Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Pregnancy
- Nutritional deficiencies
What Are The Types Of Heart Failure
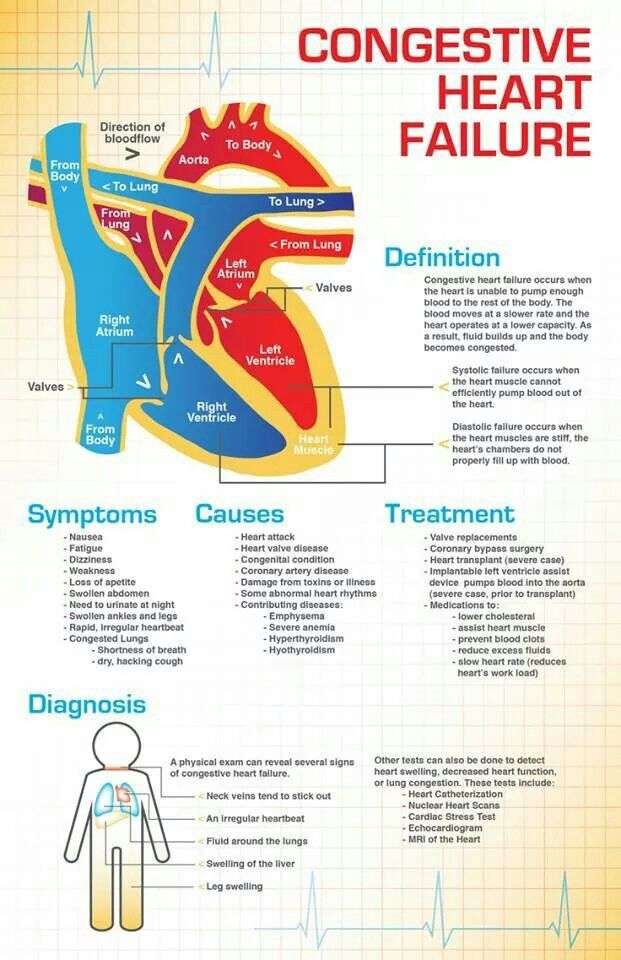
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure
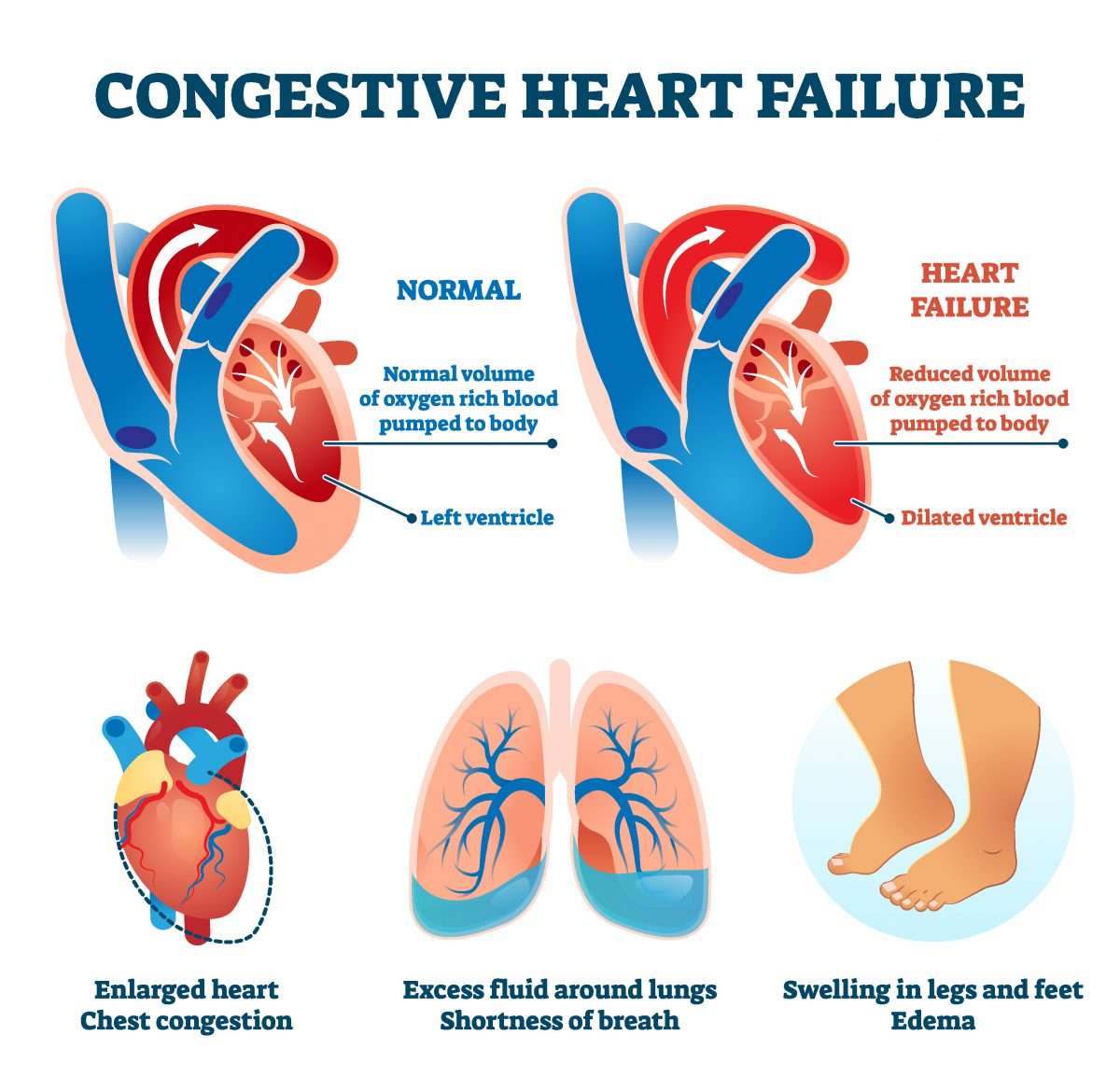
Heart failure with reduced left ventricular function The lower left chamber of your heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of your body.
Heart failure with preserved left ventricular function Your heart contracts and pumps normally, but the bottom chambers of your heart are thicker and stiffer than normal. Because of this, your ventricles can’t relax properly and fill up all the way. Because there’s less blood in your ventricles, your heart pumps out less blood to the rest of your body when it contracts.
Right-sided heart failure
Heart failure can also affect the right side of your heart. Left-sided heart failure is the most common cause of this. Other causes include certain lung problems and issues in other organs.
Myocytes And Myocardial Remodeling
In the failing heart, increased myocardial volume is characterized by larger myocytes approaching the end of their life cycle. As more myocytes drop out, an increased load is placed on the remaining myocardium, and this unfavorable environment is transmitted to the progenitor cells responsible for replacing lost myocytes.
Progenitor cells become progressively less effective as the underlying pathologic process worsens and myocardial failure accelerates. These featuresnamely, the increased myocardial volume and mass, along with a net loss of myocytesare the hallmark of myocardial remodeling. This remodeling process leads to early adaptive mechanisms, such as augmentation of stroke volume and decreased wall stress and, later, to maladaptive mechanisms such as increased myocardial oxygen demand, myocardial ischemia, impaired contractility, and arrhythmogenesis.
