the syndrome .
Recognising And Managing Comorbid Copd And Cvd
Comorbidity in COPD is common and can be fatal. Therefore, in order to treat patients appropriately, physicians should proactively search for prevalent and clinically important comorbidities such as CVD. The three most commonly occurring cardiac comorbidities of COPD are AF, HF and IHD . However, non-specific symptoms such as dyspnoea and fatigue are common to all four diseases and acute exacerbations of each of these conditions can result in exacerbation of respiratory symptoms. Indeed, acute respiratory symptoms invariably have mixed pulmonary and cardiac origin . Diagnosing and managing comorbid COPD and CVD and their exacerbations thus remain challenging .
Read Also: Can Anesthesia Cause Heart Attack
Don’t Miss: What Caused Carrie Fisher’s Heart Attack
Pharmacological Treatment For Hf That Influences Copd Patient Prognosis
Treatment with statins, angiotensin-converting enzyme inhibitors, and angiotensin-receptor blockers can reduce the morbidity and mortality of COPD patients.49,50 Some retrospective studies, such as the one by Mancini et al49 have shown a reduced risk of hospitalization in COPD patients treated with statins who also received treatment with ACE inhibitors and/or ARBs. In fact, in patients with absolute contraindications for -blockers, the association of ACE inhibitors and ARBs could be a treatment option for increasing survival, as shown in a meta-analysis that has evaluated this topic.49 Additionally, Mortensen et al have also reported that the use of statins and ACE inhibitors prior to hospital admission is associated with a decreased mortality in subjects hospitalized for COPD exacerbation.50 Recently, in a prospective study by Bartziokas et al, the use of statins was associated with a low risk of COPD exacerbation and more severe COPD.51 Nonetheless, results from these studies should be cautiously interpreted. We think that new controlled studies to establish their real usefulness are needed. In the meantime, the use of these medications should only be recommended when COPD patients have an associated condition with clear indication.52
Can Heart Failure Be Prevented
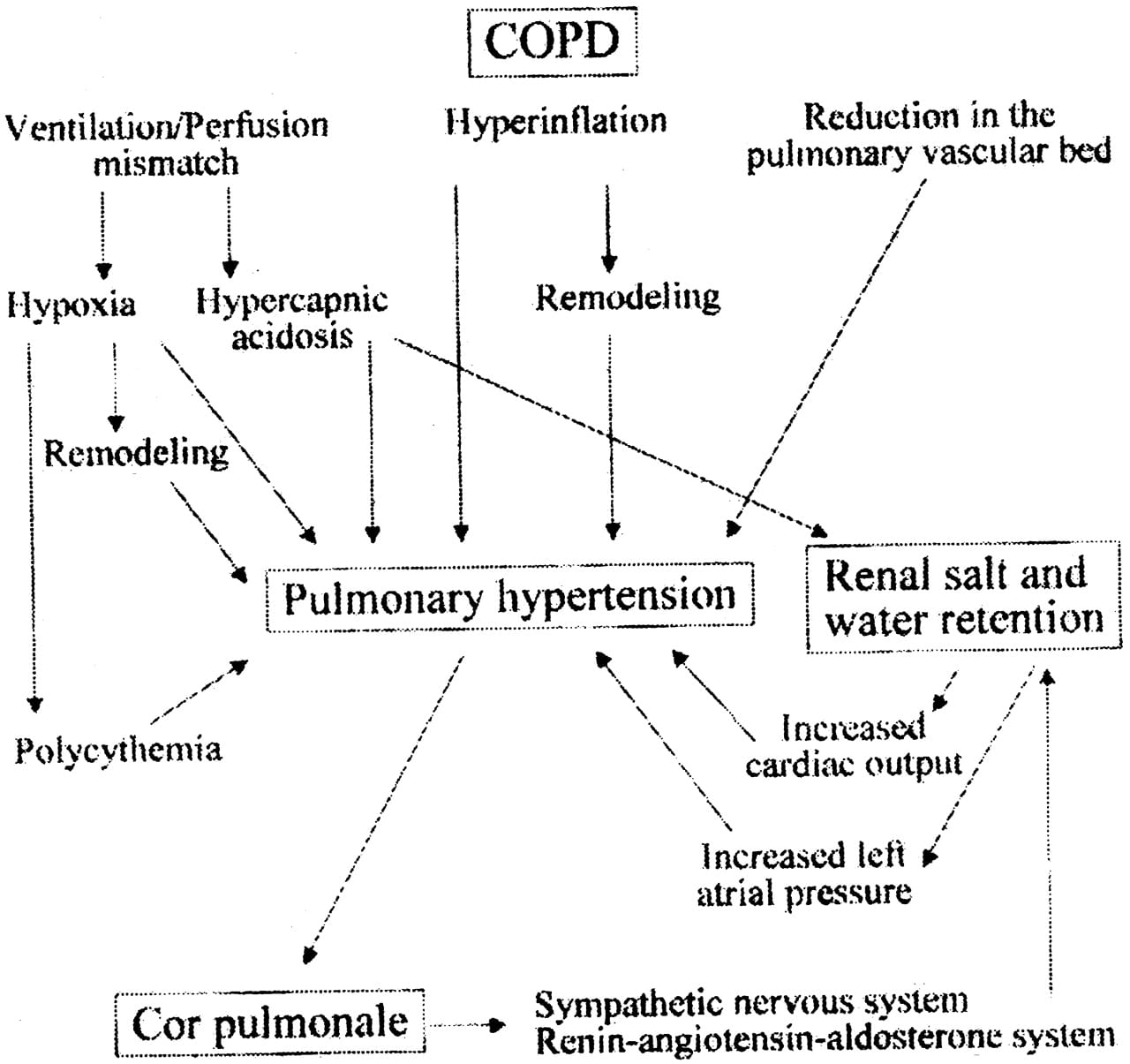
Quitting smoking, and working with your doctor on creating a good COPD treatment regimen can help prevent the progression of COPD. Wearing CPAP at night if you have OSA has been shown to reduce your risk for developing heart failure.4
These are some of the basic theories of how COPD might cause heart failure. In my next post, I will describe the signs and symptoms of heart failure, when to seek help, and what some treatment options are.
To learn more about heart failure signs and symptoms, visit this article: “Heart Failure: Learning the Signs and Symptoms.”
You May Like: Sudden Increase In Heart Rate