As heart failure advances, there is a relative decline in the counterregulatory effects of endogenous vasodilators, including nitric oxide , prostaglandins , bradykinin , atrial natriuretic peptide , and B-type natriuretic peptide . This decline occurs simultaneously with the increase in vasoconstrictor substances from the RAAS and the adrenergic system, which fosters further increases in vasoconstriction and thus preload and afterload. This results in cellular proliferation, adverse myocardial remodeling, and antinatriuresis, with total body fluid excess and worsening of heart failure symptoms.
Recommended Reading: Why Has My Resting Heart Rate Suddenly Dropped
What Medications Should I Avoid If I Have Heart Failure
There are several different types of medications that are best avoided in those with heart failure including:
- Nonsteroidal anti-inflammatory medications such as Motrin or Aleve. For relief of aches, pains, or fever take Tylenol instead.
- Most calcium channel blockers
- Some nutritional supplements, such as salt substitutes, and growth hormone therapies
- Antacids that contain sodium
If youâre taking any of these drugs, discuss them with your doctor.
Itâs important to know the names of your medications, what theyâre used for, and how often and at what times you take them. Keep a list of your medications and bring them with you to each of your doctor visits. Never stop taking your medications without discussing it with your doctor. Even if you have no symptoms, your medications decrease the work of your heart so that it can pump more effectively.
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Don’t Miss: Why Is My Heart Rate Higher On Keto Diet
When To See A Healthcare Provider
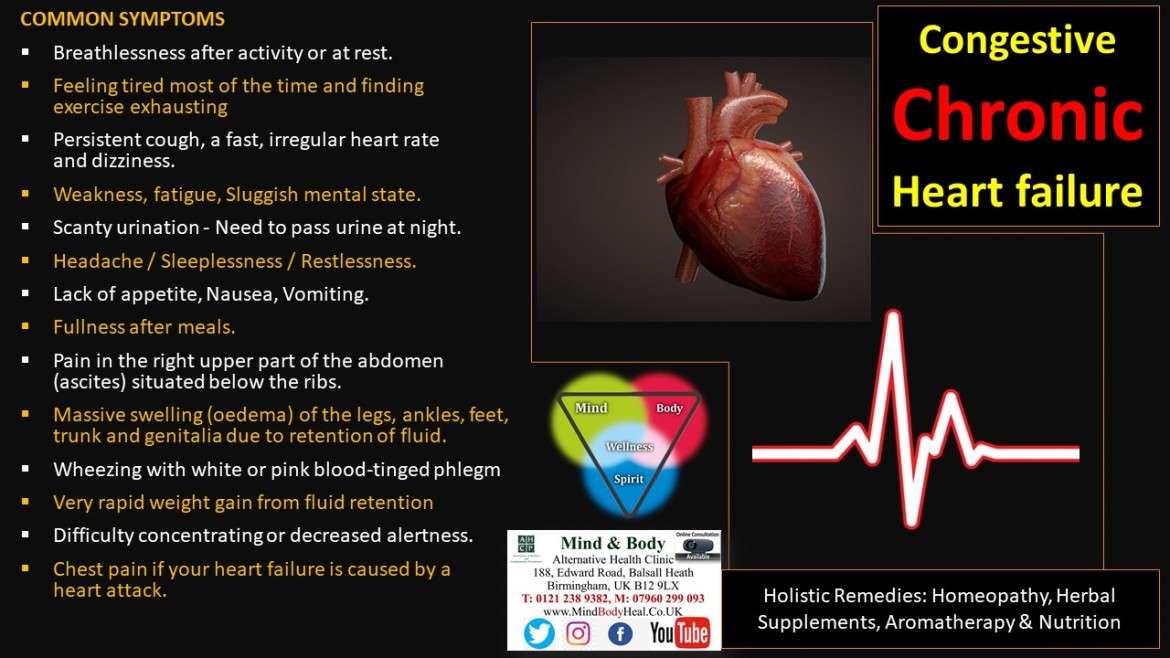
If you are experiencing chest pain, shortness of breath, sudden swelling of the arms or legs, or fatigue on exertion, you may want to get checked by a healthcare professional.
Heart failure and CHF are chronic, progressive conditions that can often be managed with timely treatment, so do not wait to be seen by a healthcare professional if you experience any of the aforementioned symptoms.
How Is Congestive Heart Failure Treated
Doctors will assess the current health status of the patient to establish a baseline, and develop a long-term health plan with the goal of improving the patients health. This may involve the optimization of medicines and therapies, adding new medication, or possibly enrollment in a clinical trial.
Stabilizing and/or reversing a patients condition often involves long-term, collaborative follow-up with a referring cardiologist or physician.
In serious situations, advanced therapies, which include mechanical solutions, a heart transplant, or hospice, may be offered.
Also Check: What Should My Heart Rate Be When Walking
Causes Of Symptoms In Chronic Congestive Heart Failure And Implications For Treatment
The most common symptoms of patients with heart failure are shortness of breath and fatigue. The causes of these symptoms may be different in various entities encompassed by the general term heart failure, such as acute pulmonary edema, circulatory collapse and chronic heart failure. In patients with acute heart failure, shortness of breath is closely related to left atrial pressure. In patients with chronic heart failure, optimally treated with diuretics, the body fluid compartments are usually of normal size. Recent work strongly suggests that, in such patients, central hemodynamic abnormalities are not the sole determinants of symptoms. Impaired vasodilation and altered metabolism in skeletal muscle, circulating metabolites and pulmonary ventilation-perfusion mismatch with consequent increased physiologic dead space may all contribute to the genesis of symptoms. Consequently, it may be possible to alleviate symptoms by treatments that are not aimed directly at improving central hemodynamics. Whether such an approach could also modify prognosis is unknown.
- Previous article in issue
Point Of Maximal Impulse
The point of maximal impulse of the left ventricle is usually located in the midclavicular line at the fifth intercostal space. With the patient in a sitting position, the physician uses fingertips to identify this point. Cardiomegaly usually displaces the cardiac impulse laterally and downward.
At times, the point of maximal impulse may be difficult to locate and therefore loses sensitivity . Yet the location of this point remains a specific indicator for evaluating the size of the heart.14
Also Check: How Blood Pumps Through The Heart
Stage C Treatment Options
Treatment at this stage focuses on managing your symptoms, optimizing your heart function, and preventing worsening of your condition.
Medications to treat stage C heart failure include:
- Diuretics to reduce fluid retention
- Beta blockers to help make your heart work less hard
- SGLT2 inhibitors to reduce the risk of cardiovascular death and hospitalization for heart failure
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Entresto , which reduces the risk of death and hospitalization among patients with chronic heart failure
- Aldosterone antagonists
- Digoxin to help the heart beat stronger and more regularly
- Possible cardiac resynchronization therapy
- Possible implantable cardiac defibrillator therapy
In addition to the lifestyle changes for stages A and B, you may need to make the following changes:
- Reduce your sodium intake
- Restrict fluid intake
- Keep track of your weight daily
Remember that even if the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression of your condition to stage D.
When To Get Medical Advice
See a GP if you experience persistent or gradually worsening symptoms of heart failure.
Call 999 for an ambulance or go to your nearest A& E department as soon as possible if you have sudden or very severe symptoms.
A number of tests can be used to help check how well your heart is working, including blood tests, an ECG and an echocardiogram.
You May Like: Last Stage Congestive Heart Failure
About Congestive Heart Failure
Heart failure, sometimes called congestive cardiac failure , is a condition in which the heart muscle is weakened and cant pump as well as it usually does. The main pumping chambers of the heart can change size and thickness, and either cant contract or cant relax as well as they should. This triggers fluid retention, particularly in the lungs, legs and abdomen.
The major causes of heart failure include coronary heart disease and heart attack, high blood pressure, damage to the heart muscle , heart valve problems and abnormal heart rhythms. Of these, coronary heart disease and heart attack are the most common causes.
The major factors that contribute to coronary heart disease include:
- reduced emotional and social wellbeing
- physical inactivity.
Heart failure is more common in elderly people. The survival rate for people with this disorder depends on the severity of their condition.
Most common treatments for heart failure are medications and self-managed lifestyle changes. Some less-common treatments may require insertion of implantable cardiac devices or valve replacement.
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Recommended Reading: How To Tell If You’re Having A Heart Attack Female
Atrial Natriuretic Peptide And B
ANP and BNP are endogenously generated peptides activated in response to atrial and ventricular volume/pressure expansion. ANP and BNP are released from the atria and ventricles, respectively, and both promote vasodilation and natriuresis. Their hemodynamic effects are mediated by decreases in ventricular filling pressures, owing to reductions in cardiac preload and afterload. BNP, in particular, produces selective afferent arteriolar vasodilation and inhibits sodium reabsorption in the proximal convoluted tubule. It also inhibits renin and aldosterone release and, therefore, adrenergic activation. ANP and BNP are elevated in chronic heart failure. BNP especially has potentially important diagnostic, therapeutic, and prognostic implications.
For more information, see the Medscape Drugs & Diseases article Natriuretic Peptides in Congestive Heart Failure.
How Are Obesity And Heart Disease Related
Obesity affects more than 40% of the U.S. population. The excess fat in obesity was originally thought to be harmless . However, we now know that excess fat causes chemical changes in your blood that increase your heart disease risk. When your fat cells become enlarged, they give off hormones that produce chronic inflammation.
Inflammation can lead to your body no longer using insulin efficiently . This means your body has trouble regulating your blood sugar levels, which can result in metabolic syndrome. Having this condition means you have risk factors that increase your chance of developing heart disease, such as:
How does body shape affect your heart disease risk?
Your risk of heart disease varies based on where your body stores excess fat. People with an apple shape have a higher risk of heart disease than people with a pear shape. Your healthcare provider may measure your waist circumference to understand the degree of abdominal obesity you have as this correlates well with a higher risk of heart disease.
How else can obesity affect your heart?
Increased body fat may also directly contribute to changes in your heart, including:
Obesity also increases your risk of irregular heartbeat . Research shows it may cause one-fifth of all cases of atrial fibrillation . Afib can lead to blood clots that cause stroke.
You May Like: How Does Heart Disease Affect The Skeletal System
How The Normal Heart Works
The normal healthy heart is a strong, muscular pump a little larger than a fist. It pumps blood continuously through the circulatory system.
The heart has four chambers, two on the right and two on the left:
- Two upper chambers called atria
- Two lower chambers called ventricles
The right atrium takes in oxygen-depleted blood from the rest of the body and sends it through the right ventricle where the blood becomes oxygenated in the lungs.
Oxygen-rich blood travels from the lungs to the left atrium, then on to the left ventricle, which pumps it to the rest of the body.
The heart pumps blood to the lungs and to all the bodys tissues through a sequence of highly organized contractions of the four chambers. For the heart to function properly, the four chambers must beat in an organized way.
How Does Heart Failure Affect The Quality Of Life And Lifestyle
With the right care and treatment plan, many adults still enjoy life even though heart failure limits their activities. How well you feel depends on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
This includes caring for yourself by:
- Taking your medications.
- Tracking and reporting new or worsening symptoms to your provider.
- Keeping regular follow-up appointments with your healthcare provider.
Because heart failure is a chronic, long-term illness, talk to your doctor and your family about your preferences for medical care. You can complete an advance directive or living will to let everyone involved in your care know what you want. A living will details the treatments you do or dont want to prolong your life. Its a good idea to prepare a living will while you are well in case you arent able to make these decisions at a later time.
A note from Cleveland Clinic
If you have heart failure, you can take steps to improve your heart health. Take your medications as instructed, follow a low-sodium diet, stay active or become physically active, take notice of sudden changes in your weight, live a healthy lifestyle, keep your follow-up appointments and track your symptoms. Talk to your healthcare provider about questions or concerns you have about your medications, lifestyle changes or any other part of your treatment plan.
References
Also Check: Why Does My Heart Palpitate When I Lay Down
Heart Failure With Preserved Ejection Fraction
In heart failure with preserved ejection fraction , formerly known as diastolic heart failure, the left side of the heart retains its ability to pump but the stiffening of the heart muscle does not allow it to relax during beats.
Losing the ability to relax during beats means that the left ventricle chamber loses its capacity to adequately fill with blood, so when it pumps, less blood is pushed out.
What Is The Prognosis For Children With Congenital Heart Defects
The prognosis depends on the defect. In many cases, children with congenital heart defects go on to live normal lives. In most cases, people with heart defects are at greater risk for developing infection of the heart and valves. They may need to take antibiotics when having certain dental or surgical procedures in order to prevent endocarditis, an infection of the hearts lining.
You May Like: Prognosis Of Congestive Heart Failure
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
What Are The Common Types Of Pediatric Congenital Heart Defects
A septal defect is a hole in the septum, the wall that divides the heart. There are 2 types of septal defects: atrial septal defects are holes in the septum between the left and the right atria ventricular septal defects are holes in the septum between the left and right ventricles. Because of this hole, oxygenated blood mixes with non-oxygenated blood.
A septal defect means that blood flows from one chamber of the heart to the other, instead of taking its normal path. For instance, with an atrial septal defect, blood flows from one atrium to the other, instead of going to the ventricle.
Similarly, with a VSD, the blood flows from the left ventricle to the right ventricle, rather than through its normal path to the aorta and the rest of the body. As a result, blood that has picked up oxygen from the lungs mixes with oxygen-poor blood. This can mean that parts of the body arent getting enough oxygenated blood.
ASDs and VSDs can be small or large. Some ASDs close up on their own as the child grows older. Others may be repaired using catheters or with open heart surgery.
Although some small VSDs may close on their own, some are so large that the left side of the heart is forced to work much harder. If it is not treated, a VSD can lead to heart failure. These defects have to be repaired with open heart surgery.
Valve defects
Another type of defect involves the heart valves. Defective valves may be caused by:
Other types of congenital heart defects
Don’t Miss: How To Tell If You’re Having A Heart Attack
